Abstract
Objective
We compared the radiological and clinical outcomes between patients who underwent posterior fixation alone and supplemented with fusion following the onset of thoracolumbar burst fractures. In addition, we also evaluated the necessity of posterolateral fusion for patients treated with posterior pedicle screw fixation.
Methods
From January 2007 to December 2009, 46 consecutive patients with thoracolumbar burst fracture were included in this study. On the basis of posterolateral fusion, we divided our patients into the non-fusion group and the fusion group. The radiological assessment was performed according to the Cobb's method, and results were obtained at immediately, 3, 6, 12 months after surgery. The clinical outcomes were evaluated using the modified Mcnab criteria at the final follow-up.
Results
The demographic data and the mean follow-up period were similar between the two groups. Patients of both groups achieved satisfactory clinical outcomes. The mean loss of kyphosis correction showed that patients of both groups experienced loss of correction with no respect to whether they underwent the posterolateral fusion. There was no significant difference in the degree of loss of correction at any time points of the follow-up between the two groups. In addition, we also compared the effect of fixed levels (i.e., short versus long segment) on loss of correction between the two groups and there was no significant difference. There were no major complications postoperatively and during follow-up period.
The thoracolumbar spine fracture is one of the fractures that are encountered the most frequently in a clinical settings, and it is involved in almost 90% of all spinal injuries. In addition, 10% to 20% of them are burst fractures3,7,8). Some mechanical factors make the thoracolumbar spine susceptible to fracture following trauma. As a typical example, the thoracolumbar junction is a unique part of the spinal column where the spine undergoes the transition from the rigid kyphotic thoracic to mobile lordotic lumbar spine. This transitional anatomy renders it vulnerable to the trauma from a fall or a motor vehicle accident17,18,36). Thoracolumbar burst fractures usually occur due to a substantial axial loading force, which results in a compression failure of the anterior and middle spinal columns. There are some characteristic findings in the burst fractures; comminution of the injured vertebral body, progressive kyphotic deformity of the sagittal alignment, and canal compromise caused by retropulsion of the fracture segment, which may produce neurological deficits.
The management of thoracolumbar burst fractures still remains a challenging issue. Treatment varies ranging from the conservative management to various types of surgery. In addition, there is a great variability in the indications depending on surgeons. Furthermore, diverse treatments have been proposed for thoracolumbar burst fractures by different authors35,38). To date, many published studies have reported this issue. It remains unclear, however, which treatment modalities would be more effective between the conservative and surgical management. There is no established consensus regarding the ideal treatment modality37,38). Nevertheless, the overall management principles would be obvious that correct the deformity and instability, induce neurological recovery, allow early mobilization and return to work while incurring minimal complication. There are some major factors to consider when determining the optimal treatment; neurological status, spinal stability, degree of deformity, and associated injuries.
There is still a controversy as to the indications for operative treatment and types of stabilization procedure for the thoracolumbar burst fracture. But, the unstable fracture frequently requires surgical correction. Progressive neurological deterioration is generally considered an absolute indication for early surgery4,15). Other strong indications for surgical intervention include incomplete neurological deficit, more than 25° to 30° angle of kyphotic deformity, more than 50% loss of vertebral body height, more than 40% to 50% canal narrowing. The main goals of surgical treatment are to decompress the neural elements for neurological recovery and to restore the spine stability with a correction of the deformity. Surgical treatment provides immediate spinal stability and allows rapid mobilization. In addition, it also restores sagittal alignment, vertebral height and spinal canal dimension than cast or brace management more reliably33). Furthermore, it can also prevent complications of conservative management such as prolonged recumbency, pressure sores, residual kyphosis, belated neurologic impairment12).
Since Roy-Camille et al.28) used plates with pedicle screws for the fixation of thoracolumbar fracture in 1963, various techniques have been introduced, including anterior, posterior or combined (circumferential) fixation. Biomechanical data comparing these techniques have been described in several literatures13,16,32). Posterior transpedicular screw fixation allows immediate and superior stabilization of the spinal column. Nowadays, posterior short segment pedicle screw fixation (that is, involving one vertebra above and one below the fractured level) has become popular for management of thoracolumbar fractures.
Internal fixation with spinal fusion is a surgical treatment method that is generally accepted for patients with thoracolumbar fracture. Achievement of solid fusion leads to a lower risk of implant failure, while fusion components restrict segmental motion and increase stress on the adjacent levels1,2,6,26,39). Therefore, there is a constant debate on the necessity and reliability of fusion techniques for the treatment of the thoracolumbar burst fracture with the posterior instrumentation. Some clinical studies have demonstrated good treatment outcomes of the single instrumentation without fusion9,29,39).
In the present study, we retrospectively reviewed the clinical and radiological outcomes of 46 patients with thoracolumbar burst fracture, who underwent posterior pedicle screw fixation. Based on the posterolateral fusion, we divided them into two groups; the non-fusion group and fusion group. Then, our clinical series of patients randomly underwent the posterior fixation alone or were supplemented with posterolateral fusion. The preoperative characteristics, postoperative clinical outcomes and changes of kyphotic angle were compared between the two groups. The purpose of the present study was to evaluate the necessity of posterolateral fusion in patients with thoracolumbar burst fracture who were treated with the posterior pedicle screw fixation.
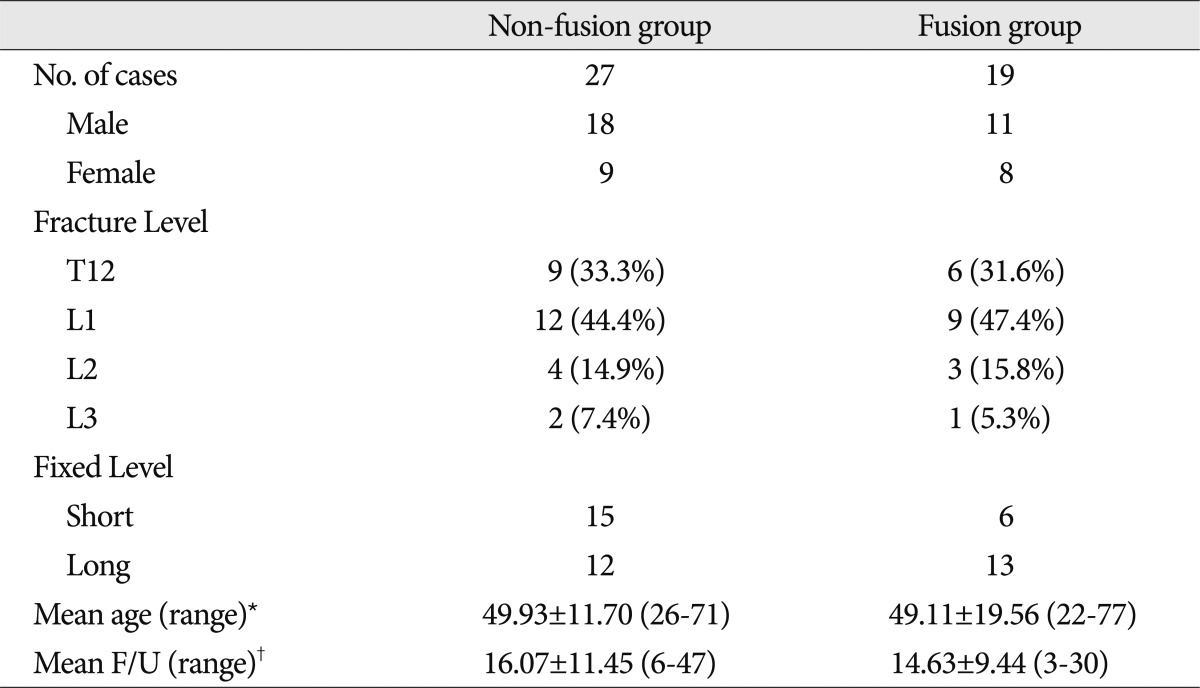
We retrospectively examined 59 consecutive patients with thoracolumbar burst fracture who were surgically treated between January 2007 to December 2009. Because 13 patients had no follow-up imaging after discharge, 46 patients were finally enrolled in the present study. All our clinical series of patients had a burst fractures from T12 to L3 level and underwent the posterior pedicle screw fixation. Based on the posterolateral fusion, our patients were divided into two groups; the non-fusion group and fusion group. The fusion groups was composed of 19 patients who underwent the posterior instrumentation with posterolateral fusion. But, there were 27 patients who received no fusion procedure. The indications for operative management were kyphotic deformity more than 30° and/or anterior vertebral height loss more than 50% as well as the involvement of more than two spinal columns. Patients randomly underwent the posterior fixation alone or were supplemented with posterolateral fusion. The number of operating segments (short versus long) was determined based on the pattern of fracture, the severity of kyphotic deformity and surgeons' preference.
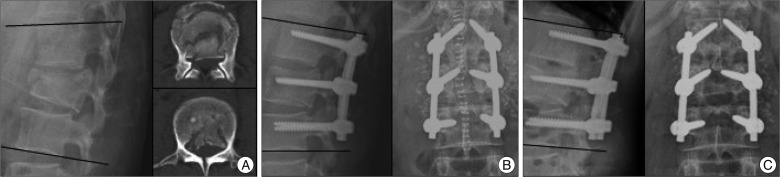
All the patients underwent a similar posterior pedicle screw fixation with no respect to the number of fixed levels (Fig. 1). Patients were placed in a prone position on a Wilson frame under general anesthesia. Pedicle screw fixation and reduction was performed under C-arm guidance. Some patients, who had more than 50% canal encroachment with/without progressive neurological deterioration, received laminectomy or another decompressive procedure. All patients underwent postural and instrumentation via screw-rod system reduction to achieve satisfactory reduction. Especially, monoaxial reduction screws (long lever-arm) were used and total laminectomy underwent in case of severe kyphotic deformity and/or canal encroachment. In the fusion group, simultaneous posterolateral fusion with bone graft was carried out after screw fixation (Fig. 2). The spine was exposed laterally to the tip of both transverse processes and it was cleaned from soft tissue and then decorticated to increase the recipient area with a high-speed burr. The bone graft materials, consisting of autologous local bone graft and/or synthetic bone substitutes, were placed in the decorticated area of the fixed segments. The local bone graft (LBG) was harvested from the decompression site and morselized into small corticocancellous pieces. Tricalcium phosphate or hydroxiapatite granule/strip type were used as bone substitutes solely or in combination with the LBG. From the postoperative day 2 or 3 on, our patients were recommended to use a custom-fitting thoracolumbosacral orthosis when sitting, standing or ambulating for three months postoperatively.
Patients were assessed with plain X-ray films on standing antero-posterior and lateral views. A radiographic follow-up was done at immediately after surgery, 3, 6 months, and 1 year after surgery. Parameters were measured by Cobb technique; the kyphosis on a lateral X-ray view from the superior endplate of the vertebral body one level above the injured vertebra body to the inferior endplate of the vertebral body one level below14). Clinical outcomes were evaluated using modified Mcnab criteria at a final follow-up.
The distribution of age, sex, and level of fracture were similar between the two groups (Table 1). The non-fusion group included 27 patients (18 males and 9 females), the fusion group 19 patients (11 males and 8 females), with no significant difference between the two groups in terms of male/female ratio (p=0.544, chi-square test). The mean age of patients was 49.93±11.70 years (range : 26-71) in the non-fusion group and 49.11±19.56 years (range : 22-77) in the fusion group (p=0.871, Welch's t-test). The fracture levels at T12 was 9 cases; L1, 12 cases; L2, 4 cases, and L3, 2 cases in the non-fusion group. The fusion group had T12, 6 cases; L1, 9 cases, L2, 3 cases, and L3, only 1 case (p=0.802, Fisher's exact test). The number of fixed levels in terms of short versus long was comparable in both groups (p=0.108, chi-square test). In the non-fusion group, 15 patients underwent short segment fixation while long segment fixation was performed in 12 patients. Whereas in the fusion group, these numbers were 6 and 13, respectively. The average follow-up period was also similar in both groups, 16.07±11.45 months (range : 6-47) and 14.63±9.44 months (range : 3-30) in the non-fusion and fusion group, respectively (p=0.885, Mann-Whitney U test) (Table 1). The statistical significance was not exist between the two groups (p>0.05).
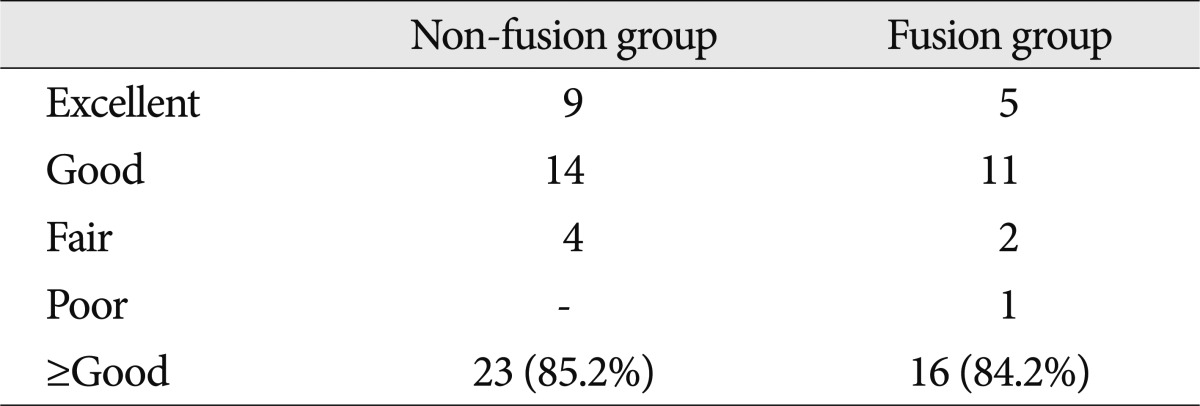
Patients of both groups achieved satisfactory clinical outcomes by modified Mcnab criteria. The results showed that 9 patients had excellent and 14 patients had good outcome in the non-fusion group; 5 patients and 11 patients in the fusion group, respectively. Therefore, the proportion of patients whose treatment outcomes were good or better was 23/27 (85.2%) in the non-fusion group and 16/19 (84.2%) in the fusion group. This indicated that there were no significant differences in clinical outcomes between the two groups (p=0.714, Fisher's exact test) (Table 2).
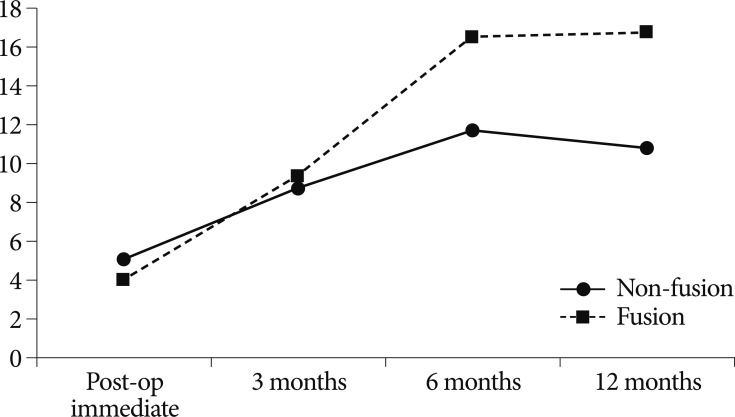
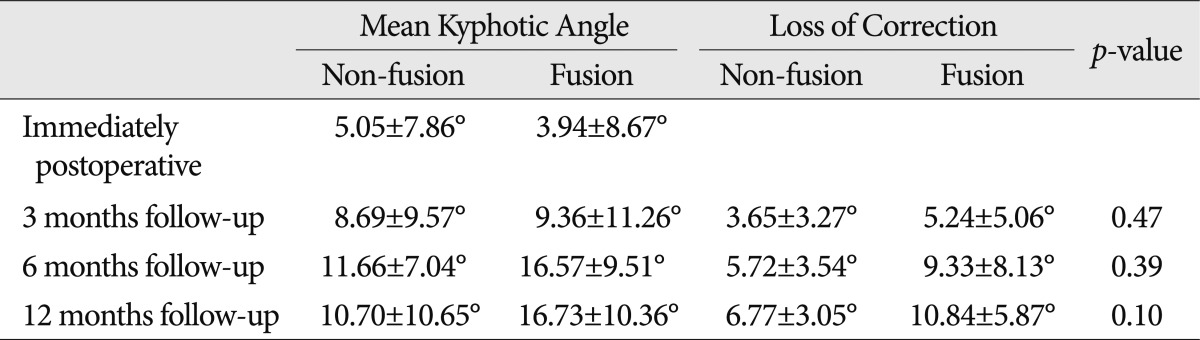
The mean kyphotic angle at the time of immediate postoperative was 5.05±7.86° (range : -17.62° to 17.93°) in the non-fusion group and 3.94±8.67° (range : -19.67 to 13.59°) in the fusion group. The follow-up kyphotic angles were assessed at the time of 3, 6 and 12 months after surgery (Fig. 3). The average angle at each follow-up period was as follows : which increased to 8.69±9.57° at 3 months follow-up; 6 months, 11.66±7.04°; 12 months, 10.70±10.65° in the non-fusion group and 3 months, 9.36±11.26°; 6 months, 16.57±9.51°; 12 months, 16.73±10.36° in the fusion group (Table 3). Also, the mean loss of kyphosis correction was evaluated and demonstrated in Table 3, which was 3.65±3.27°, 5.72±3.54°, and 6.77±3.05° at each follow-up period in the non-fusion group. In the fusion group, the average kyphotic angle was increased 5.24±5.06°, 9.33±8.13°, and 10.84±5.87°, respectively. These results demonstrated that loss of correction progressed in both groups, regardless of posterolateral fusion. The difference was not significant between the two groups at any time points of the follow-up (p>0.05, Mann-Whitney U test) (Table 3).
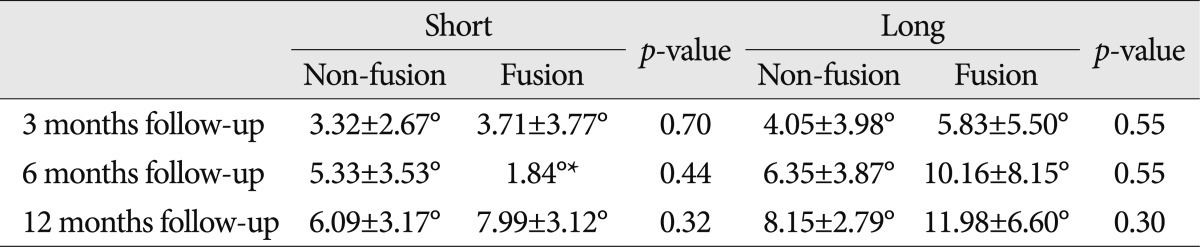
In addition, we also compared the effect of fixed levels (i.e., short versus long) on the loss of kyphosis correction between the two groups (Table 4). The mean loss of correction in 21 patients with posterior short segment pedicle screw fixation were not significantly different according to posterolateral fusion (p>0.05, Mann-Whitney U test). The results at each follow-up period were as follows : 15 patients in the non-fusion group, the average loss of correction was 3.32±2.67° at 3 months follow-up; 6 months, 5.33±3.53°; 12 months, 6.09±3.17° and 3 months, 3.71±3.77°; 6 months, 1.84°; 12 months, 7.99±3.12° in the fusion group. Similarly, 25 patients who underwnet posterior long segment pedicle screw fixation showed no statistical difference between non-fusion and fusion at any follow-up period (p>0.05, Mann-Whitney U test). The corresponding values were 4.05±3.98°, 6.35±3.87°, and 8.15±2.79° in the non-fusion group while 5.83±5.50°, 10.16±8.15°, and 11.98±6.60° in the fusion group, respectively.
There were no cases of major complication such as wound infection, cerebrospinal fluid leakage, postoperative neurological deficit or hardware failure. During the follow-up period, there were no patients who underwent revision surgery or that for the removal of instrument.
Thoracolumbar burst fractures are most common in patients with spine injuries. The most commonly utilized system for classification of thoracolumbar fractures is presented by Denis10). According to the Denis 3-column concept, burst fractures consist of anterior and middle columns injury with retropulsion of bone fragments into the spinal canal, which is the radiographic hallmark22,23,41). In addition, McAfee et al.20) distinguished an unstable burst fracture from stable burst fracture based on the disruption of the posterior elements.
Although a substantial number of literatures have reported the treatment of thoracolumbar fractures, it still remains controversial. It is generally known that unstable burst fractures require surgical management. Since Roy-Camille et al.28) first introduced the plates with pedicle screw fixation, various operative techniques have been developed. Thereafter, Dick et al.11) used "fixateur interne" for the internal fixation. Since then, posterior short segment pedicle screw fixation has become the most popular method for the surgical management of thoracolumbar fractures. As compared with a conventional long segment fixation, short segment constructs provide the advantage of saving motion segments19,27,29,34,39). Furthermore, Tezeren and Kuru34) reported that there was no significant difference in the clinical outcome between the two methods. Despite the superiority of this method, many surgeons have reported that an early implant failure and a loss of the correction are the most important disadvantages16,21,30).
In the current study, 21 patients underwent a posterior short segment pedicle screw fixation with or without posterolateral fusion. Even though short segment fixation could not avoid the loss of kyphosis correction, there were no instances of hardware failure in the present study. Besides, clinical outcomes according to the modified Mcnab criteria, above grade 'good' were observed in 17 patients (80.1%), which was not significantly different from that of the long segment fixation (22 of 25, 88.0%). Most clinicians believe that kyphotic deformity of the thoracolumbar spine precipitate poor clinical outcomes, but the relationship between them is unclear. Some authors advocated that there is no proven association between kyphosis and back pain or functional impairment5,24,40). Likewise, the present study showed satisfactory clinical outcomes in spite of correction loss.
Traditional standard concept of surgical treatment for spinal fracture includes a concurrent internal fixation and a fusion method. To date, the internal fixation devices have greatly facilitated the management of thoracolumbar fractures. But if a bone fusion could not be achieved, the instrumentation eventually would be fatigued and failed. Solid fusion is well known to decrease the risk of hardware failure, but it restrains the spinal motion permanently and increases stress on the adjacent levels1,2,6,26,39). Consequently, the necessity of fusion as a supplement to instrumentation for the treatment of thoracolumbar burst fractures is always controversial.
To our knowledge, there are only a few studies that have reported good clinical results of pedicle screw fixation without fusion for the treatment of thoracolumbar burst fractures. Sanderson et al.29) conducted a retrospective study of 28 patients who underwent a short segment screw fixation without fusion. According to these authors, there was no significant correlation between the radiological parameters and clinical outcomes. They considered that a routine posterior or posterolateral fusion would be unnecessary in the operative management of thoracolumbar burst fracture. Wang et al.39) prospectively compared the clinical results between fusion and non-fusion groups with short segment posterior fixation (28 and 30 patients, respectively). They found better perioperative parameters in the non-fusion group, and showed that there were no significant differences in the results of the radiological and functional assessment between the two groups. The short-term results of short segment fixation without fusion were satisfactory in that study. In a recently published paper, Dai et al.9) reported the long-term results of a prospective randomized trial involved 73 patients who underwent a posterior short segment screw fixation with or without posterolateral fusion (37 and 36 patients, respectively). These authors reported that there were no significant differences in the radiographic or clinical outcomes between the two groups, thus suggesting that posterolateral bone graft would not be mandatory.
Consistently with previous studies, the current study showed that loss of kyphosis correction was not significantly different between the non-fusion group and the fusion group. The result of radiological assessment demonstrated that loss of correction progressed in both groups, regardless of posterolateral fusion. Furthermore, the loss of correction was compared under short versus long segment fixation and there was no significant difference between the non-fusion group and fusion group. Satisfactory clinical outcomes, 'excellent' or 'good' according to modified Mcnab criteria, were similarly observed in both groups and also there was no statistically significant difference between the two groups.
The variables that affect the attainment of spinal fusion are complex and incompletely understood. Bone grafting is one of the most important factors in fusion surgery for the thoracolumbar fractures. There are many different types of bone graft, autologous iliac crest bone graft is considered the gold standard. However, harvesting iliac crest bone leads to considerable donor site morbidity, such as risk of infection, hematoma, fracture, wound healing problems, and donor site pain. To avoid these complications, local bone graft and various bone graft substitutes have been used in posterolateral fusion. Controlled trials have demonstrated that posterolateral fusion with local bone graft may yield similar clinical and fusion outcomes as iliac crest bone graft25,31). Synthetic bone graft substitutes are often used in spinal fusion surgery and deemed to be efficient based on their osteoconductive properties. When combined with bone marrow aspirate or used as an extender for autologous bone graft, they are useful biomaterials for bone fusion. In the present study, patients of the fusion group underwent posterolateral fusion with autologous local bone graft and/or synthetic bone substitutes.
However, performing fusion techniques, without regard to graft materials or methods, extend the operating time and increase the blood loss. Particularly in posterolateral fusion, an extensive surgical soft tissue stripping would be required to prepare the bed for the graft, and thus the aforementioned disadvantages become more apparent. In addition, fusion methods result in a permanent loss of the segmental motion and long-term adjacent level disease1,2,6,26). Therefore, the spinal fusion has many drawbacks. In the current study, we addressed the serious question of whether a simultaneous fusion would be necessary when treating thoracolumbar burst fractures with a posterior pedicle screw fixation.
There are some limitations in our study. The number of patients included in this retrospective study may be too small for a proper statistical analysis. In addition, the follow-up period was relatively shorter as compared with previous studies. Henceforth, further long term follow-up studies in a lager patient population are warranted to generalize our results.
In this study, we retrospectively compared the radiological and clinical outcomes between the two groups of patients who underwnet posterior pedicle screw fixation with or without posterolateral fusion for the treatment of thoracolumbar burst fractures. The present study demonstrated that there were no significant differences in the kyphosis correction and clinical outcomes between the two groups. Posterior pedicle screw fixation alone yielded satisfactory results that are equivalent to those of supplemented with posterolateral fusion. Futhermore, posterolateral fusion has many disadvantages such as permanent loss of segmental motion, long-term adjacent level disease and technique-related complications (i.e., blood loss, operating time, hospitalization period, etc.). Admitting that further studies are warranted, we suggest that posterolateral fusion may be unnecessary for patients with thoracolumbar burst fractures who underwent posterior pedicle screw fixation.
References
1. Aebi M, Etter C, Kehl T, Thalgott J. Stabilization of the lower thoracic and lumbar spine with the internal spinal skeletal fixation system. Indications, techniques, and first results of treatment. Spine (Phila Pa 1976). 1987; 12:544–551. PMID: 3660081.

2. Aiki H, Ohwada O, Kobayashi H, Hayakawa M, Kawaguchi S, Takebayashi T, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 2005; 10:490–495. PMID: 16193361.

3. Benson DR, Burkus JK, Montesano PX, Sutherland TB, McLain RF. Unstable thoracolumbar and lumbar burst fractures treated with the AO fixateur interne. J Spinal Disord. 1992; 5:335–343. PMID: 1520993.

4. Bohlman HH. Treatment of fractures and dislocations of the thoracic and lumbar spine. J Bone Joint Surg Am. 1985; 67:165–169. PMID: 3881446.

5. Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine (Phila Pa 1976). 1993; 18:971–976. PMID: 8367784.

6. Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation : a minimum 5-year follow-up. Spine (Phila Pa 1976). 2007; 32:2253–2257. PMID: 17873819.

7. Crawford NR, Brantley AG, Dickman CA, Koeneman EJ. An apparatus for applying pure nonconstraining moments to spine segments in vitro. Spine (Phila Pa 1976). 1995; 20:2097–2100. PMID: 8588165.

8. Crawford NR, Dickman CA. Construction of local vertebral coordinate systems using a digitizing probe. Technical note. Spine (Phila Pa 1976). 1997; 22:559–563. PMID: 9076889.

9. Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009; 91:1033–1041. PMID: 19411450.

10. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8:817–831. PMID: 6670016.

11. Dick W, Kluger P, Magerl F, Woersdörfer O, Zäch G. A new device for internal fixation of thoracolumbar and lumbar spine fractures : the 'fixateur interne'. Paraplegia. 1985; 23:225–232. PMID: 3900882.

12. Domenicucci M, Preite R, Ramieri A, Ciappetta P, Delfini R, Romanini L. Thoracolumbar fractures without neurosurgical involvement : surgical or conservative treatment? J Neurosurg Sci. 1996; 40:1–10. PMID: 8913955.
13. Eichholz KM, Hitchon PW, From A, Rubenbauer P, Nakamura S, Lim TH, et al. Biomechanical testing of anterior and posterior thoracolumbar instrumentation in the cadaveric spine. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004; 1:116–121. PMID: 15291031.

14. Enad JG, Slakey JB, McNulty PS. Measurement of thoracolumbar kyphosis after burst fracture : evaluation of intraobserver, interobserver, and variability of 4 measurement methods. Am J Orthop (Belle Mead NJ). 2008; 37:E60–E63. PMID: 18535682.
15. Ferguson RL, Allen BL Jr. An algorithm for the treatment of unstable thoracolumbar fractures. Orthop Clin North Am. 1986; 17:105–112. PMID: 3945473.

16. Gurwitz GS, Dawson JM, McNamara MJ, Federspiel CF, Spengler DM. Biomechanical analysis of three surgical approaches for lumbar burst fractures using short-segment instrumentation. Spine (Phila Pa 1976). 1993; 18:977–982. PMID: 8367785.

17. Kim NH, Lee HM, Chun IM. Neurologic injury and recovery in patients with burst fracture of the thoracolumbar spine. Spine (Phila Pa 1976). 1999; 24:290–293. discussion 294. PMID: 10025025.

18. Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine (Phila Pa 1976). 2001; 26:88–99. PMID: 11148651.

19. Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976). 2007; 32:1503–1507. PMID: 17572619.

20. McAfee PC, Yuan HA, Lasda NA. The unstable burst fracture. Spine (Phila Pa 1976). 1982; 7:365–373. PMID: 7135069.

21. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993; 75:162–167. PMID: 8423176.

22. Meves R, Avanzi O. Correlation between neurological deficit and spinal canal compromise in 198 patients with thoracolumbar and lumbar fractures. Spine (Phila Pa 1976). 2005; 30:787–791. PMID: 15803082.

23. Mohanty SP, Venkatram N. Does neurological recovery in thoracolumbar and lumbar burst fractures depend on the extent of canal compromise? Spinal Cord. 2002; 40:295–299. PMID: 12037711.

24. Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976). 1993; 18:955–970. PMID: 8367783.
25. Ohtori S, Suzuki M, Koshi T, Takaso M, Yamashita M, Yamauchi M, et al. Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft : a prospective, randomized study with a 2-year follow-up. Eur Spine J. 2011; 20:635–639. PMID: 21165658.

26. Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976). 2004; 29:1535–1540. PMID: 15247575.

27. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures : a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000; 25:1157–1170. PMID: 10788862.

28. Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986; 203:7–17. PMID: 3955999.

29. Sanderson PL, Fraser RD, Hall DJ, Cain CM, Osti OL, Potter GR. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999; 8:495–500. PMID: 10664310.

30. Sasso RC, Cotler HB. Posterior instrumentation and fusion for unstable fractures and fracture-dislocations of the thoracic and lumbar spine. A comparative study of three fixation devices in 70 patients. Spine (Phila Pa 1976). 1993; 18:450–460. PMID: 8470006.

31. Sengupta DK, Truumees E, Patel CK, Kazmierczak C, Hughes B, Elders G, et al. Outcome of local bone versus autogenous iliac crest bone graft in the instrumented posterolateral fusion of the lumbar spine. Spine (Phila Pa 1976). 2006; 31:985–991. PMID: 16641774.

32. Shono Y, McAfee PC, Cunningham BW. Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine (Phila Pa 1976). 1994; 19:1711–1722. PMID: 7973965.
33. Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, et al. Treatment of traumatic thoracolumbar spine fractures : a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976). 2006; 31:2881–2890. PMID: 17139218.

34. Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture : short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005; 18:485–488. PMID: 16306834.
35. Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine (Phila Pa 1976). 2003; 28:2459–2465. PMID: 14595164.

36. Vaccaro AR, Nachwalter RS, Klein GR, Sewards JM, Albert TJ, Garfin SR. The significance of thoracolumbar spinal canal size in spinal cord injury patients. Spine (Phila Pa 1976). 2001; 26:371–376. PMID: 11224884.

37. van der Roer N, de Lange ES, Bakker FC, de Vet HC, van Tulder MW. Management of traumatic thoracolumbar fractures : a systematic review of the literature. Eur Spine J. 2005; 14:527–534. PMID: 15690209.

38. Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine : a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976). 2004; 29:803–814. PMID: 15087804.

39. Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine? : a prospective, randomized study. Spine (Phila Pa 1976). 2006; 31:2646–2652. discussion 2653. PMID: 17077731.

40. Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar "burst" fractures treated conservatively : a long-term follow-up. Spine (Phila Pa 1976). 1988; 13:33–38. PMID: 3381135.

41. Wilcox RK, Boerger TO, Allen DJ, Barton DC, Limb D, Dickson RA, et al. A dynamic study of thoracolumbar burst fractures. J Bone Joint Surg Am. 2003; 85:2184–2189. PMID: 14630851.

Fig. 1
A 48-year-old female was sustained an injury due to a motor vehicle. She was diagnosed with burst fracture of L1 and underwent a posterior short segment screw fixation including the index level (that is, the level of the burst fracture). A : The preoperative lateral view and CT scan show 17.9° kyphotic angle and 51% canal encroachment, respectively. B : The immediate postoperative lateral view shows that kyphotic angle was decreased to 13.6°. C : At a 1-year follow-up, the lateral view shows 18.1° kyphotic angle.
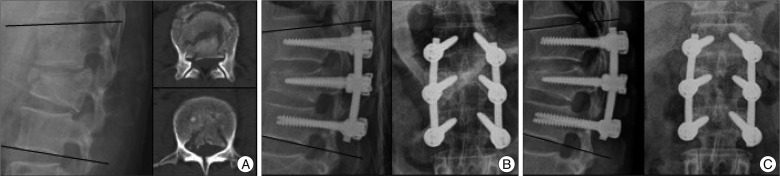
Fig. 2
A 42-year-old male fell backwards from height of 3 meters. He was diagnosed with burst fracture of L2 and underwent total laminectomy with posterior short segment screw fixation involving the index level. Instrumentations were supplemented with posterolateral fusion. A : The preoperative lateral view and CT scan show 10.1° kyphotic angle and 62% canal encroachment, respectively. B : The immediate postoperative lateral view shows 12.3° lordotic angle and AP view reveals that bone graft materials were placed in the transverse process of fixed segments. C : At a 1-year follow-up, the lateral view shows 6.2° lordotic angle and the AP view demonstrates that bone grafts were partially absorbed (progression of bone fusion).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download