Abstract
Objective
In the pediatric population the skull has not yet undergone ossification and it is assumed that the diagnostic rate of skull fractures by simple X-rays are lower than that of adults. It has been recently proposed that the diagnostic rates of skull fractures by 3-dimensional computer tomography (3D-CT) are higher than simple X-rays. The authors therefore attempted to compare the diagnostic rates of pediatric skull fractures by simple X-rays and 3D-CTs with respect to the type of fracture.
Methods
One-hundred patients aged less than 12 years who visited the Emergency Center for cranial injury were subject to simple X-rays and 3D-CTs. The type and location of the fractures were compared and Kappa statistical analysis and the t-test were conducted.
Results
Among the 100 pediatric patients, 65 were male and 35 were female. The mean age was 50±45 months. 63 patients had simple skull fractures and 22 had complex fractures, and the types of fractures were linear fractures in 74, diastatic fractures 15, depressed fractures in 10, penetrating fracture in 1, and greenstick fractures in 3 patients. Statistical difference was observed for the predictive value of simple skull fractures' diagnostic rate depending on the method for diagnosis. A significant difference of the Kappa value was noted in the diagnosis of depressed skull fractures and diastatic skull fractures.
Skull fractures are known to be the most common underlying etiology of death among the various types of pediatric injuries. Every year 1500000 children are afflicted with skull fractures in the United States, 1200000 children visit the emergency services, 250000 are admitted, and among them 50000 die from this injury7,14). While skull fractures in children are common, there is disagreement among medical institutions with regard to the diagnostic method. Although the simple skull X-rays are regarded as the most basic imaging tool in patients with skull fractures, there exists debate regarding the exact role in the diagnosis of skull fractures4,9,16). This is assumed to be due to the fact that in the pediatric population the skull has not yet undergone ossification and it is therefore the diagnostic rates of skull fractures by simple X-rays seem to be lower compared to adults11). While the diagnosis of the fracture itself is not clinically more important than intracranial hemorrhage, contusion, or ischemia, other events that accompany skull fractures such hemorrhaging, CSF leakage, neurovascular injury, meningitis, cranial nerve palsy, carotid artery dissection, and carotid-cavernous fistula may be present, as well as legal compensation issues13,15).
Recent advances in the high resolution image reconstruction of 3-dimensional computer tomography (3D-CT) has led to marked improvement of skull fracture diagnosis rates, and hence there is widespread opinion that the diagnostic rates of skull fractures by 3D-CT is far superior to that of simple X-rays, from newborn to infants. In addition, there are reports that site-specific skull fractures or depression skull fractures are related to intracranial injury, and therefore the application of 3D-CT in all cases of skull fractures have been suggested4,13). However, as the ionizing radiation dose of 3D-CT is several hundred-fold greater than simple X-rays, there have been concerns for potential carcinogenesis after long term exposure as well as for the increased cost and complexities should all simple X-rays be replaced by 3D-CT1,6). The authors of this study attempted to compare the diagnostic rates of simple X-rays and 3D-CT in patients with pediatric skull fractures according to the different types of fracture so as to establish the clinical roles of the above two imaging modalities in the evaluation of pediatric head injuries.
For a period of 40 months from January 1st, 2007 to April 30, 2010, 100 pediatric patients aged less than 12 years who visited the our emergency center for cranial injury were subject to simple X-rays and 3D-CT. Skull disease-related fractures, and those pathologic fractures due to tumors or metastatic tumor were excluded from the present study.
Skull fractures were analyzed with respect to the complexity, type, location, accompanying lesions, and treatment methods after simple X-rays and 3D-CT. The type of fracture was compared by 2 independent observers for diagnostic rates and interobserver agreement.
Kappa statistical analysis was employed to determine statistical significance of interobserver agreement between observers, and the t-test assessed the statistical significance of the diagnostic rates17).
Kappa values were divided into 0.2 intervals from 0.0 to 1.0, and each interval was interpreted as poot, slight fair, moderate, substantial, and almost perfect.
Among the 100 head injury patients, 65 were male and 35 were female. The mean age was 50±45 months and ranged from 0-2 years (n=42), 3-6 years (n=25), and 7-14 years (n=33).
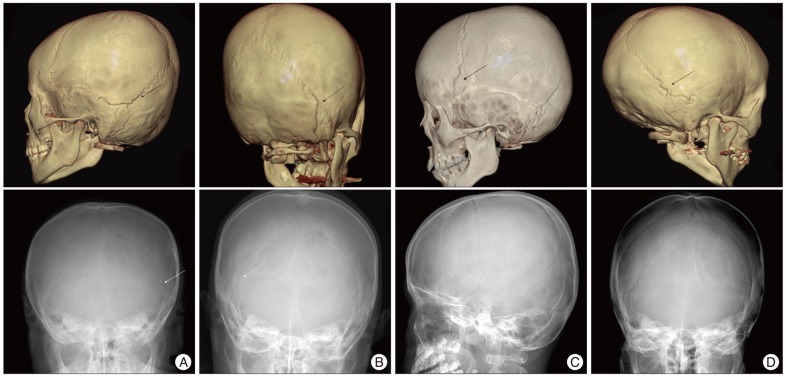
Simple skull fractures were observed in 63 patients, complex skull fractures in 22, and the types of fractures found were linear fracture in 74 patients (Fig. 1), depression fractures in 10 (Fig. 2), diastatic fractures in 15 (Fig. 3), penetrating fracture in 1, and a greenstick fracture in 3 patients. Fractures were most common in the parietal area (n=32), followed by the occipital in 22, frontal in 13, and temporal area in 1 patient. Fractures involving more than one site were observed in 16 patients, and was the most common in the parieto-occipital skull (n=8), with 2 cases in the fronto-parietal, and temporo-parietal skull, and 1 case each of the both parietal, fronto-occipital, fronto-temporal, and temporo-parieto-occipital skull. The most common diastatic fracture type was the occipito-mastoid suture (n=6), followed by fractures of the coronal suture in 3, lambdoidal suture in 2, and temporo-parietal suture, temporo-parieto-lambdoidal suture, metopic suture, and temoro-parieto-lamdboido-metopic suture in 1 each, respectively.
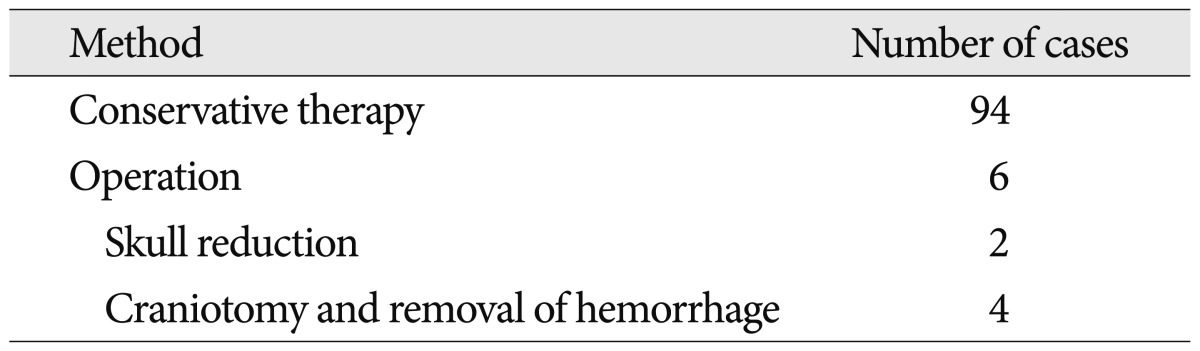
The most common comorbidity was scalp hemorrhage which number 90, and there were 28 cases of epidural hemorrhage, 14 cases of pneumocephalus, 3 patients who experienced subarachnoid hemorrhage, 2 patients with subdural hemorrhage, 2 who suffered intracerebral hemorrhage, and 1 child with sinus thrombosis. Among the 100 patients with head injuries, 94 were treated conservatively while 6 received surgery. The surgery group comprised of 4 patients who underwent open craniotomy and hematoma removal, all with diastatic fractures. Three of these surgery patients were accompanied by epidural hemorrhage, while 1 patient had both epidural hemorrhage and subdural hemorrhage simultaneously. Two patients received simple skull reduction only for depression (Table 1).
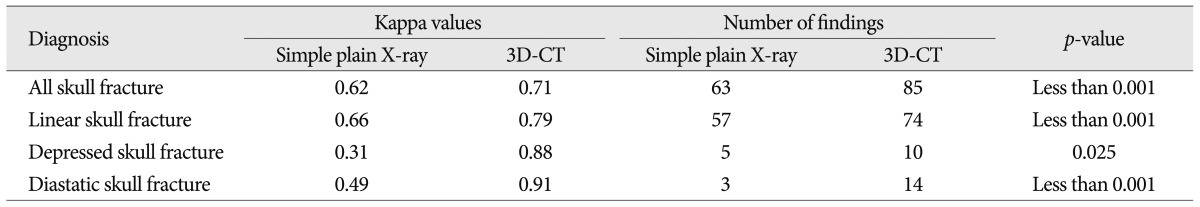
Skull fractures were observed in 63 patients by simple X-rays while 85 cases were found by 3D-CT (p<0.001), and the calculated Kappa values were 0.57 and 0.71 respectively, showing that the predictive rate of 3D-CT was higher than simple X-rays, but did not show significantly higher interobserver agreement between observers. Linear skull fractures were demonstrated in 57 and 74 patients by simple X-ray and 3D-CT, respectively (p<0.001), and the respective Kappa values were 0.66 and 0.79 the diagnostic rate of 3D-CT was higher than simple X-rays but did not show significantly higher interobserver agreement between observers. In comparison, depression skull fractures were detected by simple X-rays in 5 cases while 3D-CT diagnosed 10 such fractures (p=0.025), and the calculated Kappa values were 0.31 and 0.88, respectively. This demonstrated a significant difference which suggests that 3D-CT has a higher predictive rate compared to simple X-ray and also a very high interobserver agreement. Diastatic skull fractures were diagnosed by simple X-rays and 3D-CT in 3 and 14 patients, respectively (p<0.001), and the respective Kappa values of 0.49 and 0.91 showed that 3D-CT has a higher predictive rate compared to simple X-ray and also a very high interobserver agreement.
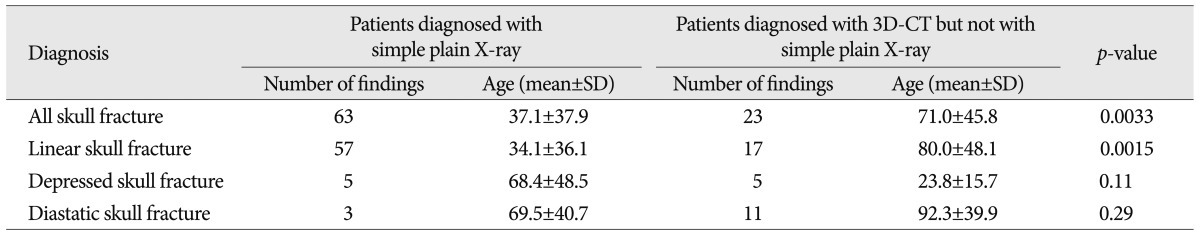
Comparison of the age of the patient who had and who had not been diagnosed with a skull fracture by simple skull X-ray but confirmed to be with fracture by 3D-CT showed that in all fractures, the mean age of 63 patients diagnosed by simple X-ray was 37.1±37.9 months, and 71.0±45.8 months in 23 patients diagnosed by 3D-CT but not by simple X-rays, and which was statistically significant (p=0.0033). Similarly, the mean age of the 57 patients with simple fracture who were diagnosed by simple X-ray was 34.1±36.1 months, and 80.0±48.1 months in the 17 patients who were diagnosed by 3D-CT but not by simple X-ray, and this was statistically significant (p=0.0015). However, the mean age of the 5 patients with depression fractures diagnosed by simple X-ray was 68.4±48.5 months, and the age of the 5 patients diagnosed by 3D-CT but not by simple X-ray was 23.8±15.7 months, and this was not statistically different (p=0.11). Also, the mean age of the 3 diastatic fracture cases who were diagnosed by simple X-rays was 69.5±40.7 months, and was not statistically different from the 92.3±39.9 months of the 11 cases diagnosed by 3D-CT but not by simple X-rays (p=0.29).
The simple X-ray is one of the most basic diagnostic tools for evaluating skull fracture that result from head injury but its pivotal role is not yet established5,7,14,16). In spite of simple X-rays having simplicity in performance, relatively safe radiation exposure and possibility of detecting other accompanying fractures, the immature sclerosis of the younger aged children leads to decreased diagnostic rates of skull fractures compared to adult fractures11), and following the development of the multi-planner high-resolution 3D-CT, it has been suggested that conducting 3D-CT only is more faster and accurate than simple X-rays.
Nelson et al.10) reported that in a study of 1097 patients with skull fractures, 53% were simple fractures, 16% were depression fractures, 12% were of the compound fracture type and 19% were basal skull fractures. It was also noted in the same report that the incidence of skull fractures were 44.3 per 100000 persons each year, and was slightly higher among the urban population compared to the rural areas. The incidence of skull fractures was the highest among the youngest aged according to age, the simple linear fracture type being the most common, with a male to female ratio ranging from 2.1 : 1 to 4.5 : 1 according to the type of fracture. In our study population, we also observed that there were more males than females and that fractures were the most common in the 0-2 year old age group.
In the present series, simple fractures comprised 63% of the total head injury patients. This was followed by 22 patients with complex or compound fractures and linear fractures being the most common in 74 patients. We observed that there were diastatic fractures in 15% of our patients which is a relatively higher number than previously reported numbers and also a number of skull greenstick fractures that were discovered probably due to the routine implementation of 3D-CT when fractures were suspected. In a large investigation by Quayle et al.12), it was shown that among 322 children with head injuries, intracranial injury was present in 8% of the patients and skull fractures in 16%. Surgery was performed in 10 patients which comprised of 5 depression fracture reconstructions, 4 extraventricular drainage catheter insertions, and 1 patient in which surgery for removal of an intracerebral hematoma was conducted. When Quayle et al.'s results12) are compared to this study, it can be seen that the numbers of fractures and surgery of the above mentioned author are far less than ours, and this is attributable to our selection of only those children who received both skull simple X-rays and 3D-CT and excluded those simple head injury patients who underwent only simple X-ray or 2 dimensional computed tomography (2D-CT). Moreover, as the radiation exposure is greater with 3D-CT compared to 2D-CT, it cannot exclude the possibility that 3D-CT was implemented in more severe head injury patient.
The parietal and occipital locations were the most common sites of skull fracture, and since it is known that injuries to the occipital area entails greater accompanying intracranial injury than the frontal area, it may be supposed that patients with more severe injuries than the general head injury population may be included in this study. We would like to draw attention to the 10 lambdoidal suture fractures out of 15 cases of diastatic fractures that included the occipito-mastoid sutured and the lambdoid suture of the posterior suture, which was greater number than the coronal suture fractures.
Another point of interest is that the proportion of accompanying cephalhematoma lesions was 90% among the 100 patients showing that the majority of pediatric head injury patients are unable to present their symptoms, and also the relatively higher 28% of patients with epidural hemorrhage compared to other investigations also infers that our selection of head injury patients were of a more serious nature than general head injury patients. The detection of the sole case of traumatic sinus thrombosis that has been absent in the previous literature is probably due to routine cautionary measures for sinus thrombosis such as testing for the D-dimer marker in all head injury patients, and we therefore suggest that the possibility of a sinus thrombosis should be kept in mind in all cases of pediatric head injury.
According to the report by Quayle et al.12), 8 among 322 head injury patients were diagnosed with linear skull fracture by a simple X-ray but not by brain CT. Conversely, 2 patients were diagnosed by brain CT but not by a simple X-ray, implying that the 2D-CT may detect fractures that were not diagnosed by simple X-rays. In a recent study by Connor and Flis3), the 3-D multiplanar high resolution computed tomography (HRCT) was able to diagnose basal skull fractures that were not detected by 5 mm interval axial CT, and it was suggested by the author that 3-D multiplanar HRCT plays a prominent role, and especially that at least a 3D-CT should be performed when evaluating patients with suspected basal skull fractures. A similar conclusion was arrived at by Ringl et al.13) who stressed the role of 3D-CTs in the diagnosis of basal skull fractures and that among the types of 3D-CT the Maximum Intensity Projection imaging and high-resolution multiplanar reformation provides the highest diagnostic predictive value. Therefore, at the present time, various modes of 3-D imaging, including 3-D high resolution techniques are acknowledged as diagnostic tools with the highest accuracy in detecting basal skull fractures. This is again reflected by the results in the series by Ringl et al.13), who demonstrated that the accuracy of basal skull fracture diagnosis by 3D-CT was 80-87% which was significantly higher than the 43-70% of axial CTs13), which is because the 3D-CT is able to distinguish well between diagnosis errors such as vascular groove and fractures. The importance of the role of 3D-CT in the diagnosis of not only skull base fractures but also those of the occiput has been proposed by Choudhary et al.2). The suture lines of the occiput skull are complex and the 3D-CT is able to distinguish clearly these sutures from lambdoidal diastatic fractures. The occiput begins by fusion of the posterior intraoccipital synchondrosis at 2 years of age and is completed by age 6 years. The anterior intraoccipital synchondrosis begins fusion at 2 years but fusion is completed at 7-10 years of age2). The petro-occipital synchondrosis is fused at age 16, and the occipito-mastoid sutures should be fused by age 228), and therefore since there are frequent variations of the suturelines itself, it seems that extended employment of the occipital 3D-CT is a likelihood event.
Until now, as there is a paucity of data pertaining to the role of 3D-CT in the diagnosis of depression fractures or diastatic fractures, it is difficult to compare with simple X-rays in the accurate diagnosis of skull fractures. In the present study we were able to observe that not only the predictive value but also the Kappa values showed that 3D-CT were superior to simple X-ray in the diagnosis of skull fractures, and also that in the future the employment of 3D-CT may be extended to the evaluation of depression fractures or diastatic fractures. One surprising fact that emerged from our study was that among the 15 cases of diastatic fractures, 9 were accompanied by intracerebral hemorrhage, among whom 4 received evacuation of hematoma via surgery. This interprets to 4 out of 100 pediatric head injury patients who received surgery for parenchymal hemorrhage who all had diastatic fractures, which suggests that the importance of diastatic fractures should be addressed in future large scale studies.
The authors of this current study were able to confirm the statistical significance of the diagnostic predictive value of 3D-CT in patients with simple linear fractures that has not been yet described in the previous literature, and present the new observation that the predictive value is not limited to those younger pediatric patients whose skull ossification is not yet completed such that diagnosis of fracture lesions are difficult by simple X-rays, but also applicable to older children of over 6 years of age in whom 3D-CT may provide a high accuracy of linear fracture diagnosis. Although the legal significance of simple linear fractures may be of interest, the clinical aspects such as treatment and prognosis of children are as yet undetermined. It is true that 3D-CT results in 10-100 fold greater radiation exposure to patients than simple X-ray, and therefore there are limitations in extending the indications for 3D-CT which may entail the possibility of radiation exposure carcinogenesis1,5). If advances in technology provide a 3D-CT with substantial decreased radiation exposure, then the breadth of the clinical applications will be widened.
We attempted to compare difference in diagnostic rates of pediatric skull fractures by simple X-rays and 3D-CTs, and unexpectedly found that simple X-rays were unable to make a diagnosis in older aged children but by 3D-CT. This may possibly be due to incorrect or inaccurate X-ray imaging procedure, or mild diastatic fracture may have been overlooked, or linear fractures not occurring in full thickness of the skull but only in its outer layer that it could not be detected by simple X-rays. A larger scale with larger cohort of study patients is required to clarify this issue.
References
1. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007; 357:2277–2284. PMID: 18046031.

2. Choudhary AK, Jha B, Boal DK, Dias M. Occipital sutures and its variations : the value of 3D-CT and how to differentiate it from fractures using 3D-CT? Surg Radiol Anat. 2010; 32:807–816. PMID: 20174986.

3. Connor SE, Flis C. The contribution of high-resolution multiplanar reformats of the skull base to the detection of skull-base fractures. Clin Radiol. 2005; 60:878–885. PMID: 16039923.

4. Da Dalt L, Marchi AG, Laudizi L, Crichiutti G, Messi G, Pavanello L, et al. Predictors of intracranial injuries in children after blunt head trauma. Eur J Pediatr. 2006; 165:142–148. PMID: 16311740.

5. Di Scala C, Osberg JS, Gans BM, Chin LJ, Grant CC. Children with traumatic head injury : morbidity and postacute treatment. Arch Phys Med Rehabil. 1991; 72:662–666. PMID: 1830468.
6. Gogos KA, Yakoumakis EN, Tsalafoutas IA, Makri TK. Radiation dose considerations in common paediatric X-ray examinations. Pediatr Radiol. 2003; 33:236–240. PMID: 12709751.

7. Jaffe D, Wesson D. Emergency management of blunt trauma in children. N Engl J Med. 1991; 324:1477–1482. PMID: 2023607.

8. Madeline LA, Elster AD. Suture closure in the human chondrocranium : CT assessment. Radiology. 1995; 196:747–756. PMID: 7644639.

9. Mann SS, Naidich TP, Towbin RB, Doundoulakis SH. Imaging of postnatal maturation of the skull base. Neuroimaging Clin N Am. 2000; 10:1–21. viiPMID: 10658152.
10. Nelson EL, Melton LJ 3rd, Annegers JF, Laws ER, Offord KP. Incidence of skull fractures in Olmsted County, Minnesota. Neurosurgery. 1984; 15:318–324. PMID: 6332998.

11. Oh CK, Yoon SH. The significance of incomplete skull fracture in the birth injury. Med Hypotheses. 2010; 74:898–900. PMID: 20005051.

12. Quayle KS, Jaffe DM, Kuppermann N, Kaufman BA, Lee BC, Park TS, et al. Diagnostic testing for acute head injury in children : when are head computed tomography and skull radiographs indicated? Pediatrics. 1997; 99:E11. PMID: 9113968.
13. Ringl H, Schernthaner RE, Schueller G, Balassy C, Kienzl D, Botosaneanu A, et al. The skull unfolded : a cranial CT visualization algorithm for fast and easy detection of skull fractures. Radiology. 2010; 255:553–562. PMID: 20332373.

14. Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006; 21:544–548. PMID: 17122685.

15. Samii M, Tatagiba M. Skull base trauma : diagnosis and management. Neurol Res. 2002; 24:147–156. PMID: 11877898.
16. Teasdale GM, Murray G, Anderson E, Mendelow AD, MacMillan R, Jennett B, et al. Risks of acute traumatic intracranial haematoma in children and adults : implications for managing head injuries. BMJ. 1990; 300:363–367. PMID: 2106986.

17. Viera AJ, Garrett JM. Understanding interobserver agreement : the kappa statistic. Fam Med. 2005; 37:360–363. PMID: 15883903.
Fig. 1
Linear skull fracture in the simple X-ray and 3 dimensional computed tomography. Linear skull fractures on the occipital bone (A and B) and parietal bone (C) show not in the simple X-ray but clearly in the 3 dimensional computed tomography.
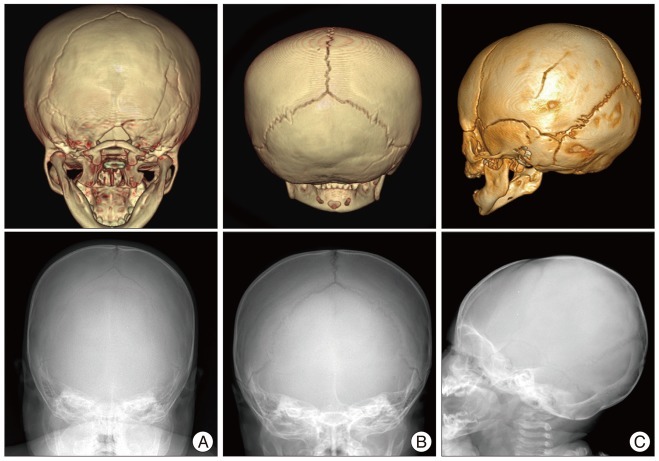
Fig. 2
Depressed skull fracture in the simple X-ray and 3 dimensional computed tomography. A : Depressed skull fracture on the parietal bone shows clearly both in the simple X-ray and 3 dimensional computed tomography. B and C : Depressed skull fracture on the outer table of the parietal bone shows not in the simple X-ray but clearly in the 3 dimensional computed tomography.
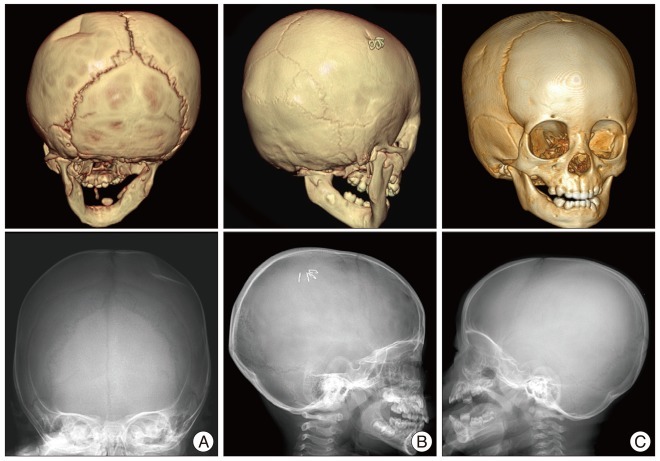
Fig. 3
Diastatic skull fractures in the simple X-ray and 3 dimensional computed tomography. A and B : Diastatic skull fractures on the lambdoid, temporo-parietal and occipito-mastoid sutures show clearly both in the simple X-ray and 3 dimensional computed tomography. C and D : Diastatic skull fractures on the coronal, lambdoid, and temporo-parietal sutures show not in the simple X-ray but clearly in the 3 dimensional computed tomography. Arrows indicate site of fracture in each pictures.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download