Abstract
A spinal epidural hemangioma is rare. In this case, a 51 year-old female patient had low back pain and right thigh numbness. She was initially misdiagnosed as having a ruptured disc with possible sequestration of granulation tissue formation due to the limited number of spinal epidural hemangiomas and little-known radiological findings. Because there are no effective diagnostic tools to verify the hemangioma, more effort should be put into preoperative imaging tests to avoid misdiagnosis and poor decisions).
Spinal epidural hemangiomas have been reported in the literature, but most of them were cavernous type hemangiomas that enable a preoperative differential diagnosis with relative ease. The occurrences of spinal epidural hemangioma are exceedingly rare. The limited number of spinal epidural hemangiomas and few radiological findings make an exact diagnosis difficult prior to surgery. A high vascularization of spinal epidural hemangiomas may result in an unexpected surgical situation in the case of preoperative misinterpretation.
In the current case, we report a case of spinal epidural hemangiomas mimicking sequestrated lumbar disc herniation.
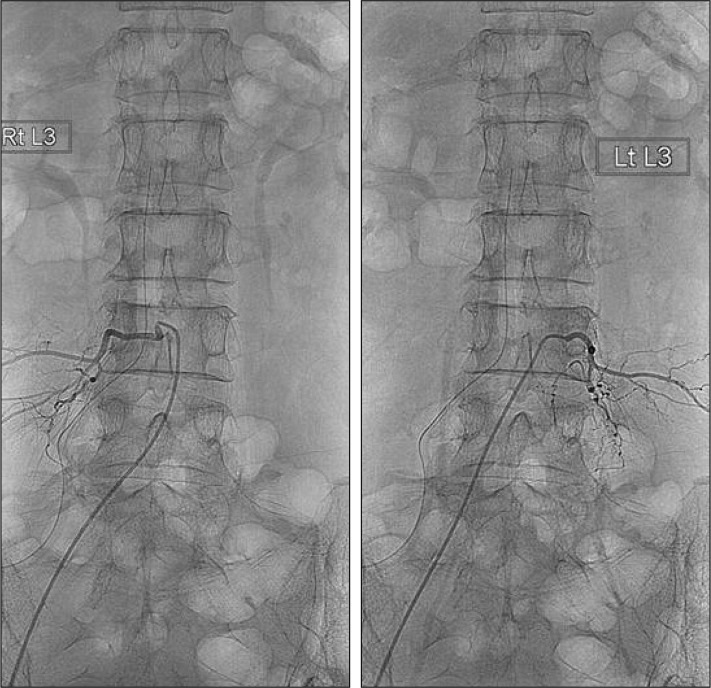
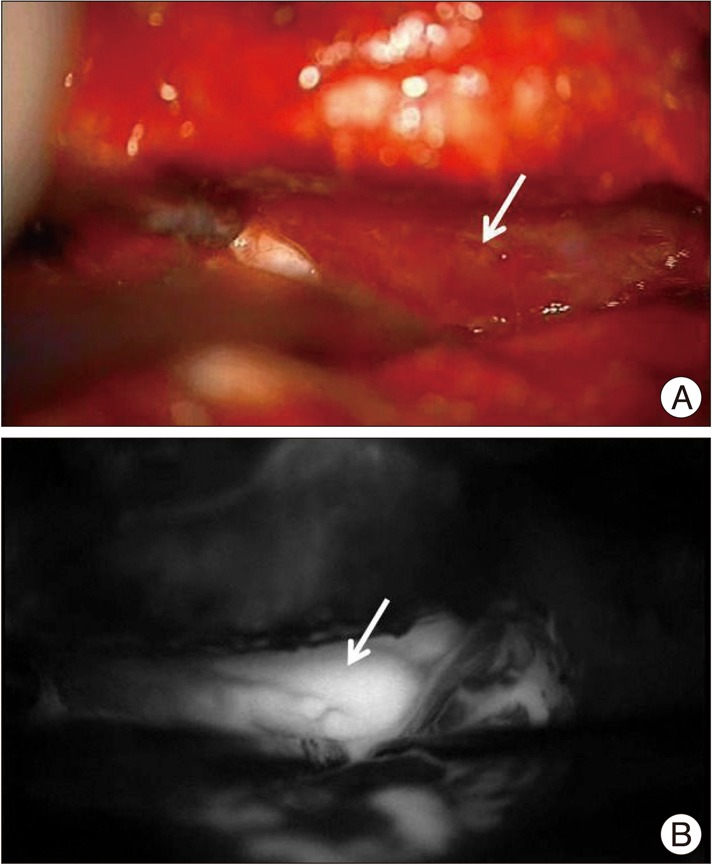
A 51-year-old woman presented with a 3-week history of lower back pain with right anterior thigh numbness. Her symptoms persisted despite conservative treatments. The patient had a magnetic resonance imaging (MRI) at a local hospital which revealed a lesion at the L3 level, located in the ventral epidural space and connected with L3/4 protruded disc material that demonstrated a heterogeneous signal at T2 weighted images and an iso- to low signal at T1 weighted image (T1-WI). The lesion became enhanced at sagittal T1-WI with contrast (Fig. 1). Based on a presumed diagnosis of a ruptured disc with possible sequestration or granulation tissue formation, the patient underwent surgery. A right hemilamincetomy of L3 was performed, and a retracting thecal sac revealed a highly engorged vascular structure. When the structure was discovered, the surgery was stopped for further evaluation. A spinal angiography was performed but no abnormal finding was observed (Fig. 2). Due to continued patient discomfort second surgery was performed. Near-infrared indocyanine green videoangiography (ICG-VA) showed a delayed mass filling. Coagulation of the vascular supply and en bloc removal was performed (Fig. 3). Histological examination revealed a vascular lesion composed of small to medium sized veins with irregular calibers, which is consistent with an arteriovenous hemangioma (Fig. 4). The patient's postoperative recovery was uneventful and her pain improved.
The typical symptoms of epidural lesions other than disc herniation of the lumbar region are low back pain or radiculopathy which are indistinguishable from the clinical symptoms of disc herniation diseases. Moreover, spinal epidural hemangiomas are very rare. Most spinal epidural hemangiomas that have been previously reported were of the cavernous type. Also, spinal epidural hemangiomas constitute approximately 4% of all epidural tumors and 12% of all intraspinal hemangiomas4).
The differential diagnosis for spinal epidural hemangiomas before surgery included schwannoma, lymphoma, meningioma, angiolipoma, disk herniation, synovial cysts, granulomatous infection, pure epidural hematoma, and extramedullary hematopoiesis9,12). Most epidural hemangiomas described in the literature were exclusively cavernous hemangiomas1,2,7). These differ from spinal epidural hemangioma form in terms of pathology. The cavernous type displays histologically with large number of sinusoidal channels in collagenous tissue7), whereas the arteriovenous type shows with a cluster of abnormal arteries and veins and vessel walls containing elastin, and smooth muscle5).
A complete surgical en bloc removal is the treatment of choice for spinal epidural hemangiomas with mass effect because of the excessive vascularity of hemangioma, piece to piece resection should be avoided6). An indocyanine green videoangiography can help surgeons understand the vasculature surrounding the mass and facilitate the en bloc removal of the hemangioma. Fluorescence angiography with indocyanine green provides real-time information regarding the patency of vessels. An ICG-VA enhances the flow direction delineation capability, flow velocity and sequence of dye filling in different components of complex spinal vascular lesions3).
Due to the high vascularization of hemangiomas, a misinterpretation may result in unexpected intraoperative hemorrhage. The incomplete surgical removal of a spinal hemagioma because of diffuse bleeding or minimal exposure during disk surgery might result in the persistence of clinical symptoms or recurrence. Reoperation for remnant or recurrent spinal hemangioma is very difficult due to peridural or periradicular adhesion and unclear margins; as a result, complete resection cannot be guaranteed. Therefore, proper preoperative planning and complete resection during the operation is essential. For this, a preoperative suspicion of spinal hemangioma is important8).
As in our case, obscure radiologic findings make diagnosis difficult. An angiography needs to be considered to distinguish spinal epidural hemangiomas from disc herniation. But, like this case, an angiography may not always confirm the diagnosis of an artriovenous hemangioma. Clinicians should be aware that an angiography cannot provide conclusive evidence of the presence of an antriovenous hemangioma.
References
1. Aoyagi N, Kojima K, Kasai H. Review of spinal epidural cavernous hemangioma. Neurol Med Chir (Tokyo). 2003; 43:471–475. discussion 476. PMID: 14620197.

2. Caruso G, Galarza M, Borghesi I, Pozzati E, Vitale M. Acute presentation of spinal epidural cavernous angiomas : case report. Neurosurgery. 2007; 60:E575–E576. discussion E576. PMID: 17327768.
3. Colby GP, Coon AL, Sciubba DM, Bydon A, Gailloud P, Tamargo RJ. Intraoperative indocyanine green angiography for obliteration of a spinal dural arteriovenous fistula. J Neurosurg Spine. 2009; 11:705–709. PMID: 19951023.

4. Feider HK, Yuille DL. An epidural cavernous hemangioma of the spine. AJNR Am J Neuroradiol. 1991; 12:243–244. PMID: 1902020.
5. Graziani N, Bouillot P, Figarella-Branger D, Dufour H, Peragut JC, Grisoli F. Cavernous angiomas and arteriovenous malformations of the spinal epidural space : report of 11 cases. Neurosurgery. 1994; 35:856–863. discussion 863-864. PMID: 7838334.
6. Hong SP, Cho DS, Kim MH, Shin KM. Spinal epidural cavernous hemangioma simulating a disc protrusion : a case report. J Korean Neurosurg Soc. 2003; 33:509–511.
7. Jo BJ, Lee SH, Chung SE, Paeng SS, Kim HS, Yoon SW, et al. Pure epidural cavernous hemangioma of the cervical spine that presented with an acute sensory deficit caused by hemorrhage. Yonsei Med J. 2006; 47:877–880. PMID: 17191320.

8. Lee JW, Cho EY, Hong SH, Chung HW, Kim JH, Chang KH, et al. Spinal epidural hemangiomas : various types of MR imaging features with histopathologic correlation. AJNR Am J Neuroradiol. 2007; 28:1242–1248. PMID: 17698523.

9. Minh NH. Cervicothoracic spinal epidural cavernous hemangioma : case report and review of the literature. Surg Neurol. 2005; 64:83–85. discussion 85. PMID: 15993196.

10. Raabe A, Beck J, Gerlach R, Zimmermann M, Seifert V. Near-infrared indocyanine green video angiography : a new method for intraoperative assessment of vascular flow. Neurosurgery. 2003; 52:132–139. discussion 139. PMID: 12493110.

11. Raabe A, Nakaji P, Beck J, Kim LJ, Hsu FP, Kamerman JD, et al. Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. J Neurosurg. 2005; 103:982–989. PMID: 16381184.

12. Shin JH, Lee HK, Rhim SC, Park SH, Choi CG, Suh DC. Spinal epidural cavernous hemangioma : MR findings. J Comput Assist Tomogr. 2001; 25:257–261. PMID: 11242225.
13. Woitzik J, Horn P, Vajkoczy P, Schmiedek P. Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green videoangiography. J Neurosurg. 2005; 102:692–698. PMID: 15871512.

14. Woitzik J, Peña-Tapia PG, Schneider UC, Vajkoczy P, Thomé C. Cortical perfusion measurement by indocyanine-green videoangiography in patients undergoing hemicraniectomy for malignant stroke. Stroke. 2006; 37:1549–1551. PMID: 16645136.

Fig. 1
A spine MR image (at present). A and D : T2 wighted image. B and E : T1 weighted image. C and F : T1 enhanced image. The figures show a L3 level posterior epidural space ovoid shape enhancing lesion with heterogeneous T2 high/low SI and T1 iso to low signal intensity.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download