INTRODUCTION
Cervical spondylosis is a common pathological condition affecting the adult spine and is the most frequent cause of cervical radiculopathy and myelopathy in older patients. Anterior cervical discectomy and fusion (ACDF) is a well-established treatment modality that has been shown to achieve good to excellent clinical results in the patients with cervical degenerative disc disease (DDD). Nevertheless, its principal disadvantage is the loss of motion segments, which may lead to a higher incidence of adjacent segment degeneration and segmental instability
7,
10,
13). Cervical total disc replacement (C-TDR) is a relatively new spinal surgical procedure that is used to preserve motion at the treated level. This preservation of motion is thought to decrease adjacent segment degeneration by avoiding the abnormal kinematic stresses produced by ACDF
15). In addition, the theoretical advantages of C-TDR include : maintenance of a range of movement (ROM), reconstitution of disc height and spinal alignment, greater maintenance of maneuverability, and allows an earlier return to the previous level of function. In cases of multilevel cervical DDD, ACDF remains the most largely accepted procedure with a satisfactory clinical outcome and proven radiological fusion ranging from 90 to 100%. However, longer fusions may cause greater stresses at adjacent levels than single level fusion and likely lead to adjacent segmental disease (ASD)
12,
14).
The purpose of this study was to evaluate the clinical and radiologic outcomes of C-TDR combined with ACDF in patients with multilevel cervical DDD. Furthermore, in our study, the limitations due to sample size and no control group prevented us from our drawing firm conclusions. We reviewed the literature and analyzed the postoperative clinical outcome and complication with those of other studies that examined HS in similarly categorized patients.
Go to :

MATERIALS AND METHODS
After institutional review board approval was obtained, a retrospective review of all contiguous multilevel (2 or 3 level) hybrid surgery was performed. Hybrid surgery was defined as a TDR with an adjacent fusion. From January 2005 to January 2010, 51 patients (40/11 males/females) ranging in age from 29 to 70 years (mean age 49.1 years). Patient inclusion criteria consisted of consecutive level of cervical DDD between C3-C4 and C6-C7 with disc herniation or spondylosis, with radiculopathy or myelopathy, which had not responded to conservative treatment (medication during at least 6 weeks). Exclusion criteria included the same currently accepted for ACDF or C-TDR, such as previous cervical spine surgery involving the use of any other device, axial neck pain as the solitary symptom, significant cervical anatomic deformity, radiographic signs of instability, ossified posterior longitudinal ligament, and active infection. Target levels were consecutive in all cases. Among the multilevel, at least one-level must meet the criteria for arthroplasty. Cervical TDR was performed at a mobile and non spondylotic segment. Fusion or TDR was determined using both preoperative flexion-extension radiographs and computed tomography (CT) scans. In order to define the precise selection criteria for choosing ACDF or TDR at each disc level, the following factors were considered before surgery; 1) Presence of motion on preoperative dynamic X-rays. In the case of no motion at the target level, ACDF was preferred; 2) Radiographic signs of instability (translational instability of more than 2 mm, angular motion more than 11 degrees greater than either adjacent level). ACDF was performed; 3) Advanced vertebral body spondylosis or facet degeneration on preoperative CT scan. In these cases, ACDF was performed; 4) Bony spur or gross bony abnormalities. ACDF was preferred because of the increase in inducing heterotopic ossification. In addition, if the target segment met the TDR criteria, the segment with greater motion received the TDR (C5-6>C4-5>C6-7>C3-4)
24).
Surgical technique
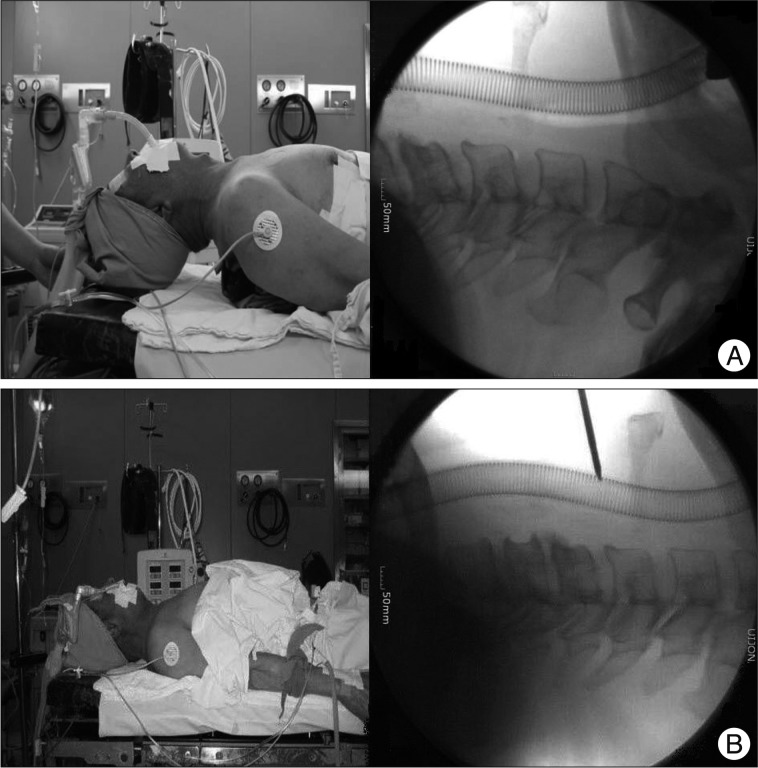
The hybrid surgical technique was the same as the method used in routine ACDF and C-TDR, respectively. A standard Smith-Robinson approach, the cervical microsurgical discectomy, was used in all cases to perform the neural decompression and prepare the disc space and the vertebral end plates for positioning of either a cage or disc prosthesis. Patients underwent an arthroplasty using an artificial discs (Prodisc C, Synthes, West Chester, PA, USA; Bryan disc, Medtronic Sofamor Danek, Memphis, TN, USA), combined with a cervical plate system (Zephir plate; Medtronic, Memphis, TN, USA). Before surgery, we placed a tourniquet below the patient's upper back to change the patient's neck position according to the ACDF or TDR. During the ACDF, we inflated the tourniquet to extend the patient's neck to keep the lordosis. In contrast to TDR, we deflated the tourniquet to keep the patient's neck position neutral. (
Fig. 1). A standard technique as described by manufacturers was used to implant the different devices. At our institution, TDR was performed first and fusion was performed later. All cages were filled with autologous iliac bone.
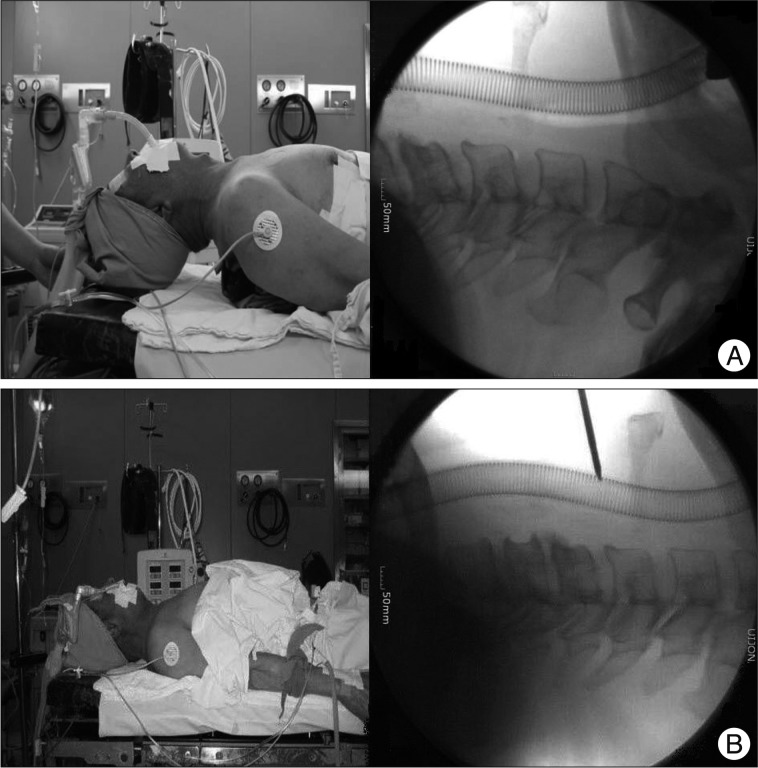 | Fig. 1A : Tourniquet was inflated to extend the patient's neck to maintain the lordosis during the anterior cervical discectomy and fusion. Patient's neck shows extension on C-arm image. B : Tourniquet was deflated to place the patient's neck in a neutral position during the total disc replacement. Patients' neck shows neutral alignment on C-arm image. 
|
Clinical outcomes and review of articles
The reviewed clinical outcomes were analyzed based on the Visual Analogue Scale (VAS) score and the neck disability index (NDI) questionnaires (preoperatively and 1, 6, 12, 24 months follow up). Pain intensity was reported from 0 to 10 using a subjective visual analog scale (VAS; 0=no pain; 10=the worst pain imaginable). The NDI scores varied from 0 to 50. The results were recalculated and expressed on a scale ranging from 0% (no disability) to 100% (maximum disability). Clinical outcomes were assessed by a neurosurgeon (J-Y Kim), who didn't participate in the surgery.
Previously published articles were reviewed to evaluate the effect and safety of hybrid surgery in 2-level cervical degenerative disease. English language articles were retrieved using PubMed by searching for "cervical spine," "arthroplasty," "fusion," "hybrid," and "degenerative disc disease." This search was supplemented by manually searching reference lists within all relevant articles. Cases in which combined fusion and arthroplasty was performed in patients with multilevel cervical disease were collected. A total of 75 cases in 3 articles were selected. The information entered into this analysis included 1) year of publication, 2) number of patients treated by hybrid surgery, 3) sex, 4) age, 5) treated level, 6) clinical outcome (VAS or NDI), and 7) complications.
Radiological evaluation
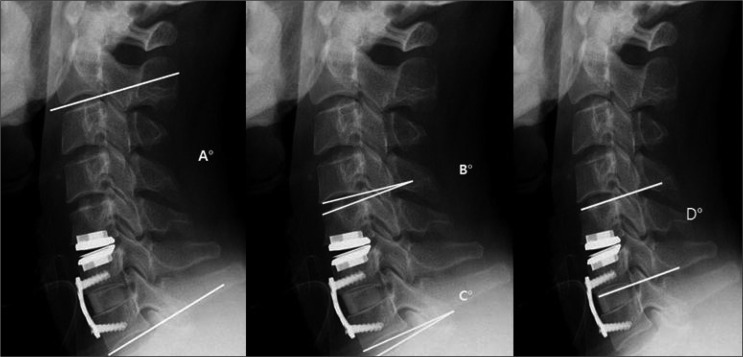
All patients underwent preoperative flexion-extension radiography, CT scanning, and magnetic resonance imaging of the cervical spine. Flexion-extension radiographs were evaluated preoperatively and postoperatively at intervals of 1, 6, 12 and 24 months. The angular range of motion (ROM) for C-2 to C-7 and adjacent segment (upper and lower) were measured using the Cobb's measurement tools with PACS workstation (Marosis, Marotech, Korea) (
Fig. 2). We also analyzed the change of the ROMs of arthroplasty level after fusion to investigate the biomechanical stress on artificial disc prostheses, due to their placement adjacent to the fused level (
Fig. 2). The ROM was calculated based on the difference in Cobb angles between full flexion and full extension on the lateral radiograph. Lordosis was expressed as a negative value and kyphosis was expressed as a positive value. These data were calculated by a neurosurgical resident who was not involved in the surgery. We checked the ROM twice and obtained the mean to reduce the error.
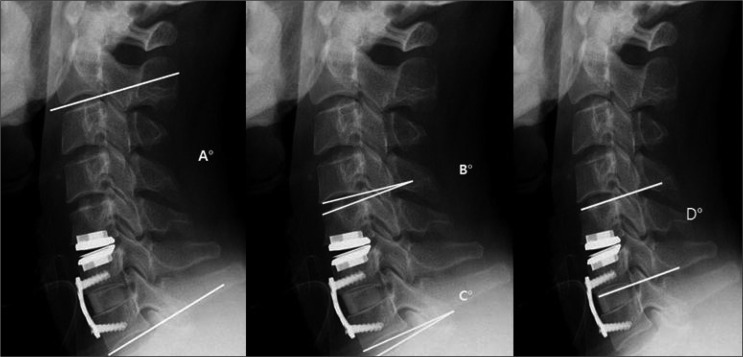 | Fig. 2Radiographs illustrating how to measure the range of motion (ROM). The ROM of the whole cervical spine is defined as the difference in the Cobb's angle of C2-C7 between the flexion and extension view (A°). The ROM of upper adjacent segment (B°) and lower adjacent segment (C°) is defined as the difference in the Cobb's angle of adjacent level in the treated unit between the flexion and extension view. The ROM of arthroplasty level is calculated in the dynamic lateral simple radiographs (D°). 
|
Statistical analyses
Statistical analyses were conducted using SPSS version 17 software (SPSS Inc., Chicago, IL, USA). Clinical outcome was assessed by an outcome scales (VAS and NDI score). Data are given as mean±standard deviation (SD).
NDI, VAS score and the statistical differences of the ROM were analyzed by the Student t test. Differences were considered to be significant when the statistical p value was <0.05.
Go to :

RESULTS
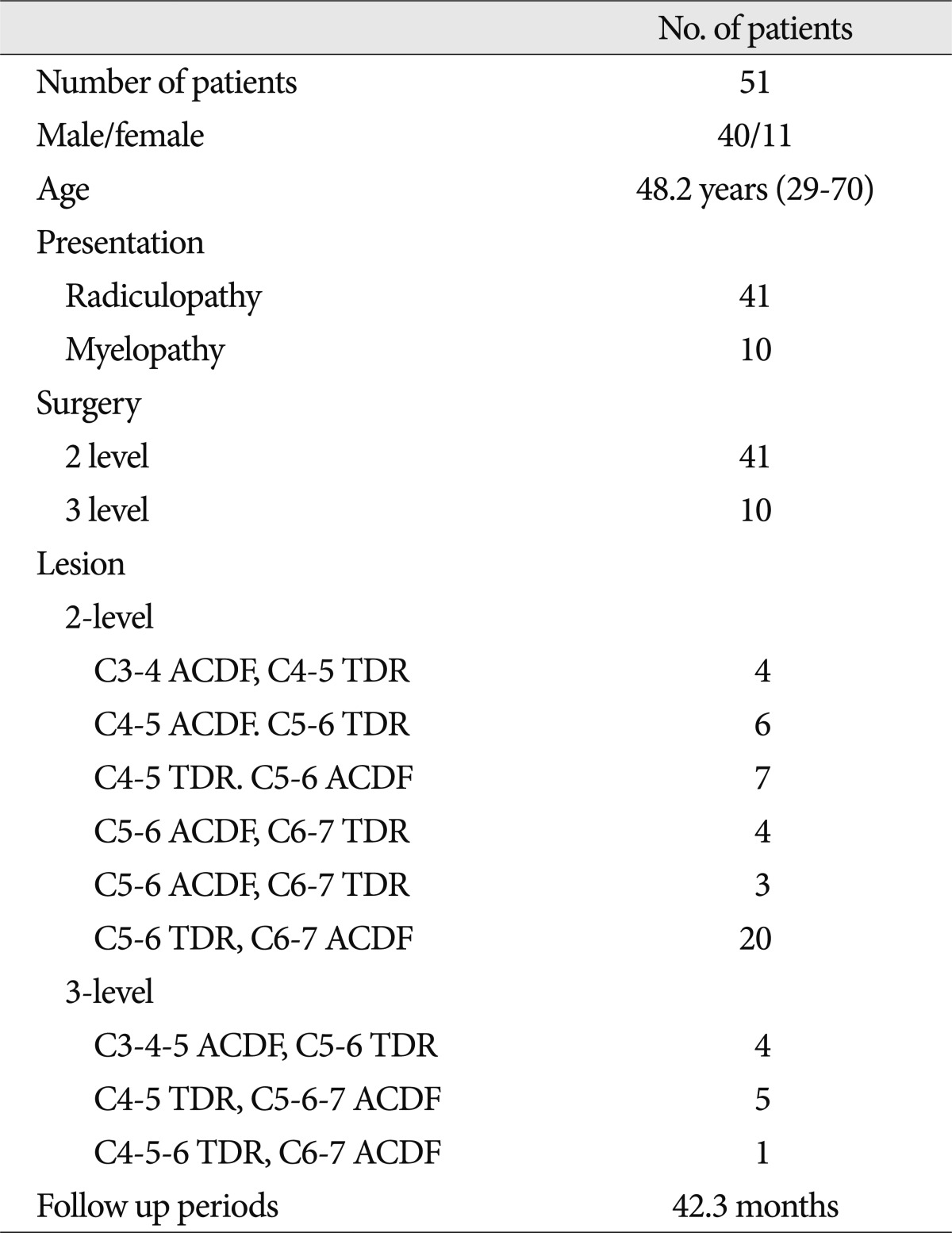
Over 5 years, fifty-one patients with 2- or 3- consecutive level of DDD were treated by implantation of a hybrid construct at our institution. The mean clinical and radiological follow-up was 42.3 months (range 24-84 months). A diagnosis of radiculopathy and/or myelopathy was established in all patients. The demographic and clinical data of the 51 patients were collected and are presented in
Table 1. The male-to-female ratio was 40 : 11 and mean patients age was 48.2 years (range, 29-70 years).
Table 1
Summary of the demographics and procedural details
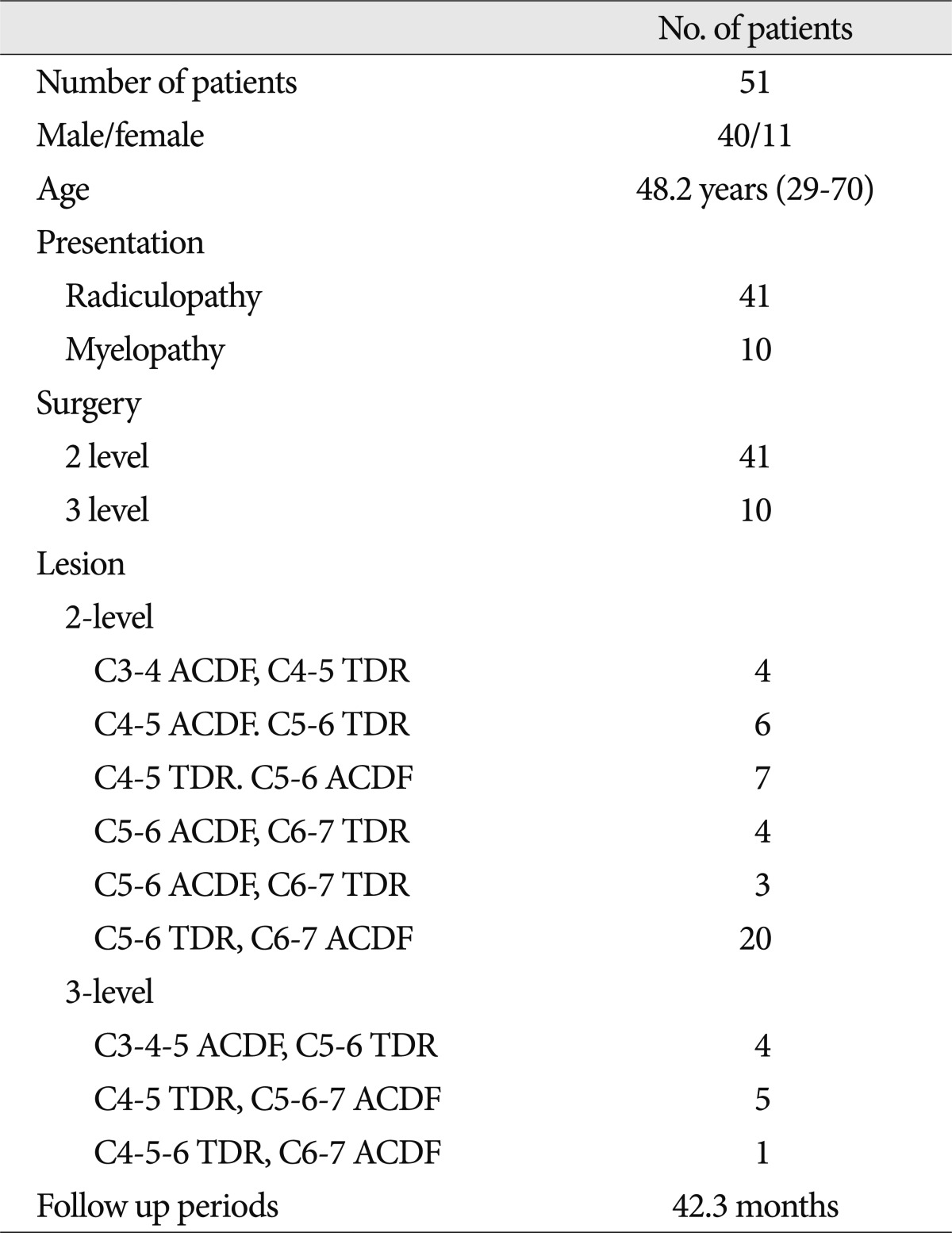

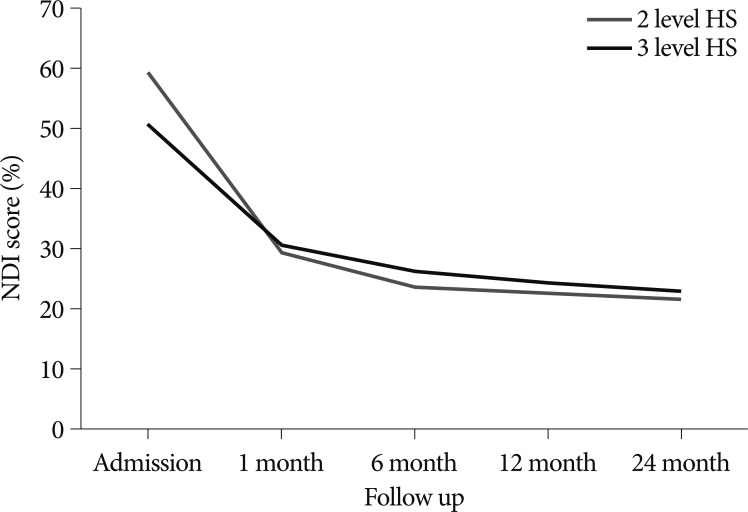
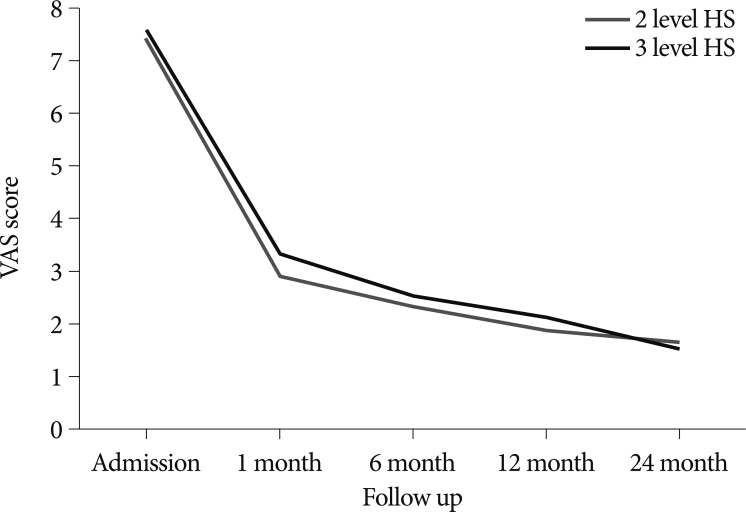
Fig. 3 and
4 show the clinical outcomes. The mean NDI scores (mean±SD) of 2-level hybrid surgery score significantly improved after surgery (on admission, 59.2±9.5%; 1 month after surgery, 29.39±5.4%; 6 month after surgery, 23.53±3.0%; 12 months after surgery, 22.8±2.62%; 24 months after surgery, 21.6±3.4%,
p=0.006). For the 3-level hybrid surgery, the corresponding mean NDI were 50.7±7.1%; 30.3±3.1%; 26±2.5%, 24.2±2.6% and 23±3.2% respectively. The mean VAS scores of 2-level hybrid surgery for arm pain were 7.5±0.9 preoperatively; 2.9±0.7, 1 month after surgery; 2.3±0.5, 6 months after surgery; 1.9±0.5, 12 month after surgery; and 1.6±0.7, 24 months after surgery. For the 3-level hybrid surgery group, the corresponding mean VAS scores were 7.6±0.8; 3.3±0.5; 2.5±0.5; 2.1±0.4 and 1.5±0.5% respectively. There was a trend toward a rapid decrease in the NDI and VAS scores immediately during the postoperative period, followed by a slow decrease in the NDI and VAS scores in both groups. There was no significant difference between the NDI and VAS scores of both groups at the last follow up (
p<0.05).
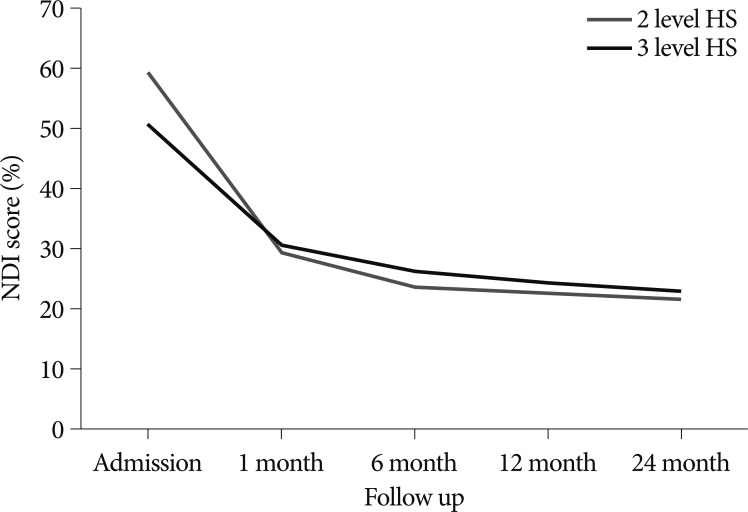 | Fig. 3The mean NDI scores decreased significantly in 2-level and 3-level HS. There is no difference between both groups. NDI : neck disability index, HS : hybrid surgery. 
|
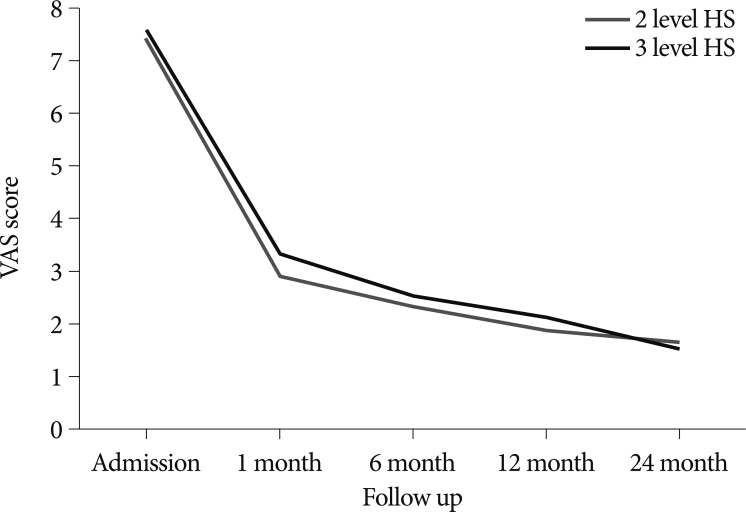 | Fig. 4The mean VAS scores decrease significantly in 2-level and 3-level HS. There is no difference between both groups. VAS : Visual Analogue Scale, HS : hybrid surgery. 
|
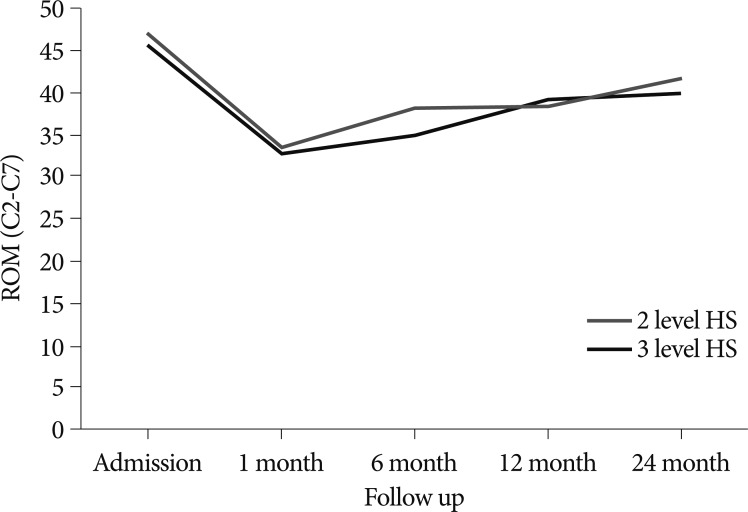
Fig. 5 shows the ROM of the cervical spine. The overall mean cervical ROMs of 2-level HS were 46.9±12.5° preoperatively; 33.4±9.3°, 1 month after surgery; 38.2±8.7°, 6 months after surgery; 38.4±5.9°, 12 months after surgery, and 41.6±8.1°, 24 months after surgery, whereas corresponding ROM of 3-level of HS were 45.5±10.1° preoperatively, 32.8±12.5°, 34.9±8.8°, 38.8±7.4° and 39.7±9.1° respectively (
Fig. 5). The cervical motion was significantly limited immediately after surgery and then gradually recovered. There was no significant difference between ROM of 2-level HS and that of 3-level HS (
p=0.13).
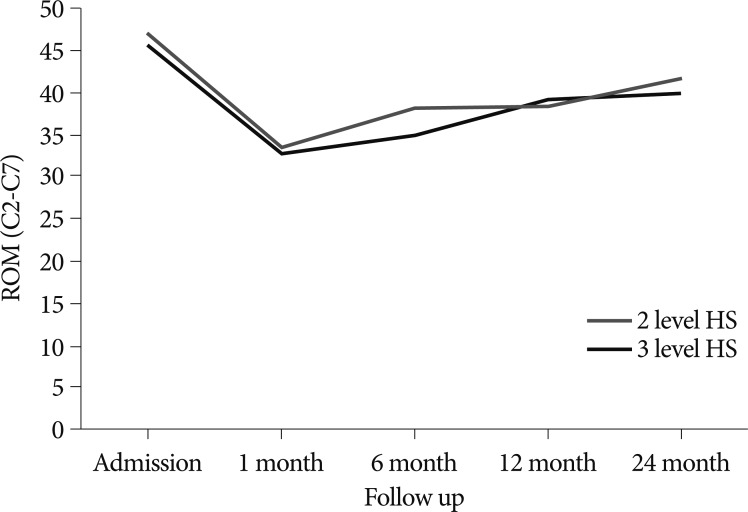 | Fig. 5The ROM of cervical spine was recovered at 6 and 12 month after HS. There is no difference between both groups. ROM : range of motion, HS : hybrid surgery. 
|
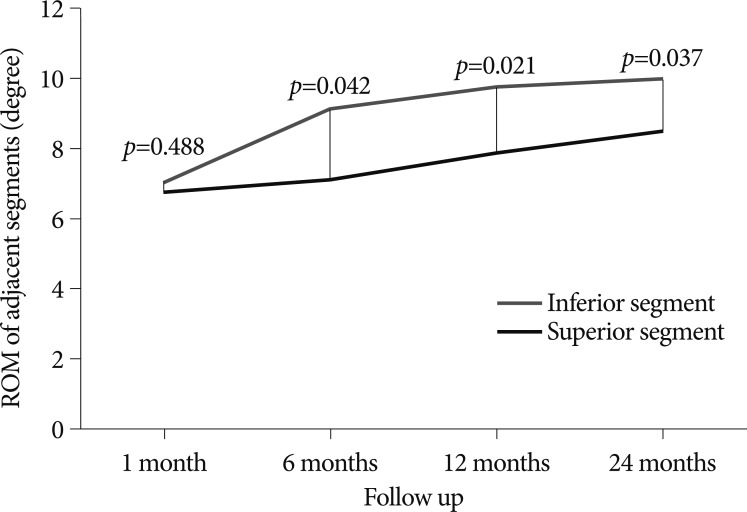
Fig. 6 shows the change of the ROM of adjacent segments. The mean inferior adjacent segment ROMs were 7.0±3.9°, 1 month after surgery; 9.1±3.9°, 6 months after surgery; 9.7±3.9°, 12 months after surgery; and 9.9±4.2°, 24 months after surgery. The corresponding mean superior adjacent segment ROM scores were 6.7±3.9°, 7.03±4.2°, 7.8±4.0°, and 8.4±3.9°, respectively. There was a significant difference between superior segments ROM and inferior segment ROM during the follow up periods (
p=0.037).
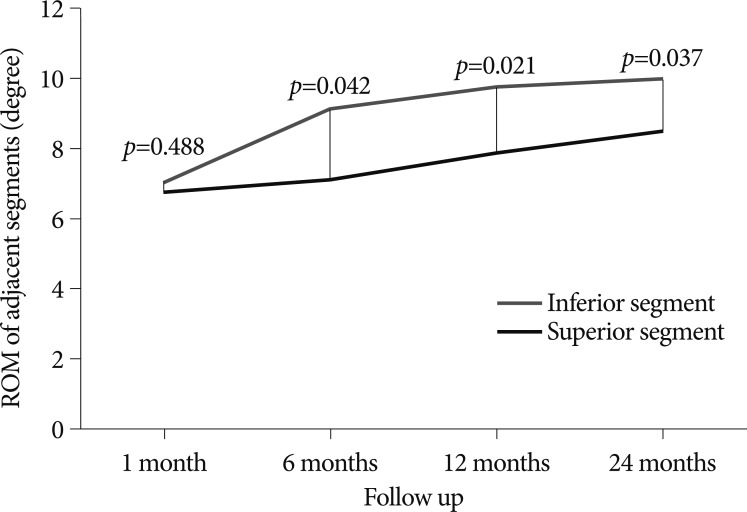 | Fig. 6The ROM of inferior adjacent segments is significantly larger than that of superior adjacent segments after HS. ROM : range of motion, HS : hybrid surgery. 
|
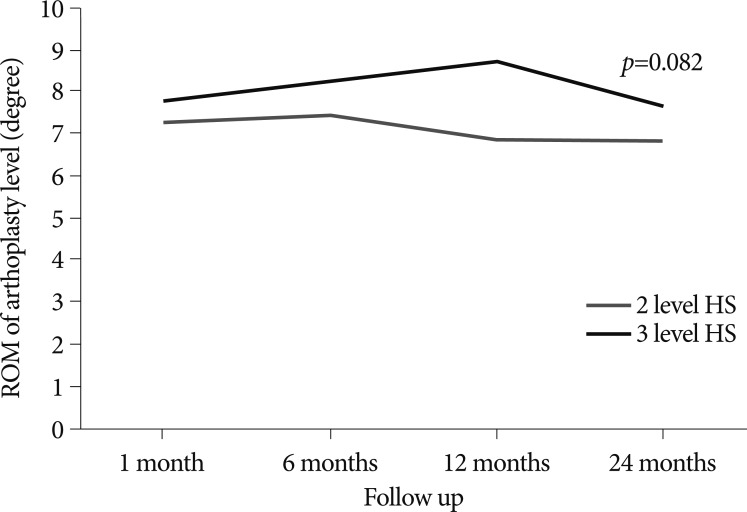
We also investigated the ROM of arthroplasty level adjacent to the fusion level and the results are shown in
Fig. 7. The ROM of the arthroplasty level in 2 level hybrid surgery at 1 month postoperatively, 7.3±3.2° at 1 month; 7.4±3.01° at 6 month; 6.9±3.01° at 12 months; 6.8±2.7° at 24 months. The corresponding ROM of 3 level surgery were 7.8±1.6°; 8.3±1.4°; 8.7±2.1°; 7.7±2.1°, respectively. There were no significant changes of ROM at the arthroplasty level during the follow up periods. Although the ROMs of arthroplasty level in 3 level HS were larger than that of 2-level HS, no differences were observed between 2-and 3-level hybrid surgery (
p=0.082).
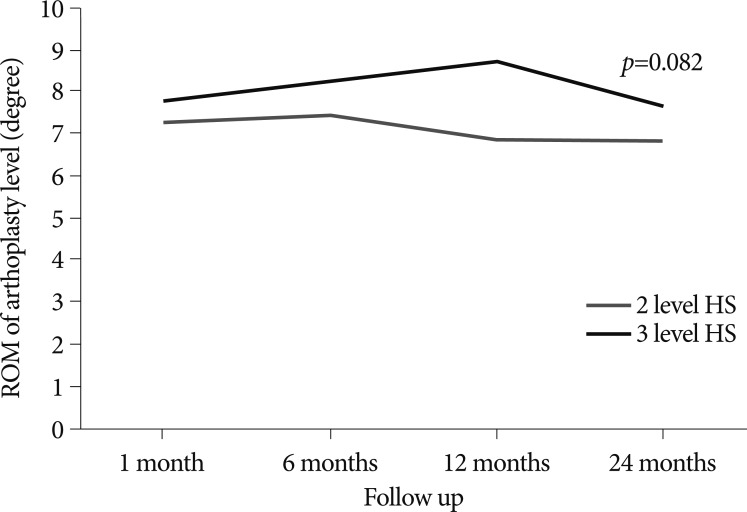 | Fig. 7The mean range of ROM at arthroplasty level was from 3.8 degree to 12.4 degree. There are no significant changes of ROM at TDR level during the follow up periods. ROM : range of motion, TDR : total disc replacement, HS : hybrid surgery. 
|
During the follow up periods, no case of screw back out, implant dislodgment, progressive kyphosis, formation of heterotopic bone, evidence of pseudarthrosis at the fusion levels, or development of symptomatic adjacent-level disease was observed.
Go to :

DISCUSSION
ACDF, a safe and reliable technique, is regarded as the gold standard procedure for single or multilevel cervical spondylosis leading to radiculopathy and/or myelopathy
6,
8,
22,
23). However, fusion can lead to a loss of ROM and increase of load to adjacent levels, which may accelerate degeneration in adjacent segments. Baba et al.
1) reviewed the cases of 106 patients with cervical spondylotic myeloradiculopathy who were treated with ACDF and reported that spinal stenosis had occurred at adjacent segments in 25% of the patients during a 8.5 year follow up period. Hilibrand and Robbins reported that, annually, 2.9% of patients developed adjacent segment disease after ACDF that required cervical intervention
11,
18). Furthermore, it has long been hypothesized that longer fusions cause greater stresses at adjacent levels, which likely lead to ASD
12,
14,
21). To date, several cervical disc replacement systems have been developed to make up for the disadvantage of ACDF. C-TDRs offer many distinct advantages over the traditional ACDF and resulted in preserved segmental motion and improved clinical outcomes. C-TDR is also believed to reduce the incidence of ASD. Robertson et al. reported that maintaining motion rather than fusion will delay or prevent symptomatic postoperative disc disease and will decrease to a significant degree the associated adjacent-level radiological disc disease
23). Although, there is a considerable body of literature regarding the outcome of single level C-TDR, multilevel cervical TDR has not been comprehensively investigated. Some authors have suggested multilevel C-TDR with excellent outcomes
5,
17). However, the follow-up periods and number of patients in the current studies were too short and small. In addition, multilevel C-TDR may permit unnecessary extra-motion in the treated levels. High medical costs may also be a problem. In line with this idea, we speculated that HS may be suitable for multilevel cervical disease and will reduce the extra-load in adjacent segment. The rationale of HS was based on the notion that the most suitable treatment must be provided at each disc level respectively according to the status of affected level. Furthermore, the reason to perform HS is that multilevel degenerative disease of the cervical spine did not show the same type and degree of degeneration at each affected disc level. Therefore, there is no need to fuse all the affected levels, if alternative, safe and effective treatment can be performed. The main goals of this hybrid construct are preserving the segmental motion of the cervical spine, avoiding the long level fusion, preventing further long-term adjacent degeneration, and maintaining the functional spinal unit and ROM of cervical spine.
Our surgical protocol of multilevel cervical DDD was to perform the C-TDR if the target levels are mobile and non spondylotic. However, in most cases, not all of the target levels met the C-TDR criteria because most of degenerative levels showed no motion, a collapsed intervertebral space, facet degeneration or bony spurs. There are no absolutely reliable criteria for choosing ACDF or TDR at each affected level. As mentioned in the selection criteria in the methods section in our study, the facet joints condition, degree of spondylotic change and segmental ROM were important elements in the evaluation process leading to the final decision on whether to choose arthroplasty or arthrodesis. The presence of facet hypertrophy, partial fusion, artheroscleotic change and segmental instability were contraindication to arthroplasty at the affected level.
In our 53 patients, neurological follow-up confirmed the resolution of neck pain and radiculopathy in all patients. Shin et al.
21) reported clinical and radiological outcomes of 2 level HS compared to 2 level ACDF and reported that both surgeries were effective in eliminating radicular pain, and hybrid surgery had a more favorable recovery of NDI scores. However, Sasso et al.
19) reported better arm pain relief in C-ADR compared to the ACDF. Our results demonstrated that HS was effective in reducing neck and arm pain. But, we believe that this was the result of nerve root decompression rather than the specific technique-ACDF versus TDR-used.
Radiographic analysis demonstrated preserved postoperative cervical lordosis with all HS. ROMs of cervical spine were recovered at 6 and 12 month after surgery compared to preoperative status. When analyzing the ROM of adjacent segments, the mean ROM of the inferior adjacent segment was significantly larger than that of the superior segments during the follow up periods in our study. Schwab et al.
20) examined the cervical spine kinematics in a human cadaveric study and found that a greater compensation occurred at the inferior segments for the lower levels (C5-C6, C6-C7) fusion, and the superior segments had greater compensation than the inferior segments when the upper levels (C3-C4, C4-C5) were fused. In our study, sampling error may affect the results because the number of the upper level fusion (C3-C4, C4-C5, 14 cases) was relatively low compared to the lower level fusion (C5-C6, C6-C7, 33 cases). Although, no clinical and radiological ASDs were observed during the follow up periods, increase ROMs of inferior segments may accelerate the degenerative change of adjacent segments. A long term follow up study will be needed to clarify this.
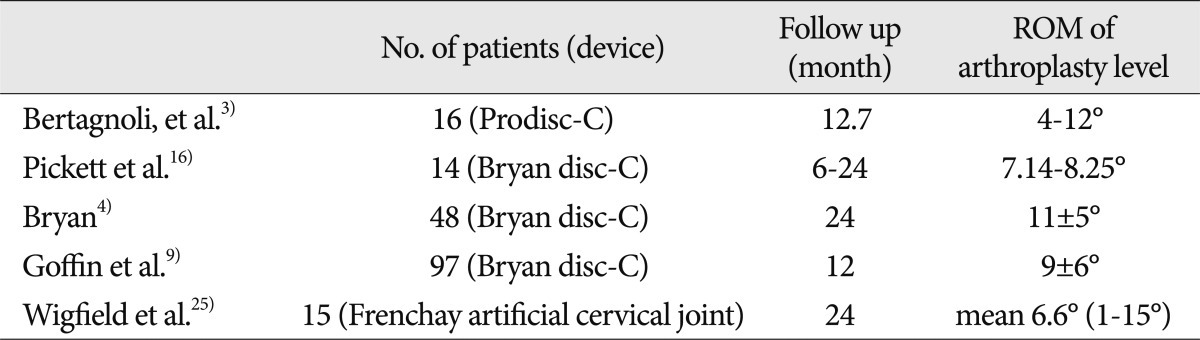
We also hypothesized that hybrid surgery could increase the load on an artificial disc because of their placement adjacent to fused level and likely lead to prosthesis failure or dislocation. In spite of not having a true control group, we are able to compare our results with others
3,
4,
9,
16,
25). During the follow up periods, we measured the ROM of TDR level to confirm the presence of functioning artificial discs by analyzing the postoperative flexion-extension views (
Fig. 6). The ROM at the TDR level ranged from 3.8 degree to 12.4 degree. These results are consistent with ROM of TDR level in hybrid surgery compared favorably with the range of results that were reported in the literature (
Table 2). Furthermore, no device-related complications were observed in our study during the follow up periods. This suggests that fusion did not interfere with the normal function of artificial disc prostheses; however, because of the limitations in the sample size and no control group, we could not reach any statistical conclusions.
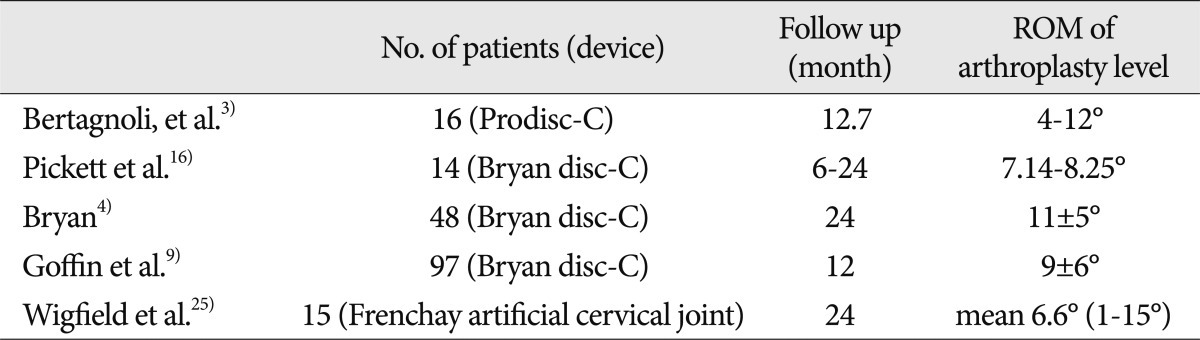
Table 2
Range of motion at the single level arthroplasty

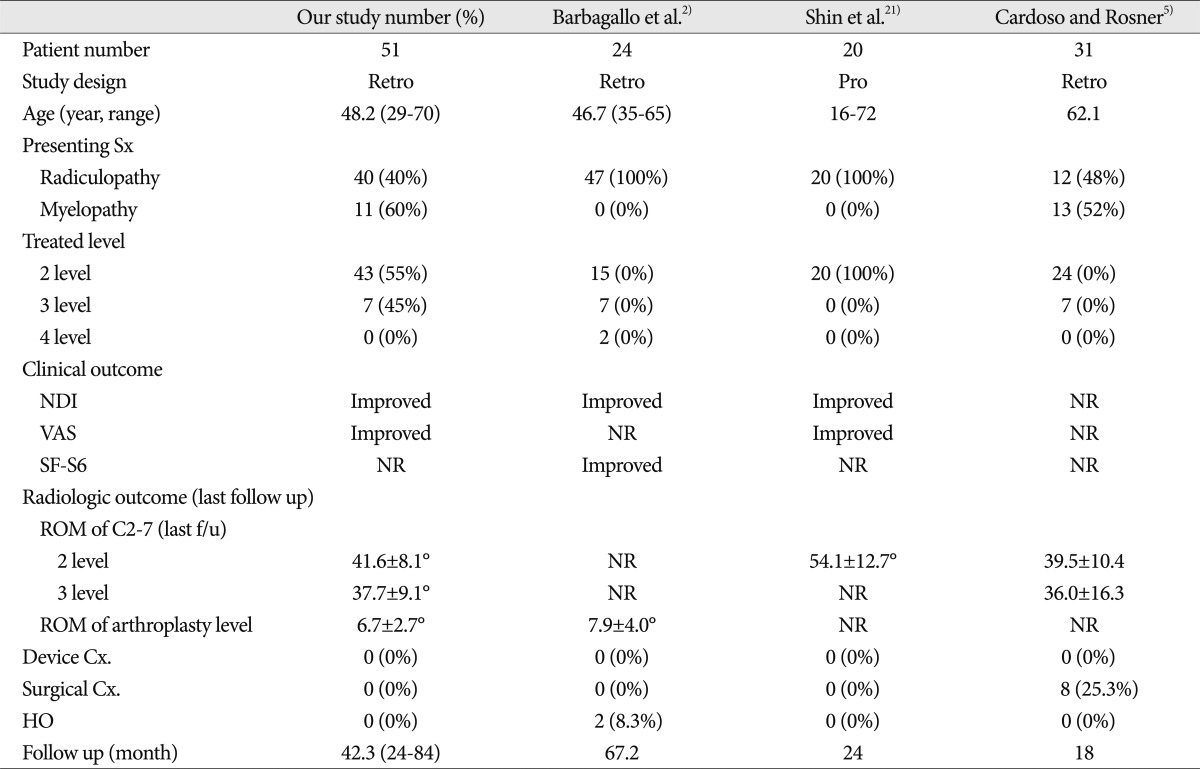
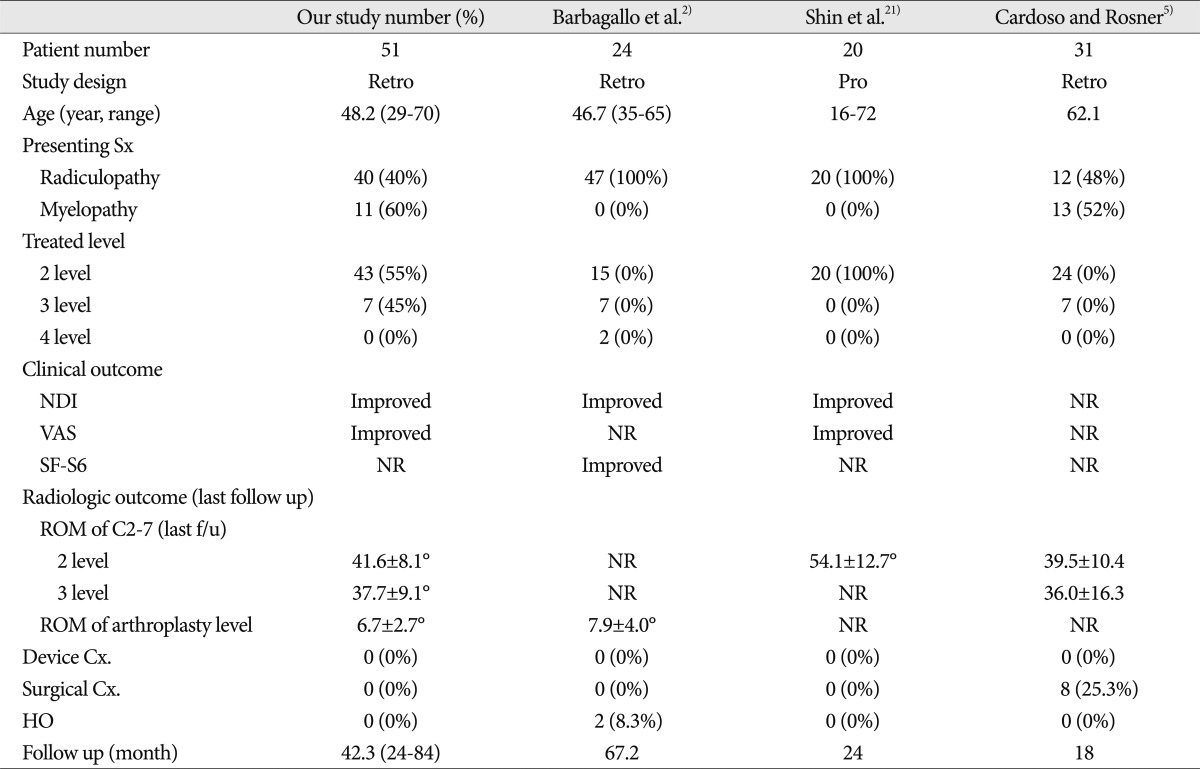
In review of other articles, there was a 3 series involving a total of 75 cases that met our selection criteria (
Table. 3)
2,
5,
21). Of these, two studies reported multilevel (>2 level) hybrid surgery and one study reported only 2 level hybrid surgery. In a study of 20 patients with 2 level HS compared to 2 level ACDF by Shin, they concluded that HS was effective in decreasing the VAS score, NDI and was superior to 2-ACDF in terms of better NDI recovery, less postoperative neck pain. In a study by Barbagallo, 24 patients that underwent multilevel HS (2 level; 15 patients, 3 level; 7 patients, 4 level; 2 patients), and 23 patients demonstrated significant clinical improvement (NDI, SF-36, Nurick Scale). In studies by Shin and Cardoso, cervical ROM showed faster recovery and less adjacent ROM increase than 2-level ACDF. In a study by Barbagallo, the ROM of athroplasty level was reported to range from 3-15° after HS and showed normal functioning disc prosthesis. Regarding complications, 8 transient neurologic deficits after HS were reported by Cardoso, but these complications were fully recovered at the last follow up. No implants (disc prosthesis, cage and plate) failures were reported in 3 studies. Additionally, heterotopic ossification was observed in 2 cases in a study by Barbagallo.
Table 3
Outcomes in patients with multilevel cervical spondylosis treated by hybrid surgery

Through the review of other similar studies, we found that HS was a safe and effective alternative to multilevel fusion for the management of multilevel cervical DD. However, the follow-up periods and number of patients in the current studies were too short and small to come to any firm conclusions, and we could not determine whether it also reduces adjacent-level disease compared with a similar-level fusion. Thus, further studies are needed to clarify this.
The present study had several limitations. The major limitations were the retrospective nature and lack of a control group. Our study was composed of a small and heterogeneous collection of patients treated over a 5-year period. As a result, it is difficult to conclude that the hybrid surgery was more safe, effective than multilevel C-TDR and reduce the ASD compare to the same level fusion. The final decision regarding whether to consider hybrid surgery, multilevel fusion or TDR remains relatively subjective. We await with interest the results of randomized controlled trials of hybrid surgery, multilevel TDR for patients with multilevel cervical DDD.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download