Abstract
Behçet's disease (BD) is an inflammatory systemic disorder with oral and genital ulcers, as well as ophthalmologic and cutaneous symptoms. Neurological manifestations in BD represent between 2.2% to 50% of the cases. The 25-year-old male patient, diagnosed with BD three years earlier, was admitted to our clinic with complaints of recurrent headaches. Tumor-like-parenchimal involvement was detected on a cranial magnetic resonance imaging. The lesion was removed surgically and then he suffered from right hemiparesis and epilepsy. Pathological examination of the lesion noted a demyelinating non-tumoural etiology. A neuro-Behğet's case with parenchymal involvement has been examined in light of the literature, in terms of a tumor and a demyelinating disease differential diagnosis.
Go to : 
Behçet's disease (BD) is a heterogeneous, recurrent multisystem inflammatory disorder whose etiology and pathogenesis are fairly unknown. Vessels (particularly veins), joints, gastrointestinal system, and central nervous system involvement may also be observed, except for the classic triad of oral aphtaes, genital ulcerations, and uveitis2). The prevalence of neuro-Behçet's disease (NB), presenting two types of involvements as parenchymal and non-parenchymal, is at the rate of 2.2% to 50%3). The brainstem and/or the corticospinal tract are affected during the parenchymal involvement. Findings such as elevated intracranial pressure, behavioral disorders, or isolated headache progressing as a result of aseptic meningitis or venous sinus thrombosis may be experienced in cases with non-parenchymal involvement2).
A neuro-Behçet's case with parenchymal involvement has been examined in light of literatures in terms of differentiation from tumoral and demyelinating diseases.
Go to : 
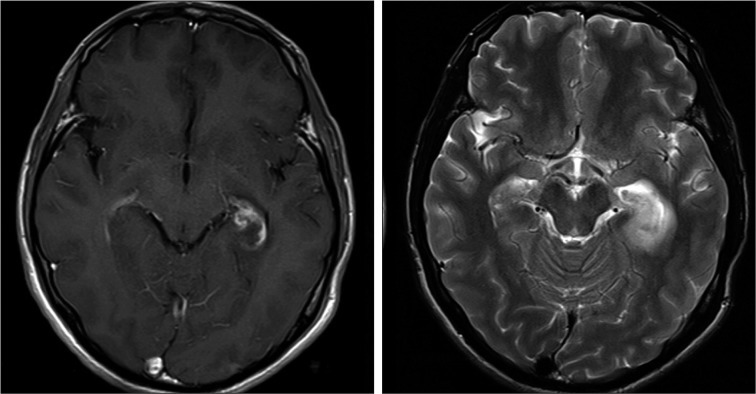
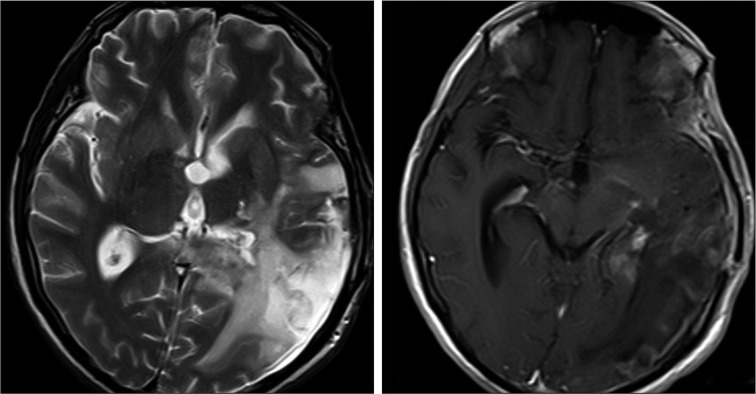
The 25-year-old male patient diagnosed with BD three years ago was admitted to our clinic with complaints of recurrent throbbing headache accompanied by nausea and vomiting for four months. The neurological examination of the patient was normal. On the Cranial magnetic resonance imaging (MRI), a lesion that was thought to be accordant with choroiditis or a tumor with a diameter of one cm was detected near the left lateral ventricle posterior horn and near the left temporal lobe uncus (Fig. 1). Lumbar punction (LP) could not performed because the patient did not give permission for an LP. The patient was then discharged. On the basis of the intracranial mass (malignancy?) diagnosis, a tumor excision was made on the patient who applied at another center. The pathological examination was consistent with a definite loss of myelin in the lesion via the immuno-histochemical method. Finally, it was commented as having a demyelinating non-tumoural etiology. After the operation, intensive oedema areas were observed in the left temporo-parietal, left pons hemisphere, and left mesencephalic hemisphere on the cranial MRI (Fig. 2). Right hemiparesis and motor aphasia were observed and three weeks later the patient suffered from secondary generalized tonic-clonic seizures. Triple antiepileptic and 1 gr/day methyl prednisolone were given to the patient who suffered persistent seizures and lethargy. Colchicine treatment was administered for BD. The patient's seizures were kept partially under control with this treatment, and he was discharged with the recommendation of coming to the controls.
Go to : 
Behçet's Disease was first described by Dr. Hulusi Behçet in 1937 as a classic triad of recurrent oral aphtaes, genital ulcerations, and uveitis disease4). The mean age range of onset of BD is 20-30 and its neurological involvement comes out averaging five years after the systemic findings. It is observed that BD is three to four times more common among males compared to females6). Neurological involvement reveals itself primarily in the form of central nervous system (CNS) involvement, but peripheral nervous system's or muscles' involvement is highly rare.
A form of a brainstem syndrome, which develops within days, is frequently seen in parenchymal involvement. In general ataxia, dysarthria, hemiparesis, bipolar pyramidal findings, cognitive disorder, and sphincter defect are detected during the examination. Headache and fever may occur in this type of involvement5). Siva et al. reported that headaches in NB disease is at a high rate of 61%7). The headaches continuing for four months in our patient is thought to be secondary to BD or to intracranial mass accompanied by nausea and vomiting along with persistence and throbbing. As stated in the literature, parenchymal CNS involvement may first occur as a headache and it is always accompanied by neurological findings, but not accompanied in our patient. In a great majority of cases with NB, headache types such as tension-type headache or migraine can be seen as well. It may even be discussed that systemic BD exacerbations, for example, oral aphthaes, genital ulcerations, and uveitis, trigger these primary headaches among certain patients. Interestingly, about 5 percent of patients suffer from migrainous headache only during the systemic BD exacerbations and their headaches disappear via the treatment of these systemic BD exacerbations rather than the analgesics7).
According to the MRI images of our patient with headaches, a contrast-enhanced mass-like lesion existed near the left temporal lobe uncus. It was thought that this image could be either a tumoral mass or indication of parenchymal involvement of NB. On cases with parenchymal involvement of neuro-Behçet, the MRI presents lesions that extend characteristically from brain stem or basal ganglia to diencephalic structures and that appear hyperintense on T2 weighted-sections. The MRI also reports the lesions at the center of which a small contrast involvement is seen and that can be unilateral or bilateral. Additionally, the MRI points to the lesions that can show mild mass effect. It appears that these lesions become smaller by treatment and their sparsed milimetric T2 hyperintensities remain1). Nevertheless, it must be kept in mind that there may be metastatic or primary CNS tumor in BD. The pathology result of the material is reported as a nontumoural demyelinating nature after the excisional surgery that is carried out with the diagnosis of tumor epicenter. The MRI presents particularly white-matter lesions among approximately 10% of the patients with NB and it may be really difficult to differentiate these lesions from MS lesions1).
Cerebrospinal fluid examination is auxiliary in differentiating parenchymal neuro-Behçet's disease from MS in the diagnosis. In general, slightly moderate lymphocyte and polymorphonuclear cell proliferation along with moderate concentrations of protein levels (generally <100 mg/dL) are observed, even though this elevation is sometimes perceived as normal. Oligoclonal IgG bands are not usually detected in the cerebrospinal fluid, but the IgG index may have increased. Apart from supporting inflammatory neurological involvement, abnormal cerebrospinal fluid findings point to poorer prognosis and necessitate more aggressive treatment2). Cerebrospinal fluid analysis could not be made in this case, but temporal uncus lesion rather than the periventricular multiple plaques led us to think of vasculitis or a malignate lesion instead of MS.
Go to : 
For the cases encountering difficulties in differential diagnosis, if it is thought that this type of lesion may represent a finding of NB (demyelinating, in particular) or if it is considered that a metastatic or primary tumor may occur coincidentally, then it needs to be followed up as to whether this type of lesion is becoming smaller or not, primarily after the systemic treatment of BD. Also, it should be borne in mind that stereotactic surgery is the last option vis-à-vis the lesions that do not get smaller or that get slightly bigger.
Go to : 
References
1. Akman-Demir G, Bahar S, Coban O, Tasci B, Serdaroglu P. Cranial MRI in Behçet's disease : 134 examinations of 98 patients. Neuroradiology. 2003; 45:851–859. PMID: 14557904.

2. Akman-Demir G, Serdaroglu P, Tasçi B. The Neuro-Behçet Study Group. Clinical patterns of neurological involvement in Behçet's disease : evaluation of 200 patients. Brain. 1999; 122:2171–2181. PMID: 10545401.
3. Al-Fahad SA, Al-Araji AH. Neuro-Behcet's disease in Iraq : a study of 40 patients. J Neurol Sci. 1999; 170:105–111. PMID: 10561525.
4. International Study Group for Behçet's Disease. Criteria for diagnosis of Behçet's disease. Lancet. 1990; 335:1078–1080. PMID: 1970380.
5. Kara B, Somer A, Pişkin S, Aydinli N, Salman N, Yalçin I. Neuro-Behçet syndrome presenting as acute meningeal syndrome. J Infect. 2006; 52:e120–e123. PMID: 16197999.
6. Serdaroğlu P, Yazici H, Ozdemir C, Yurdakul S, Bahar S, Aktin E. Neurologic involvement in Behçet's syndrome. A prospective study. Arch Neurol. 1989; 46:265–269. PMID: 2919979.
7. Siva A, Kantarci OH, Saip S, Altintas A, Hamuryudan V, Islak C, et al. Behçet's disease : diagnostic and prognostic aspects of neurological involvement. J Neurol. 2001; 248:95–103. PMID: 11284141.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download