Abstract
Objective
Spinal cord hemangioblastomas are rare tumors. Despite their benign, slow-growing nature, they can cause severe neurological consequences. The purpose of this study was to evaluate variable factors, including clinical features, tumor findings, the extent of resection, and its recurrence or progression, which determine postoperative functional outcomes.
Methods
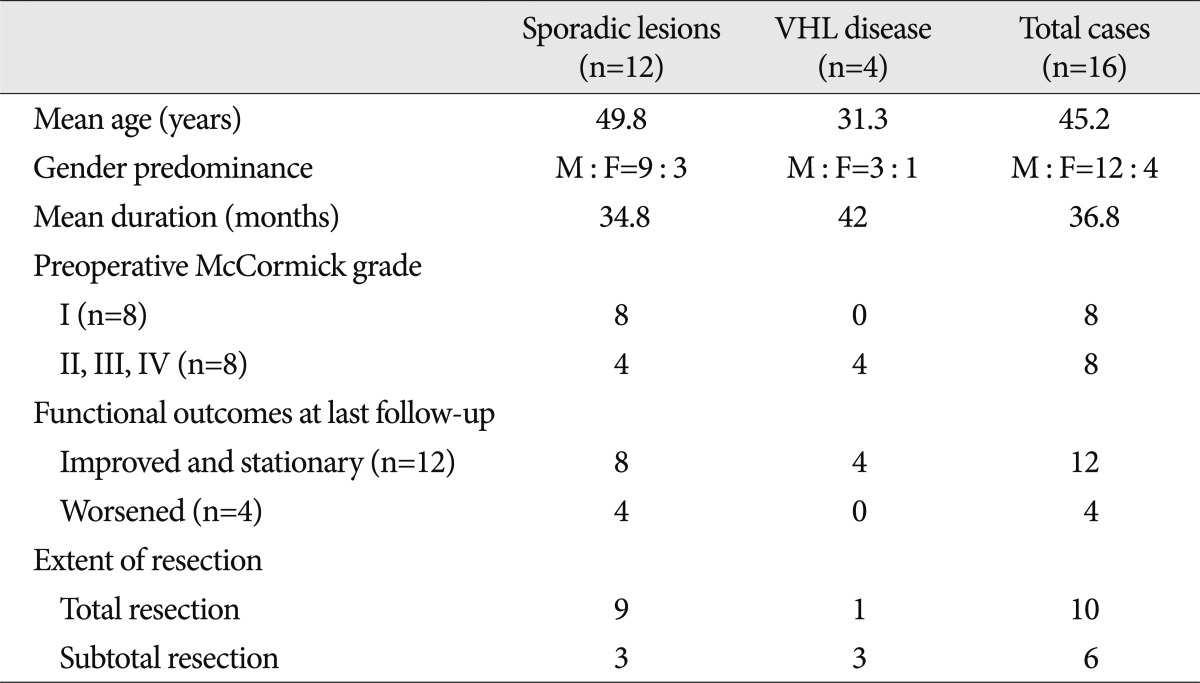
This study included sixteen patients at our institute who underwent microsurgical resection for sporadic spinal intramedullary hemangioblastomas and spinal intramedullary hemangioblastomas associated with von Hippel-Lindau (VHL) disease, between June 2003 and March 2012.
Results
A total of 30 operations were performed. Total resection (TR) of the tumor was achieved in 10 patients, and subtotal resection (STR) was achieved in 6. Postoperatively, the initial presenting symptoms were improved in 18.7% of the patients and were unchanged in 56.3%, but 25% were worse. Stable postoperative neurological functions were found in 83% of patients with preoperative McCormick grade I, and TR was achieved in 75% of these patients. In the STR group, poorer neurological status was observed in one patient, despite multiple operations. There were no poorer outcomes in the four cases of VHL disease. Various factors were analyzed, but only a correlation between the pre- and postoperative neurological status was verified in the TR-group patients.
Hemangioblastomas are highly vascular tumors of the central nervous system5,6,11,14,19) and may develop in the cerebellum, spinal cord, spinal nerves, brain stem, thalamus and pituitary stalk3,4,17,19).
Spinal cord hemangioblastomas are relatively rare, accounting for only 2% to 6% of all spinal cord tumors13). They are primarily intradural tumors, most frequently localized at the level of the cervical and thoracic vertebrae8,11). On the axial plane, the epicenters of hemangioblastomas are most commonly found in the posterior aspect of the spinal cord, in the region of the dorsal root entry zone8,9,11).
Spinal cord hemangioblastomas may occur sporadically or in association with von Hippel-Lindau (VHL) disease2,4,8,19). Whereas sporadic spinal hemangioblastomas are almost always solitary lesions, VHL disease is an autosomal dominant hereditary disease that causes lesions in the central nervous system, including the cerebellum, brain stem and retina, as well as tumors in other organs, such as the kidneys, pancreas, adrenal glands, paraganglia and epididymis4,6,13,17). The association between spinal cord hemangioblastomas and VHL disease is strong11) : approximately 20% to 45% of patients with spinal hemangioblastomas have VHL disease6,11).
Although spinal cord hemangioblastomas have benign features, such as those associated with a World Health Organization (WHO) grade I classification, and classically following a slow-growing course18), they may cause severe neurological consequences through a mass effect by intramedullary lesions11,14,17). However, a predictor of functional outcomes and the optimal treatment strategy for spinal cord hemangioblastomas are not yet fully clarified in the literature. Sporadic tumors are usually pasymptomatic at diagnosis, and these should be surgically removed11). However, the decision about whether to operate or only observe is less clear in patients who have VHL disease with multiple spinal cord lesions8,15,17).
In this study, we reviewed our experiences with 16 patients and retrospectively analyzed the clinical and radiological findings, neurological status, surgical treatments, and postoperative outcomes. The aim of this study was to determine whether there was a correlation between preoperative neurological status and postoperative functional outcomes, and to evaluate the efficacy of the treatment strategy. To predict postoperative functional outcomes, we investigated variable factors, including clinical features, tumor findings, the extent of surgical removal, and the recurrence or progression of the disease.
Between June 2003 and March 2012, 16 patients underwent microsurgical treatment for spinal cord hemangioblastomas at our institute, and their medical records and radiologic studies were analyzed retrospectively. Nine patients were new cases and seven patients had a recurrence or progression of residual lesions.
All patients had magnetic resonance imaging (MRI) taken pre- and postoperatively (Fig. 1A, B, D, 2). A routine evaluation for VHL was performed on all patients, including a family history, abdominal and cranial imaging studies and an ophthalmological examination. A preoperative angiography (Fig. 1C) was performed in 10 cases, and preoperative embolization was performed in three.
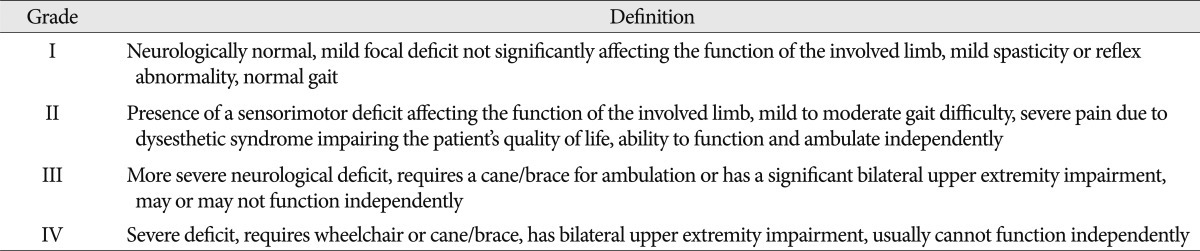
All patients underwent surgical removal using the posterior approach, and were classified into total resection (TR) and subtotal resection (STR) groups. TR is defined as complete removal of the tumor by intraoperative microsurgical findings and postoperative MRI. The neurological status and functional outcomes of the patients were evaluated preoperatively, at discharge and at the last follow-up, according to the functional scale described by McCormick et al.12) (Table 1). SPSS 19.0 (SPSS, Chicago, IL, USA) was used for statistical analysis. The non-parametric test was calculated by Mann-Whitney's U test or Spearman's method. A p value of <0.05 was considered to be statistically significant.
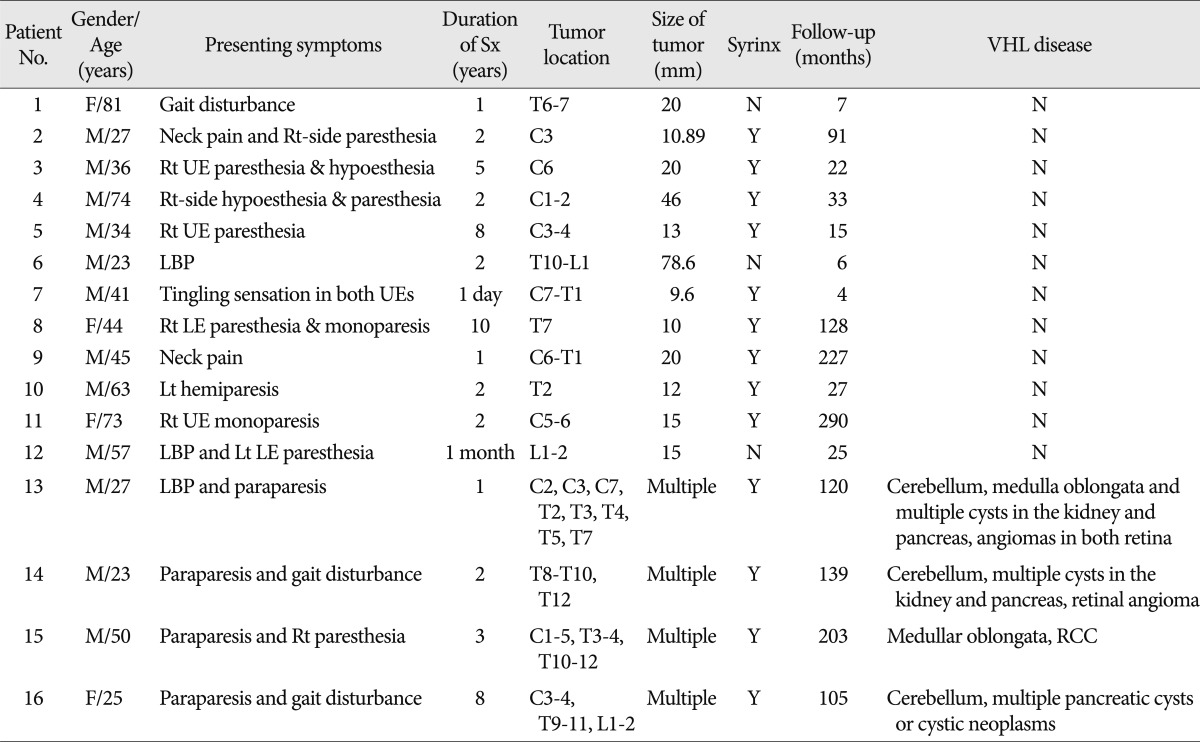
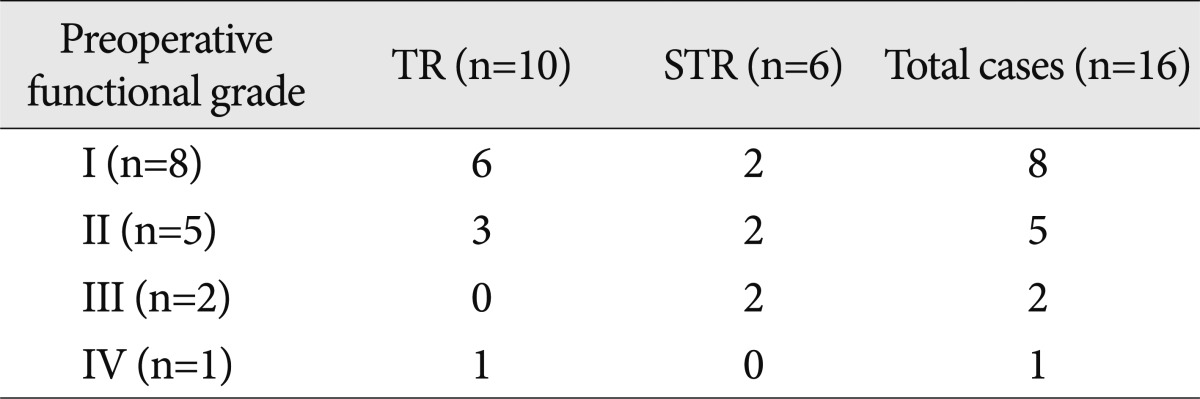
The clinical features and radiological findings are summarized in Table 2. Of the 16 patients, ranging in age from 23 to 81 years (mean age, 45.2 years), 12 were male and four were female. Four patients fulfilled the criteria for VHL disease. The mean follow-up duration was 90 months (range, 4 to 290 months). The most common presenting symptoms on admission were motor weakness (n=8) and pain or paresthesia of the limbs (n=8). Preoperatively, eight patients (50%) showed mild focal sensory changes and were classified as McCormick grade I. Five patients (31.3%) were classified as grade II, two (12.5%) as grade III, and one as grade IV. Because the mean duration between the initial symptom and admission was 36.8 months (range, 1 day to 120 months), clinical progression was relatively slow.
The spinal cord hemangioblastomas showed a strong homogeneous enhancement on the T1-weighted MRI images (WI) with gadolinium administration and hyper-intensity with surrounding edema, cysts or syrinxes on T2-WI. The tumors were located in the cervical spine in 5 patients, the thoracic spine in 3 patients, the cervico-thoracic junction in 2 patients, and the thoraco-lumbar junction in 2 patients, with multiple lesions in 4 cases. The mean tumor size was 22.5 mm (range, 9.6 mm to 78.6 mm), excluding the four VHL cases with multiple spinal lesions. Cystic components, including syrinxes and cysts, were observed in 13 cases (81.3%), and peritumoral edema was observed in all patients.
All hemangioblastomas were located on the dorsal or dorso-lateral surface of the spinal cord and were removed using the posterior approach. A total of 30 operations were performed on the 16 patients (Table 3).
Total resection of the tumor was achieved in 10 patients (62.5%), and nine were sporadic spinal hemangioblastomas. STR of the tumor was performed in 6 patients (37.5%), three of whom had VHL disease. Recurrence after total resection or progression of the residual mass after STR was observed in eight patients, who underwent a total of 22 operations (mean, 2.8 operations per person). Three patients (cases 8, 11, and 15) in the TR group (n=10) had recurrences, and 5 patients (cases 9, 10, 13, 14, and 16) in the STR group (n=6) had progression of the residual tumor and also showed progression of motor deficits. All patients who had recurrent or progressive lesions underwent a second operation. After the second surgery, the tumor recurred or progressed again in 3 patients (cases 9, 14, and 16). All four VHL patients (cases 13, 14, 15, and 16) had tumor progression and underwent serial surgeries. A syringo-subarachnoid shunt with postoperative radiation therapy was performed on one patient (case 15), but the tumor progressed with neurological deterioration. The lesion was completely removed in the second operation, but recurred again after 9 years. Another operation was performed, and neurological status improved postoperatively; however, the patient died due to an aggravated renal cell carcinoma.
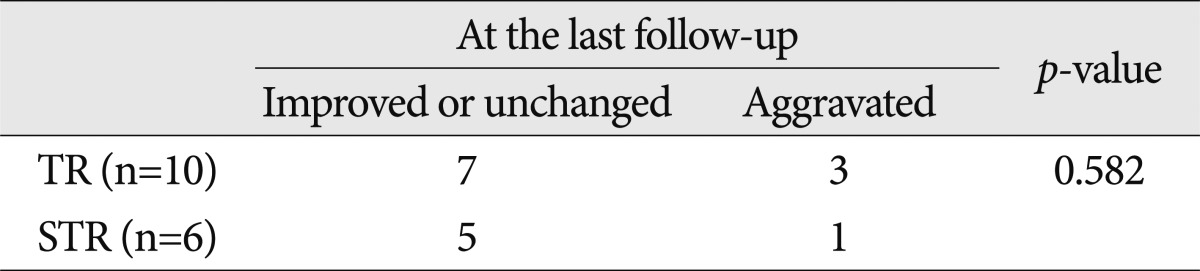
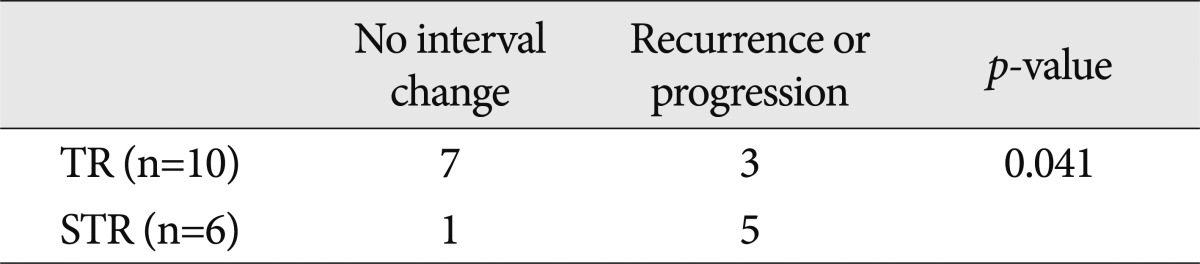
At the final follow-up, the initial presenting symptoms had markedly improved in 3 patients (18.7%, cases 8, 13, and 15). There was no change in the neurological status of 9 patients (56.3%), but 4 patients (25%, cases 1, 3, 9, and 11) were worse. The extent of resection made no statistical difference in postoperative functional outcomes (Table 4).
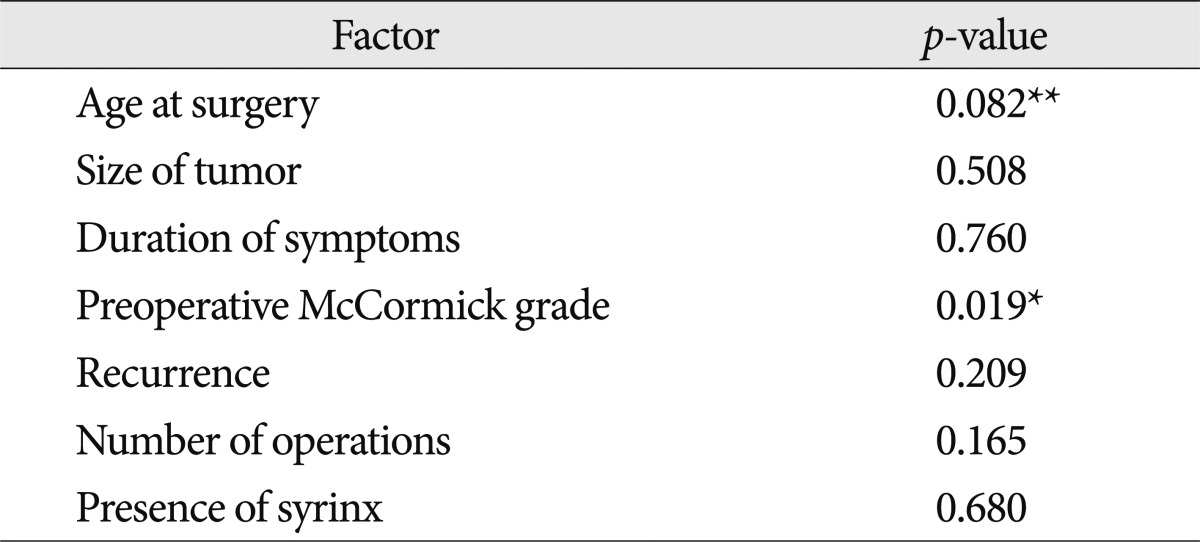
In the TR group (n=10), six patients were classified as McCormick grade I, and three were classified as grade II (Table 5). At the final follow-up, seven patients had an improved or unchanged neurological status, but the remaining three patients (cases 1, 3, and 11) exhibited greater motor deficits (Table 4). Two of these three patients were preoperative McCormick grade II (Table 3). The statistical analysis revealed a notable tendency for the postoperative functional grade in the TR-group patients to be correlated with the preoperative neurological status (rho 0.718, p<0.019). A statistical trend was observed between the patients' age in the TR group and the postoperative functional outcomes; however, the size of the tumor, the duration of symptoms, the incidence of recurrence, the number of operations, and presence of syrinx did not affect the postoperative functional outcomes (Table 6).
Despite the multiple operations in the STR group (n=6), a poorer neurological status was only observed in one patient with a sporadic lesion (case 9), and the other patients had either improved or had an unchanged functional status at the last follow-up (Table 4). Before the surgery, three patients with VHL disease had a mild to moderate degree of motor weakness, and of the three sporadic hemangioblastoma cases, two were McCormick grade I, and one was grade II (Table 3). The extent of resection (TR or STR) was correlated with recurrent lesions or tumor progression (Table 7), but the presence of recurrence, the progression of the lesion and the number of repeated surgeries were not associated with surgical functional outcomes in the STR group.
In the cases with recurrence or progressive disease (n=8), three patients remained stable and three cases recovered to a better status during the follow-up period. In addition, there was neither postoperative aggravation nor a poorer functional outcome in the patients with VHL disease who experienced recurrence (Table 8).
Some of our cases exhibited immediate postoperative functional
outcomes that were different from the final follow-up results. In nine patients, the functional outcomes at the final follow-up were unchanged compared with the preoperative neurological status. However, the motor function of 4 patients (cases 2, 6, 7, and 14) worsened in the immediate postoperative period, but gradually improved to that of the preoperative period through active rehabilitation.
Three patients over 70 years of age underwent TR. Two of the patients (cases 1 and 11) were grade II preoperatively, and one was grade I. The motor dysfunctions in two patients worsened to McCormick grade III or IV in the immediate postoperative period, and these patients could not walk independently. Thus, active rehabilitation was not successful in older patients, and their functional outcomes were not improved at the final follow-up.
This study showed the differences between sporadic hemangioblastomas and VHL disease-related hemangioblastomas, which are summarized in Table 8. The mean age of symptom onset in patients with VHL disease was 31.3 years, in the fourth decade of life, and the mean duration between the initial symptom and admission was 42 months. There were no patients who were preoperative McCormick grade I, and the four VHL patients suffered from mild to moderate paresis. The preoperative motor dysfunctions of the patients gradually worsened, and VHL disease was diagnosed after the initial evaluation. Cerebellar lesions (n=3) and multiple cysts in the kidney (n=3) and pancreas (n=3) were commonly found in this study.
Total resection was achieved in only one case, with the remaining three patients undergoing a subtotal resection. After the operations, the progression of the residual tumors and neurological deterioration were noted. There were relapses of the tumors in all four VHL patients, and all of these patients underwent subsequent operations, with an average of 3.25 operations each.
Notably, there was neither postoperative aggravation nor a poorer functional outcome in the VHL patients with recurrence, despite the repeated surgeries. Paraparesis or gait disturbance was improved postoperatively in 2 VHL patients, and the other two patients experienced unchanged functional outcomes.
Due to the small number of VHL disease cases, it was not statistically validated that a patient's age, preoperative neurological status, tumor location and size, presence of a syrinx or progressive lesions or the number of resected tumors were correlated with postoperative functional outcomes.
Generally, spinal cord hemangioblastomas are encapsulated, non-infiltrative tumors7,10,18), and total removal is therefore feasible in most cases. However, the capsule of the tumor is fragile, and violation of the capsule can induce massive intraoperative bleeding10,18). Poor delineation of the feeding arteries and draining veins may also lead to profuse intraoperative bleeding5). Thus, a thorough understanding of the angio-architecture and a meticulous microsurgical technique are required to achieve total resection. In our experience of failed total resections, massive intraoperative bleeding obscured the surgical field and increased the risk of indiscriminate coagulation of the undefined vessel for hemostasis. Consequently, disruption of the draining veins before identifying the tumor feeders led to more copious bleeding. Aggressive dissection and coagulation in the blurred margin of the tumor induced neural tissue damage or neurological deteriorations postoperatively. Hence, a small lesion remained adjacent to the vessels after the cautious control of bleeding.
From this perspective, preoperative angiography is mandatory for the identification of the tumors' feeders and the drainers1,5). We performed 10 cases of preoperative angiography, which was helpful for identifying the feeders and drainers in the surgical field. Furthermore, to reduce the risk of bleeding, the feeding artery should be dissected carefully before coagulation of the draining vein is performed.
When possible, preoperative tumor embolization is also useful for reducing intraoperative bleeding5). In our experiences with three patients, embolized tumors were more easily dissected, and intraoperative bleeding was much less than expected.
According to the literature, preoperatively paretic patients have a tendency toward postoperative neurological deterioration compared with asymptomatic patients2,16,18,19). These studies demonstrated that the functional outcomes at the final follow-up strongly correlated with the preoperative neurological status18,19). In addition, several authors reported favorable outcomes after total tumor resection1,5,14). Our experience of total resection of solitary hemangioblastomas revealed a similar tendency for the postoperative functional outcome to correlate with the preoperative neurological status.
In the TR group, 83% of the patients who had preoperative focal neurological deficits of McCormick grade I showed stable neurological functions after removal of the tumor. Of those patients with aggravated postoperative functional outcomes, 66% had a preoperative motor weakness of McCormick grade II. Interestingly, total resection was more common in those patients who only had a focal neurological deficit of McCormick grade I, and 75% of the patients who were preoperative McCormick grade I underwent total resection of the tumors. Accordingly, we assume that preoperative functional status is a predictor of the postoperative neurological outcome, and total resection may be feasible in patients who have focal neurological deficits or who are in the early stage of the natural disease course. Therefore, surgery may provide favorable neurological outcomes in patients with initial mild neurological deficits who are candidates for total resection. Many factors, including tumor characteristics, duration of symptoms, the presence of recurrence, and the number of surgeries were considered to be predictors of postoperative outcomes, but no further interrelationship with the functional outcomes was shown in our experiences of sporadic hemangioblastomas.
However, the small sample size with a consequent lack of statistical significance was a limitation of our study. In addition, whether or not a motor deficit suggests the progressive status of an intramedullary hemangioblastoma is still unclear. This assumption is also only applicable to patients who undergo TR and have sporadic hemangioblastomas and not to those who have VHL disease.
The predictors of the surgical outcome were uncertain in the STR group. This study demonstrated that there was no statistical difference in postoperative function by subtotal resection, the presence of recurrence or progression and repeated surgeries. Recurrence or tumor progression was more common in the STR group than in the TR group, but the functional outcomes of the STR group at the last follow-up were not inferior to those of the TR group. Despite repeated surgeries, the rate of neurological deterioration was actually lower in the STR group.
We assume that an aggressive surgical resection to achieve TR may inversely cause postoperative neurological deterioration, and the reason for favorable results in the STR group may be the residual lesions, which were left behind with the intention of avoiding neural tissue damage.
Therefore, we can postulate that preoperative mild neurological deficit and fastidious microsurgical manipulation of the neural tissue are associated with favorable outcomes for solitary hemangioblastomas. Moreover, our study showed that age over 70 years deserved much consideration as a predisposing factor for a poor functional outcome.
To clarify the predictors of postoperative outcomes, further studies should be performed on a larger scale.
Despite the similarity in the clinical, biological, and histological features between sporadic hemangioblastomas and those associated with VHL disease, definite differences with respect to the average age at presentation, the number of tumors and the treatment strategy are demonstrated in this study, in conjunction with the literature6,11). The mean age of symptom onset was younger, and the duration of symptoms was longer in VHL disease-related hemangioblastoma patients when compared with patients having sporadic ones.
Our experience demonstrated that all spinal cord hemangioblastomas associated with VHL disease were recurrent or progressive. The initial presenting symptoms were shown as a more severe degree of weakness, but there was no poorer postoperative functional outcome at the final follow-up. Previously, Kanno et al.4) reported similar results, with functional outcomes in most surgical cases of symptomatic VHL disease remaining unchanged or showing improvements after the operation.
In our experience, VHL disease showed a trend in which the preoperative neurological status was not correlated with the surgical outcome, unlike sporadic spinal hemangioblastoma in the TR group. Although several retrospective studies of VHL disease have indicated that preoperative neurological function, the presence of a ventral or ventro-lateral lesion, tumor size, age of onset, the presence of a syrinx, and the number of resected tumors are predictors of outcome4,9,13,19), these factors were not verified in this study.
As the goal of surgery in spinal hemangioblastomas associated with VHL disease is symptomatic palliation, aggressive surgical resection of the lesions should be avoided. Because there is currently no curative treatment for VHL disease, the preservation of motor function is more important than the extent of resection.
We advocate the total resection of solitary spinal cord hemangioblastomas because surgery is the only effective treatment modality for this condition, especially in sporadic cases. This study indicates that postoperative functional outcomes reflect preoperative neurological deficits in totally resected hemangioblastomas. However, there is no correlation between postoperative functional outcomes and other variable factors, including tumor size or location, the extent of resection, the recurrence or progression of the lesion and the number of repeated surgeries.
Therefore, we conclude that preoperative focal neurological deficits and meticulous microsurgical manipulation of neural structures may be the predictors of favorable outcomes of solitary spinal cord hemangioblastomas. In addition, a non-aggressive surgical approach is the optimal strategy to preserve the neurological function in spinal cord hemangioblastomas associated with VHL disease.
References
1. Boström A, Hans FJ, Reinacher PC, Krings T, Bürgel U, Gilsbach JM, et al. Intramedullary hemangioblastomas : timing of surgery, microsurgical technique and follow-up in 23 patients. Eur Spine J. 2008; 17:882–886. PMID: 18389290.

2. Cristante L, Herrmann HD. Surgical management of intramedullary hemangioblastoma of the spinal cord. Acta Neurochir (Wien). 1999; 141:333–339. discussion 339-340. PMID: 10352742.

3. Gläsker S, Berlis A, Pagenstecher A, Vougioukas VI, Van Velthoven V. Characterization of hemangioblastomas of spinal nerves. Neurosurgery. 2005; 56:503–509. discussion 503-509. PMID: 15730575.

4. Kanno H, Yamamoto I, Nishikawa R, Matsutani M, Wakabayashi T, Yoshida J, et al. Spinal cord hemangioblastomas in von Hippel-Lindau disease. Spinal Cord. 2009; 47:447–452. PMID: 19030009.

5. Lee DK, Choe WJ, Chung CK, Kim HJ. Spinal cord hemangioblastoma : surgical strategy and clinical outcome. J Neurooncol. 2003; 61:27–34. PMID: 12587793.
6. Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, et al. von Hippel-Lindau disease. Lancet. 2003; 361:2059–2067. PMID: 12814730.

7. Lonser RR, Oldfield EH. Microsurgical resection of spinal cord hemangioblastomas. Neurosurgery. 2005; 57:372–376. discussion 372-376. PMID: 16234688.

8. Lonser RR, Oldfield EH. Spinal cord hemangioblastomas. Neurosurg Clin N Am. 2006; 17:37–44. PMID: 16448906.

9. Lonser RR, Weil RJ, Wanebo JE, DeVroom HL, Oldfield EH. Surgical management of spinal cord hemangioblastomas in patients with von Hippel-Lindau disease. J Neurosurg. 2003; 98:106–116. PMID: 12546358.

10. Malis LI. Atraumatic bloodless removal of intramedullary hemangioblastomas of the spinal cord. J Neurosurg. 2002; 97:1–6. PMID: 12120629.

11. Mandigo CE, Ogden AT, Angevine PD, McCormick PC. Operative management of spinal hemangioblastoma. Neurosurgery. 2009; 65:1166–1177. PMID: 19934977.

12. McCormick PC, Torres R, Post KD, Stein BM. Intramedullary ependymoma of the spinal cord. J Neurosurg. 1990; 72:523–532. PMID: 2319309.

13. Mehta GU, Asthagiri AR, Bakhtian KD, Auh S, Oldfield EH, Lonser RR. Functional outcome after resection of spinal cord hemangioblastomas associated with von Hippel-Lindau disease. J Neurosurg Spine. 2010; 12:233–242. PMID: 20192620.

14. Na JH, Kim HS, Eoh W, Kim JH, Kim JS, Kim ES. Spinal cord hemangioblastoma : diagnosis and clinical outcome after surgical treatment. J Korean Neurosurg Soc. 2007; 42:436–440. PMID: 19096585.

15. Oppenlander ME, Spetzler RF. Advances in spinal hemangioblastoma surgery. World Neurosurg. 2010; 74:116–117. PMID: 21299999.

16. Pietilä TA, Stendel R, Schilling A, Krznaric I, Brock M. Surgical treatment of spinal hemangioblastomas. Acta Neurochir (Wien). 2000; 142:879–886. PMID: 11086826.

17. Richard S, Campello C, Taillandier L, Parker F, Resche F. French VHL Study Group. Haemangioblastoma of the central nervous system in von Hippel-Lindau disease. J Intern Med. 1998; 243:547–553. PMID: 9681857.

18. Shin DA, Kim SH, Kim KN, Shin HC, Yoon DH. Surgical management of spinal cord haemangioblastoma. Acta Neurochir (Wien). 2008; 150:215–220. discussion 220. PMID: 18253694.

19. Takai K, Taniguchi M, Takahashi H, Usui M, Saito N. Comparative analysis of spinal hemangioblastomas in sporadic disease and Von Hippel-Lindau syndrome. Neurol Med Chir (Tokyo). 2010; 50:560–567. PMID: 20671381.

Fig. 1
Case 5. Preoperative MRI : T2-weighted sagittal image (A) showing a hyperintense lesion with spinal cord swelling from C2 to T1. Gadolinium-enhanced T1 sagittal image (B) revealing a heterogeneous well enhancing mass at the C3-4 spinal cord level. Preoperative angiography (C) showing a hypervascular intramedullary mass at the C3 level fed by the posterior spinal and Lt ascending cervical artery. Postoperative MRI : enhanced T1 sagittal image (D) showing no residual enhanced mass and nearly disappeared cervical cord swelling.
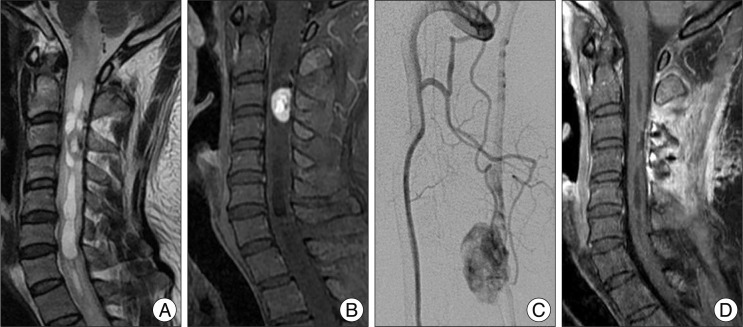
Fig. 2
Case 16. Gadolinium-enhanced T1 sagittal image (A) showing multiple variably sized, well-enhanced subpial nodules at the first operation site. Sequentially enhanced T1 sagittal image (B) revealing the recurrent lesion at the level of T11. Postoperative enhanced T1 sagittal image (C) showing the presence of small residual nodules. Contrast-enhanced brain sagittal image (D) showing asymptomatic cervical lesions. Image of the tumor increasing in size and becoming symptomatic (E). Postoperative enhanced T1-weighted image (F) showing no residual tumor at the operation site.
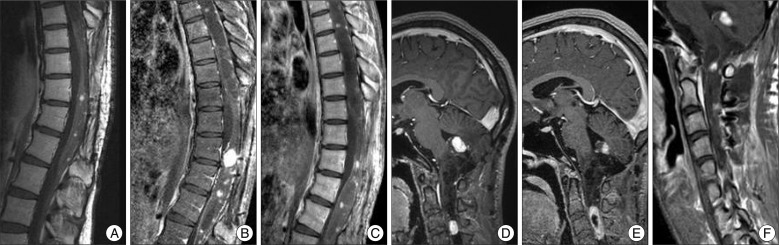
Table 3
Surgical results of the spinal cord hemangioblastomas
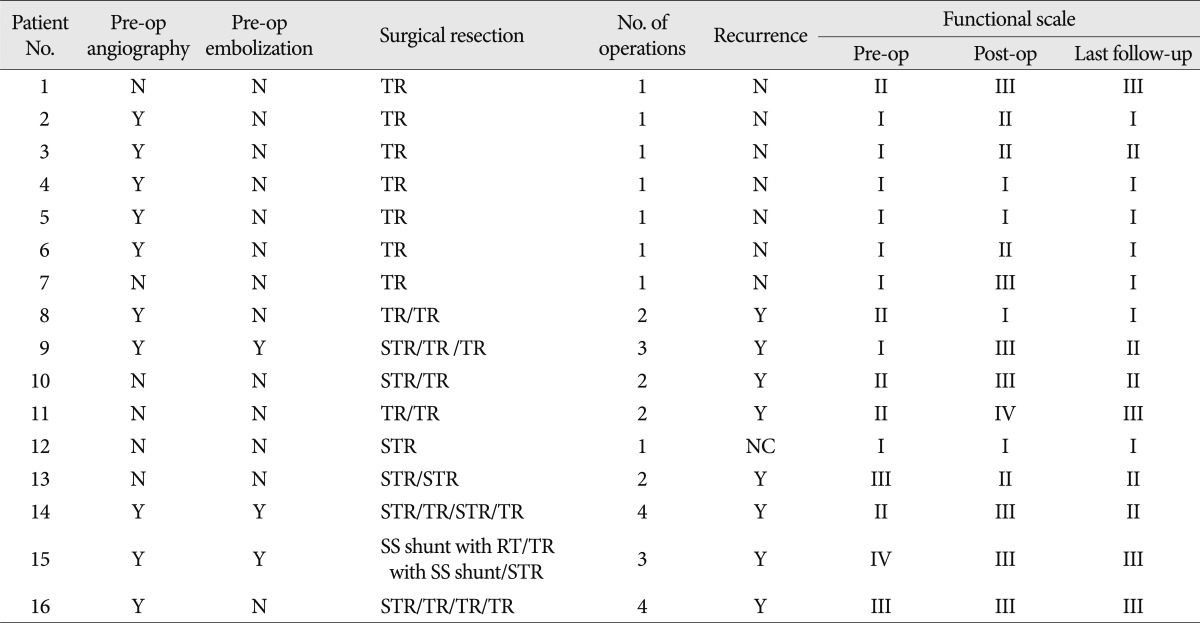
Functional scale according to the McCormick classification (Table 1). No : number, Y : present, N : absent, NC : no interval change, TR : total resection, STR : subtotal resection, SS shunt : syringo-subarachnoid shunt, RT : radiation therapy




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download