Abstract
Objective
Chronic neck or back pain can be managed with various procedures. Although these procedures are usually well-tolerated, a variety of side effects have been reported. In this study we reviewed cases of unexpected temporary adverse events after blocks and suggest possible causes.
Methods
We reviewed the records of patients treated with spinal pain blocks between December 2009 and January 2011. The types of blocks performed were medial branch blocks, interlaminar epidural blocks and transforaminal epidural blocks. During the first eight months of the study period (Group A), 2% mepivacaine HCL and triamcinolone was used, and during the last six months of the study period (Group B), mepivacaine was diluted to 1% with normal saline.
Results
There were 704 procedures in 613 patients. Ten patients had 12 transient neurologic events. Nine patients were in Group A and one was in Group B. Transient complications occurred in four patients after cervical block and in eight patients after lumbar block. Side effects of lumbar spine blocks were associated with the concentration of mepivacaine (p<0.05). The likely causes were a high concentration of mepivacaine in five patients, inadvertent vascular injection in three patients, intrathecal leak of local anesthetics in one, and underlying conversion disorder in one.
Conclusion
Spinal pain blocks are a good option for relieving pain, but clinicians should always keep in mind the potential for development of inevitable complications. Careful history-taking, appropriate selection of the anesthetics, and using real-time fluoroscopy could help reduce the occurrence of adverse events.
Spinal pain is the most common of all chronic pain disorders and the lifetime prevalence of spinal pain has been reported to range from 54% to 80%1,3,8,12,34). There are neither conservative nor surgical interventions that provide definitive long-term improvement in chronic low back pain1,11,21,29). Conservative care of axial or radicular pain of the spine may include epidural or facetal administration of corticosteroids and local anesthetics. Techniques include interlaminar, transforaminal or caudal epidural injections and medial branch block (MBB)5,26,30).
Besides the well-known complications that may be permanent or fatal, transient adverse neurologic events of spinal pain blocks are encountered frequently. Although they are temporary, they are troublesome to the patients as well as to the pain physicians. We reviewed patients treated with pain block procedures at our institution with special focus on the cases experiencing temporary neurologic events and their possible causes.
We reviewed the records of patients who had neck and back pain and were treated with spinal pain blocks between December 2009 and January 2011. According to the cause of pain, the following pain blocks were performed by the same three physicians : MBB, interlaminar epidural block (ILEB), and transforaminal epidural block (TFEB). During the first eight months of the study period (Group A), MBB was done with 2 mL of 2% mepivacaine HCL (Reyon Pharm, Seoul, Korea) mixed with 8 mg (0.2 mL) of triamcinolone acetonide (Shinpoong Pharm, Seoul, Korea) injected into each target point. For TFEB, a mixture of 1 mL of 2% mepivacaine HCL and 40 mg (1 mL) of triamcinolone acetonide was used at each target point. For ILEB, a mixture of 1 mL of 2% mepivacaine HCL and 40 mg (1 mL) of triamcinolone acetonide was used. During the last six months of the study period (Group B), the procedures were performed by the same physicians using the same methods, but mepivacaine was diluted to 1% with normal saline because we had encountered motor paralysis in some patients after block procedures.
For TFEB or ILEB, usually 1 or 2 sites were selected and injection volume was 2 mL per site. For MBB, the procedures were performed at least 3 levels simultaneously and injection volume was minimum of 6 mL and maximum 16 mL. There was no case where both cervical and lumbar blocks were done at the same time.
All procedures were performed under fluoroscopy. All the cervical procedures were done in an operating room and lumbar procedures were performed either in an operating room or fluoroscopy suite. The frequency of temporary deficits by procedure type and treatment level was statistically compared using a chi-square test.
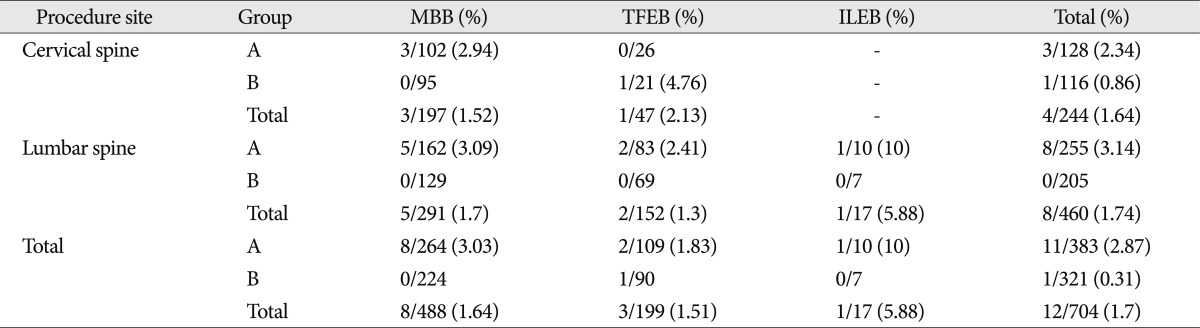
The records of 613 patients were reviewed, 352 in Group A and 261 in Group B. A total of 704 procedures were performed, 383 in Group A and 321 in Group B. The distribution of block procedures was 197 cervical MBBs, 291 lumbar MBBs, 152 lumbar TFEBs, 47 cervical TFEBs, and 17 lumbar ILEBs (Table 1). Of the 613 patients, 10 patients had 12 transient neurologic events (Table 2). Nine of these adverse events developed in Group A and one occurred in Group B.
In the cervical block cases, there were 113 patients in Group A, 96 in Group B. In the lumbar block cases, there were 233 patients in Group A, 147 in Group B. The patients who received cervical and lumbar block procedure 2 or more than 2 times were 6 and 18 in Group A and B. Two patients who had been received lumbar MBBB had suffered from repeated paraplegia (Table 2).
The recovery period was variable from ten minutes to two months. Except for the longest period of the patient with conversion disorder, the average duration to complete recovery was 66.6 minutes in cervical block cases. In lumbar block cases, it was 205 minutes. Usually they have recovered within 8 hours (Table 2).
In 704 cases, 89 cases had a history of previous surgery. Transient complications of the block procedures only occurred in patients without surgery history. So the incidence of complications associated with previous surgery do not have meaning (Table 3).
With respect to injected volume, in TFEB or ILEB case of Group A, the incidence of complication seems to have a tendency to rise according to drug volume. But, the difference did not reach statistical significance (p=0.315). In MBB of Group A, the incidence of complication did not show any tendency. In Group B, no difference was found related to injected volume (Table 4).
Looking at each site, four cases out of 244 cervical block cases (1.64%) and 8 cases out of 460 lumbar block cases (1.74%) showed transient deficits after the pain block, respectively (Table 2). In lumbar spine blocks, the incidence of side effects were closely related to the concentration of mepivacaine (p<0.05). However, in cervical spine blocks, the incidence of side effects did not seem to be related to the concentration of mepivacaine (p>0.05).
Cervical and lumbar TFEB yielded 2.13% and 1.3% of deficits in totals (Table 1). Cervical TFEB caused a higher frequency of transient deficits than the lumbar procedure; however, the difference did not reach statistical significance (p=0.055). ILEB was done only in the lumbar area, and one patient (5.88%) showed transient paraplegia. This side effect was not related to the concentration of mepivacaine (p>0.05).
In terms of the type of complication, motor paralysis developed in nine patients and respiratory depression developed in three patients. Other symptoms included chest discomfort, nausea, bradycardia, hypotension, mydriasis, impotence and fecal incontinence (Table 1). All of these patients recovered eventually. The probable causes of these temporary adverse effects were a high concentration of mepivacaine in five patients, inadvertent vascular injection in three patients, intrathecal leak of local anesthetics in one, and an underlying conversion disorder in one.
A 52-year-old woman (Case #2 in Table 1) came to the outpatient clinic complaining of pain radiating down her left arm. Cervical MRI obtained at the outpatient clinic showed herniated nucleus pulposus at the C4-5 level and ossification of the posterior longitudinal ligament at the C4-5-6 level. Cervical MBB at the left C4-5-6 was performed. Two milliliters of 2% mepivacaine HCL mixed with 8 mg (0.2 mL) of triamcinolone acetonide was injected at each level. After the procedure, the patient was moved to the recovery room. She complained of mild chest discomfort and respiratory difficulty. We checked her blood pressure and oxygen saturation and were reassured by her normal vital signs. A few minutes later, the recovery room nurse called for the CPR team. The patient's blood pressure and pulse were within the normal range, but she had severe respiratory depression. She required intubation and mechanical ventilation. The light reflex was intact, but quadriplegia was observed. Spontaneous respiration returned after thirty minutes of mechanical ventilation, and the quadriplegia improved gradually. After observation for the day, she was discharged without neurologic complications.
A 52-year-old man (Case #9 in Table 1) complained of right occipital headache and dizziness. He worked as a driver. He did not have any significant past medical history and his only regular medication was aspirin. He had tried taking medication for his occipital headache for years, but there was no improvement. A first C2 ganglion block was performed. Prior to the procedure, he underwent brain CT angiography and it was normal. Before the treatment, his blood pressure was 135/88 mm Hg and heart rate was 64 beats/min. To avoid complications of particulate steroids such as embolic infarction, only 1 mL of 2% mepivacaine was injected near the right C2 dorsal root. There was no improvement in symptoms and after 12 days, and an additional procedure was performed. Before the second procedure, his blood pressure was 128/90 mm Hg, heart rate was 65 beats/min and body temperature was 36.7℃. Using real-time fluoroscopy, a right C2 dorsal root ganglion block was performed. While attempting the block, the patient complained of his typical radiating pain to occipital area. Confirming that there was no vascular uptake after contrast media injection, the same drug as before was injected. The patient was stable during the procedure. As soon as we stepped into the recovery room, the patient complained of shortness of breath and right hemiparesis (motor grade II). Oxygen was administered and intravenous access was obtained. His vital signs were stable. Although alert, there was anisocoria in one pupil. Compared to the left, the right pupil was dilated. There were no other cranial nerve deficits. With preparation of intubation set and other emergency drugs, we observed the patient for 130 minutes. His pulse rate decreased to 49 beats/min for a moment, but soon recovered spontaneously. Finally, the symptoms all improved and he left the recovery room without neurologic deficit. However, when he came to the outpatient clinic a week later, he complained of impotence and fecal incontinence. These symptoms resolved spontaneously over two months, but he required some urologic medication.
A 34-year-old woman (Case #1 in Table 1) who was in a traffic accident two months prior to presentation visited the outpatient clinic because of right neck pain. To relieve the neck pain, cervical facet MBB at C3 to C7 was performed with a mixture of 10 mL of 2% mepivacaine and 2 mL of 40 mg triamcinolone. About 30 minutes after the injection, she reported chest discomfort and nausea. After that she rapidly developed quadriparesis, but showed stable respiration and blood pressure. Cervical spinal MRI was performed, but no abnormality was detected except for degenerative desiccation of the C5-6 disc. She required hospitalization in the neurosurgical ward. Three days later, she complained of dysphagia and showed mental obtundation. When we attempted to check the pupil size and light reflex, opening her eyelids was difficult because she was resisting; her eyeballs were deviated upwards, but it seemed like intentional deviation and the light reflexes were prompt. She was non-responsive to noxious stimuli on her face, neck, and upper and lower limbs. Deep tendon reflexes in the upper and lower extremities were symmetric and normoactive. Hoffmann or Babinski signs were not noted. Respiration, blood pressure and heart rate were stable. Brain MRI, including diffusion tensor images, was performed to differentiate organic brain lesions. It did not show any abnormalities. Four hours after mental obtundation, she awoke and was able to communicate with her mother by opening and closing her eyes. The consulting psychiatrist diagnosed her with a conversion disorder. A somatosensory-evoked potential study showed no electrophysiologic evidence of dysfunction. Physical therapy was begun. Two months of rehabilitation has improved her motor and sensory function. She complained of insomnia and abdominal discomfort without any motor or sensory disorder when she was discharged.
A case with temporary neurologic deficits after cervical transforaminal injection of local anesthetics was reported17) in which the patient had transient quadriparesis without respiratory depression for 20 minutes. The authors suggested the cause was inadvertent intra-arterial injection of drug17). There was also a reported case of transient tetraplegia after blockade of the cervical zygapophyseal joints14). Unguided injection 1% lidocaine was performed into the facet joints between the fifth and sixth cervical vertebrae. The patient developed weakness in all limbs, dissociated sensory loss and had difficulty breathing. Transient hypotension and bradycardia were also noted, but all symptoms resolved within 30 minutes. The authors discussed the arterial relationship surrounding the cervical zygapophyseal joints and hypothesized that an inadvertent uptake of the local anesthetics into the anterior spinal artery caused the deficit. In our Cases #2 and #3, judging from the type of block and the patients' symptoms, the cause was likely similar.
However, in Case #9, the cause of the deficits does not seem to be limited to arterial uptake. The signs and symptoms were compatible with toxicity of local anesthetics related to venous injection4). This case (#9) showed signs of hemianesthesia and cardiac effects. If these deficitsoccurred due to anterior spinal artery uptake, the neurologic signs would have been symmetric. If we had inadvertently punctured the adjacent vertebral artery, it should have been easily recognizable because of the large size and arterial pressure of the vertebral artery. We suspected that the profuse venous plexus around the C2 ganglion might have played some role in the deficits. We do not use particulate steroids for TFEB or ganglion blocks because it is well-known that particulate steroids can cause embolic aggregation and occlude vessels, leading to permanent neuronal infarction. In general, the greater the vascular supply of the tissue, the greater the absorption.
Radicular arterial and venous anatomy of the cervical spine is variable from person to person, and it is difficult to estimate the location even with real-time fluoroscopy. We cannot completely avoid the inadvertent intravascular uptake of the drugs. Clinicians should be aware that intravascular injection may always occur no matter how carefully the procedures are performed. Even if temporary, cervical block complications can be serious. Therefore, vital signs must be checked before and after the procedure and real-time monitoring is recommended during treatment. When performing these procedures around the cervical roots or ganglia, it would be best not to use steroids because arterial uptake can occur easily in these areas. Physicians must explain this risk to patients and caregivers for fully-informed consent.
Little is known about the relative importance of local anesthetic volume versus concentration for peripheral nerve blockade24,25,31,33) or for spinal pain blocks. The optimum dose of local anesthetics in spinal pain blocks is adjusted to prevent pain, minimize motor block, and prolong block duration. A study of the relative influence of local anesthetic volume and concentration on recovery room pain and motor paralysis in patients undergoing interscalene blocks for shoulder surgery has been reported10). This report suggested that when a large volume of local anesthetics (ropivacaine) was administered, the placement accuracy was less critical and motor block was associated with the local anesthetic concentration. In studies of sciatic nerve blocks, the authors concluded that administering a low volume and a high concentration of local anesthetic was associated with a shorter time to onset of complete sensory and motor block33) and a longer duration of analgesia31) than a larger volume and a lower concentration of local anesthetic. Individual patients may have different responses to the same dose of the same drug delivered in the same location. Needle-to-nerve proximity may also influence pain suppression or motor paralysis10). However, these results cannot be directly translated to spinal pain block procedures.
In our results, the incidence of transient deficits between Groups A and B was definitely different in lumbar pain block cases (p<0.05). The incidence of complications after the lumbar block procedure depended on the concentration of the drug. Motor paralysis was the most common symptom. Motor paralysis developed only in Group A. After the injection of 2% mepivacaine caused a temporary motor paralysis, two patients were switched to 1% mepivacaine for treatment in the same area, and the complications did not occur again. Those patients who experienced motor paralysis tended to show better pain outcomes; nevertheless dense motor paralysis was problematic. Clinicians should bear in mind that the concentration of local anesthetics can influence motor power.
Unlike the different concentration of the drug in Group A and B, the volume per injection site was set equal to 2 mL. A large number of patients had injection procedure in multiple levels. We analyzed to the relationship of total injected volume and incidence of complication but it did not show any meaningful difference.
The term conversion disorder (previously referred to as "hysterical neurosis") refers to functional or unexplained neurological deficits such as paralysis or somatosensory losses that are not explained by organic lesions in the nervous system15,22). It is usually a diagnosis of exclusion after all organic causes have been ruled out18). Hysterical conversion reactions can present as unexplained deafness, blindness, hemi- or paraplegia, seizures, or aphonia9,18,27). Most often, an underlying disorder such as depression or an overwhelming stressor has distorted the patient's coping mechanisms9,19,22,23). Recurrence rates are reported to be as high as 20% to 25%, and most recurrences are within the first year after diagnosis28). The highest recurrence rates and poorest outcomes of treatment tend to be found in individuals who are 30 to 50 years of age and those who have an underlying personality disorder at presentation, poor general health at presentation, and a long duration of symptoms before diagnosis2,7,32). This paralysis is occasionally found after spine surgery such as spinal cord stimulation13), lumbar disc surgery16) or trauma20). Chhibber and Lustik6) reported a patient who presented with leg paralysis after successful spinal anesthesia. Her neurological examination revealed the absence of voluntary movement with hyperesthesia and normal deep tendon reflexes in the affected extremity. The patient was discharged with the diagnosis of conversion disorder and later recovered after outpatient psychiatric treatment. Laraki et al.18) reported a case of bilateral lower extremity paralysis after epidural neurological examination revealed a loss of voluntary movement in the lower extremities with absent proprioception, vibratory sensation, and a patchy sensory loss bilaterally. However, all reflexes, anal tone, and the ability to urinate were intact. Likewise, this patient's symptoms were unexplainable and transient, suggesting a psychological etiology.
Before considering a psychological cause such as conversion disorder, all organic causes should be eliminated. Conversion disorder must be differentiated from malingering and factitious disorders. Unlike factitious and malingering, conversion disorders are manifested unconsciously with no evidence of any external gain.
Spinal pain blocks are a good option for relieving chronic spinal pain, but clinicians should always keep in mind the development of inevitable complications. Careful history taking to diagnose any underlying disorders, appropriate selection of the type and concentration of anesthetics, and using real-time fluoroscopy and proper suites for procedures could help reduce the adverse effects. The usual recovery time within 8 hours in our study may recommend an imaging study if the patients were not improved within that hour. Having a pre-procedural checklist, including obtaining vital signs and following meticulous informed consent procedures, is also critical to avoid medicolegal issues.
Acknowledgements
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A100054).
References
1. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, et al. Epidural steroids in the management of chronic spinal pain : a systematic review. Pain Physician. 2007; 10:185–212. PMID: 17256030.
2. Binzer M, Kullgren G. Motor conversion disorder. A prospective 2- to 5-year follow-up study. Psychosomatics. 1998; 39:519–527. PMID: 9819952.

3. Bot SD, van der Waal JM, Terwee CB, van der Windt DA, Schellevis FG, Bouter LM, et al. Incidence and prevalence of complaints of the neck and upper extremity in general practice. Ann Rheum Dis. 2005; 64:118–123. PMID: 15608309.
4. Bukwirwa DHW. Toxicity from Local Anaesthetic Drugs. p. 50–51. Update in anaesthesia No 101999.
5. Bush K, Hillier S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections : a prospective study with independent clinical review. Eur Spine J. 1996; 5:319–325. PMID: 8915637.

6. Chhibber AK, Lustik SJ. Unexpected neurologic deficit following spinal anesthesia. Reg Anesth. 1996; 21:355–357. PMID: 8837196.
7. Couprie W, Wijdicks EF, Rooijmans HG, van Gijn J. Outcome in conversion disorder : a follow up study. J Neurol Neurosurg Psychiatry. 1995; 58:750–752. PMID: 7608683.
8. Elliott AM, Smith BH, Hannaford PC, Smith WC, Chambers WA. The course of chronic pain in the community : results of a 4-year follow-up study. Pain. 2002; 99:299–307. PMID: 12237208.

9. Ford CV. Illness as a lifestyle. The role of somatization in medical practice. Spine (Phila Pa 1976). 1992; 17:S338–S343. PMID: 1440027.
10. Fredrickson MJ, Smith KR, Wong AC. Importance of volume and concentration for ropivacaine interscalene block in preventing recovery room pain and minimizing motor block after shoulder surgery. Anesthesiology. 2010; 112:1374–1381. PMID: 20460999.

11. Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis : updated Cochrane Review. Spine (Phila Pa 1976). 2005; 30:2312–2320. PMID: 16227895.
12. Guo HR, Tanaka S, Halperin WE, Cameron LL. Back pain prevalence in US industry and estimates of lost workdays. Am J Public Health. 1999; 89:1029–1035. PMID: 10394311.

13. Han D, Connelly NR, Weintraub A, Kanev P, Solis E. Conversion locked-in syndrome after implantation of a spinal cord stimulator. Anesth Analg. 2007; 104:163–165. PMID: 17179263.

14. Heckmann JG, Maihöfner C, Lanz S, Rauch C, Neundörfer B. Transient tetraplegia after cervical facet joint injection for chronic neck pain administered without imaging guidance. Clin Neurol Neurosurg. 2006; 108:709–711. PMID: 16102894.

15. Heruti RJ, Levy A, Adunski A, Ohry A. Conversion motor paralysis disorder : overview and rehabilitation model. Spinal Cord. 2002; 40:327–334. PMID: 12080460.

16. Hsieh MK, Chang CN, Hsiao MC, Chen WJ, Chen LH. Conversion paralysis after surgery for lumbar disc herniation. Spine (Phila Pa 1976). 2010; 35:E308–E310. PMID: 20395776.

17. Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anesthetic. Pain Med. 2004; 5:202–205. PMID: 15209975.

18. Laraki M, Orliaguet GA, Flandin C, Merckx J, Barrier G. Hysterical paraplegia as a cause of transient paraplegia after epidural anesthesia. Anesth Analg. 1996; 83:876–877. PMID: 8831338.

19. Leslie SA. Diagnosis and treatment of hysterical conversion reactions. Arch Dis Child. 1988; 63:506–511. PMID: 3389865.

20. Letonoff EJ, Williams TR, Sidhu KS. Hysterical paralysis : a report of three cases and a review of the literature. Spine (Phila Pa 1976). 2002; 27:E441–E445. PMID: 12394915.
21. Macario A, Pergolizzi JV. Systematic literature review of spinal decompression via motorized traction for chronic discogenic low back pain. Pain Pract. 2006; 6:171–178. PMID: 17147594.

22. Maue FR. Functional somatic disorders. Key diagnostic features. Postgrad Med. 1986; 79:201–210. PMID: 3945596.
23. Maurice-Williams RS, Marsh H. Simulated paraplegia : an occasional problem for the neurosurgeon. J Neurol Neurosurg Psychiatry. 1985; 48:826–831. PMID: 4031935.
24. Nakamura T, Popitz-Bergez F, Birknes J, Strichartz GR. The critical role of concentration for lidocaine block of peripheral nerve in vivo : studies of function and drug uptake in the rat. Anesthesiology. 2003; 99:1189–1197. PMID: 14576558.

25. Pippa P, Cuomo P, Panchetti A, Scarchini M, Poggi G, D'Arienzo M. High volume and low concentration of anaesthetic solution in the perivascular interscalene sheath determines quality of block and incidence of complications. Eur J Anaesthesiol. 2006; 23:855–860. PMID: 16834790.

26. Rowlingson JC, Kirschenbaum LP. Epidural analgesic techniques in the management of cervical pain. Anesth Analg. 1986; 65:938–942. PMID: 3017152.

27. Schwartz AC, Calhoun AW, Eschbach CL, Seelig BJ. Treatment of conversion disorder in an African American Christian woman : cultural and social considerations. Am J Psychiatry. 2001; 158:1385–1391. PMID: 11532721.

28. Silver FW. Management of conversion disorder. Am J Phys Med Rehabil. 1996; 75:134–140. PMID: 8630194.
29. Singh K, Ledet E, Carl A. Intradiscal therapy : a review of current treatment modalities. Spine (Phila Pa 1976). 2005; 30:S20–S26. PMID: 16138061.
30. Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain : a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000; 81:741–746. PMID: 10857517.

31. Smith BE, Siggins D. Low volume, high concentration block of the sciatic nerve. Anaesthesia. 1988; 43:8–11. PMID: 3344967.

32. Speed J. Behavioral management of conversion disorder : retrospective study. Arch Phys Med Rehabil. 1996; 77:147–154. PMID: 8607738.
33. Taboada Muñiz M, Rodríguez J, Bermúdez M, Valiño C, Blanco N, Amor M, et al. Low volume and high concentration of local anesthetic is more efficacious than high volume and low concentration in Labat's sciatic nerve block : a prospective, randomized comparison. Anesth Analg. 2008; 107:2085–2088. PMID: 19020163.
34. Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults : a review of the literature. Pain. 1998; 77:231–239. PMID: 9808348.

Table 2
Summary of patients with temporary neurologic events

Case #1,2,3,4,5,6,7,8,10-2% mepivacaine HCL, Case #9-1% mepivacaine HCL. MBB : medial branch block, HNP : herniated nucleus pulposus, bi. : bilateral, Fx : fracture, TFEB : transforaminal epidural block, ILEB : interlaminar epidural block, Op. : operation, OPLL : ossification of the posterior longitudinal ligament




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download