Abstract
Objective
To evaluate a new posterior atlantoaxial fixation technique using a nitinol shape memory loop as a simple method that avoids the risk of vertebral artery or nerve injury.
Methods
We retrospectively evaluated 14 patients with atlantoaxial instability who had undergone posterior C1-2 fusion using a nitinol shape memory loop. The success of fusion was determined clinically and radiologically. We reviewed patients' neurologic outcomes, neck disability index (NDI), solid bone fusion on cervical spine films, changes in posterior atlantodental interval (PADI), and surgical complications.
Results
Solid bone fusion was documented radiologically in all cases, and PADI increased after surgery (p<0.05). All patients remained neurologically intact and showed improvement in NDI score (p<0.05). There were no surgical complications such as neural tissue or vertebral artery injury or instrument failure in the follow-up period.
Conclusion
Posterior C1-2 fixation with a nitinol shape memory loop is a simple, less technically demanding method compared to the conventional technique and may avoid the instrument-related complications of posterior C1-2 screw and rod fixation. We introduce this technique as one of the treatment options for atlantoaxial instability.
The atlantoaxial complex is unique among the intervertebral joints. It is the most mobile segment of the spine with respect to axial rotation, allowing a 90 degree bilateral range of motion3). The complex largely depends on the ligamentous supports and the integrity of the odontoid for its stability.
Symptomatic atlantoaxial instability requires stabilization of the atlantoaxial joint for treatment. The causes of atlantoaxial instability include trauma, congenital malformations, inflammatory arthritis, malignancy, and infections3,17).
Various techniques of atlantoaxial fixation have evolved, each trying to achieve higher fusion rate, important given the extreme mobility of this joint. Since Gallie introduced a posterior wiring and autologous graft in 1939, various authors have reported modifications of the Gallie procedure, with success rates ranging from 75-97%, although this success depended on the use of an external halo orthosis8,9). In an effort to improve the fusion rate, Magerl and Seemann described C1-2 transarticular screw fixation in 1979, which increased the fusion rate to more than 95%4,10,11,13,16,19). Screw fixation remains the gold standard for posterior C1-2 fusion; however, it has some limitations such as technical difficulty and the risk of nerve root or vertebral artery injury20).
In this report, we introduce a new C1-2 fixation method using a nitinol shape memory loop. Nitinol is an alloy of nickel and titanium that belongs to a class of shape memory alloys. It is flexible below 10℃ (50℉), but returns to its original shape and regains its rigidity above 30℃ (86℉).
We used a nitinol loop as a C1-2 posterior column supporter. The shape memory loop has been used previously in the thoracic and lumbar regions6,12,15). Recently, it also has been used in posterior cervical fixation in the subaxial cervical spine22). The aim of this study was to evaluate a posterior fixation technique for C1-2 instability using a nitinol shape memory loop as a new method that avoids the risk of vertebral artery or nerve injury.
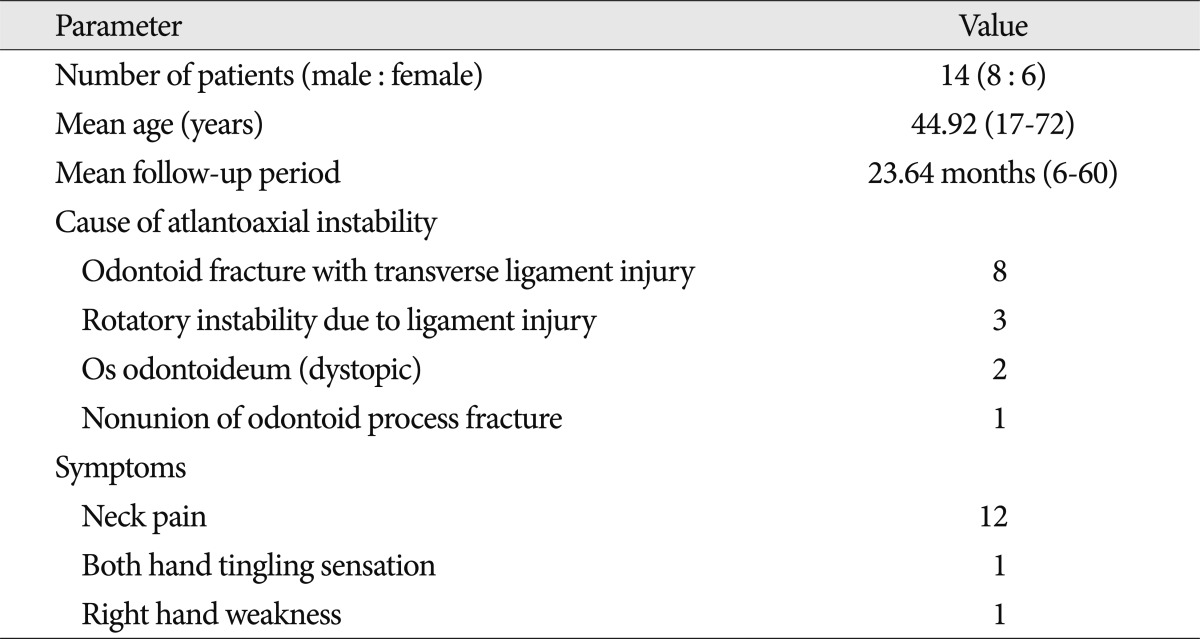
From January 2006 to January 2011, 14 patients with atlantoaxial instability were treated with this new nitinol shape memory loop fixation technique at our neurosurgery department. We used two kinds of nitinol memory loop (SpinoFix™, Fixation system; Biosmart CO., Korea and Davydov™ and KIMPF-DI Fixing system; CJSC KIMPF CO., Seoul, Korea) There were eight men and six women, and the mean age was 44.92 years (Table 1). Mean follow-up period was 23.64 months. There were eight patients with odontoid process fractures with transverse ligament injury, three with C1-2 rotational instability due to transverse and alar ligament injury, two with symptomatic os odontoideum (orthotopic type), and one with nonunion of odontoid process fracture. C1-2 rotational instability was defined as atlantoaxial subluxation or fixation that presented on C-spine CT scan. Ligament injuries on MRI scan were confirmed by neurosurgeon and neuroradiologist.
The procedure requires the patient to be placed in a prone position after induction of general anesthesia. The head is secured in a Mayfield holder and maintained in a neutral position. When severe instability or spinal cord compression is present, a cervical collar is used when turning the patient in order to reduce the risk of spinal cord injury (SCI). The posterior suboccipital and cervical regions are draped in the usual fashion as for a C1-2 fusion procedure. Lateral fluoroscopy is performed at intervals during the surgery.
A midline linear incision is made starting from the inion, and the muscles and fascia are dissected to expose the occiput and the posterior C1 and C2 vertebrae. Then, the superior margin of the C1 posterior ring and the inferior margin of the C2 lamina are dissected carefully to create a space between the thecal sac and bone and prevent spinal cord compression by the surgical hook. After that, the mesh cage packed with autologous or allograft bone is shaped to fit between C1 posterior ring and C2 lamina. After decorticating the inferior aspect of the C1 posterior ring and the superior aspect of the C2 lamina, the interpositional graft is situated between C1 and C2. Template-measuring instruments are used to calculate the exact size of the loop. We select a length of memory loop smaller than the measured distance between the C1 ring and the C2 lamina to tighten the grafted material and posterior C1-2 ring when the loop reverted to its original shape. Then, the memory loop is cooled in sterilized cold saline to a temperature less than 10℃ (50℉) for at least 30 seconds. The loop became flexible and could be deformed easily to fit between the C1 and C2 rings. One hook is placed behind the C1 posterior ring, and the other is placed behind the C2 lamina. Then, another loop is placed on the opposite side over the midline. After bilateral installation of the two loops, they are irrigated with warm saline between 35℃ (95℉) and 45℃ (113℉), and the loop slowly regain its initial form and rigidity, tightly fixing the C1 posterior ring, the mesh cage, and the C2 lamina (Fig. 1A). We assess the fixation by manually pulling and shaking the loops.
After confirmation of the fixation with intraoperative plain lateral radiography, the wound is closed layer by layer (Fig. 1B). Postoperatively, all patients are treated with immobilization for 8-12 weeks in a cervical collar.
We retrospectively reviewed the medical records of the 14 enrolled patients. Success of fusion was defined as improvement of neck pain and radiologic findings of bone fusion. Clinical improvement of neck pain was assessed with the neck disability index (NDI) preoperatively and 6 months postoperatively. The total NDI score ranged from 0 to 50, and percent disability was calculated as total score/50×100 (%). Percent disability of 0-20% was defined as minimal disability, 21-40% as moderate, 41-60% as severe, 61-80% as crippled, and 81-100% as bed bound.
We also reviewed surgical complications, instrumentation failure, bony fusion rate, and posterior atlantodental interval (PADI) in all patients. PADI was obtained preoperatively and six months postoperatively and was calculated as the distance on a plain lateral radiograph from the back of the odontoid to the anterior aspect of the posterior C1 ring. Solid bone fusion and instability were assessed with flexion-extension radiographs at intervals and 3D cervical spine computed tomography (CT) six months postoperatively. Bone fusion was defined as evidence of continuity of trabecular bone between C1 and C2 across the graft.
Statistical analysis was performed using the t-test. A significance level of p<0.05 was used.
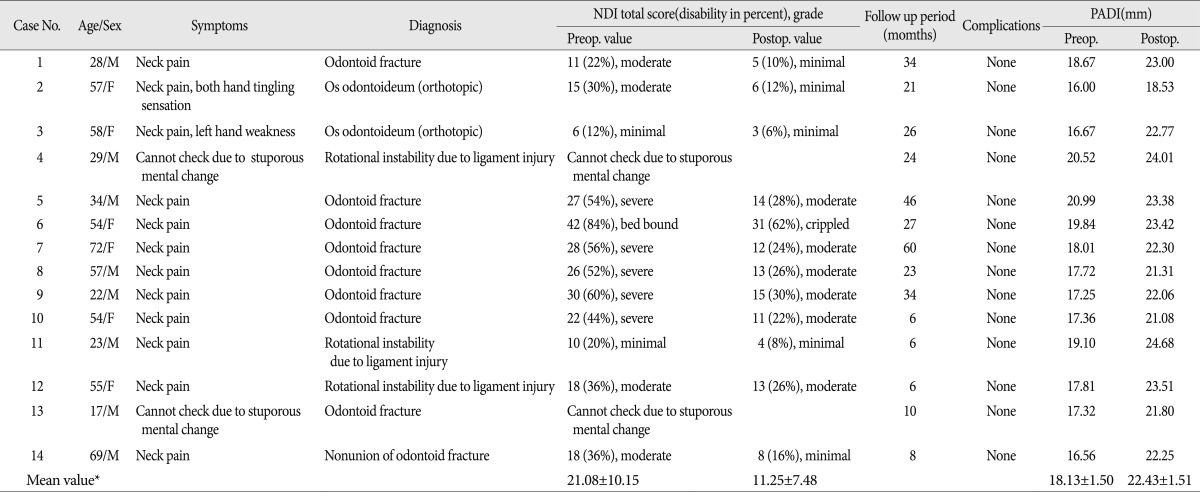
A total of 14 subjects were reviewed (Table 2). Before surgery, five patients were in the severe disability category according to NDI score, four in the moderate disability category, two in the minimal disability category, and one in the bed bound disability category. Two patients were not evaluated due to stuporous mental status.
Posterior C1-2 fusion using the nitinol loop system was performed in all of the enrolled patients. After surgery, all patients had a significantly improved NDI score compared with the preoperative value (p<0.05) (Table 2). Nine patients moved into a lower disability stage, three remained the same, and none of the patients had worsening of disability. Halo orthosis was used postoperatively in one patient to provide additional stability due to combined compression fractures at T9, T10, and T11 vertebrae. As the patient was not tolerable to wear cervical collar and TLSO simultaneously, we used Halo orthosis of which length was customized longer than that of usual one enough to stabilize lower thoracic spine.
The fixation technique in this fusion procedure was successfully applied in all cases. We used autologous iliac crest bone grafts for bone fusion in seven patients in succession until 2008 and, then allograft bone in the others. There were no surgical complications, vertebral artery or neural tissue injury, or cases of instrumentation failure.
Solid stabilization was maintained throughout the follow-up period. To confirm the solid stabilization, Brantigan-Steffee classification was used5). Also, there was evidence of solid bone fusion on 3D cervical spine CT at six months postoperatively, and there was no instability on flexion-extension radiographs during the follow-up period in any of the cases.
The mean PADI significantly increased to 22.43±1.51 mm six months after surgery compared with a preoperative value of 18.13±1.50 mm (p<0.05) (Table 2).
A 57-year-old female patient presented with posterior neck pain and tingling sensation of both hands after slip down. Initial plain radiographs and cervical CT showed orthotopic type of os odontoideum (Fig. 2A). Magnetic resonance imaging showed severe cervical canal stenosis with cord contusion (Fig. 2B). Surgical intervention was recommended.
We performed posterior C1-2 fixation with a nitinol shape memory loop, and the patient recovered without further neurological deficits. Neck pain and tingling sensation of both hands resolved with improvement of NDI score. Six months after the operation, simple cervical spine radiographs showed no instrument failure and improvements in cervical lordotic curve and PADI from 16.00 mm to 18.53 mm (Fig. 2D, E). On 3D cervical spine CT, successful fusion was demonstrated as solid bridging bone formation between C1 and C2 across the graft (Fig. 2C).
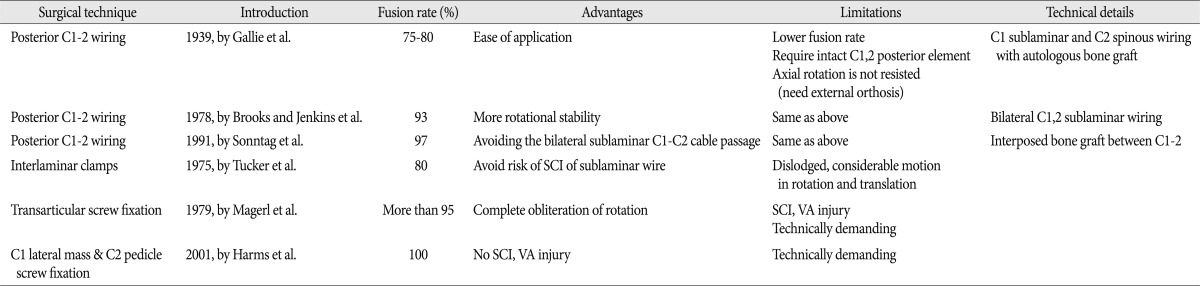
The purpose of treatment in atlantoaxial instability is to achieve a solid fusion between C1 and C2, virtually eliminating any motion between them. This is expected to relieve neck pain and avoid the risk of further neurological deficits. Various techniques are available for fixation of the atlantoaxial joint (Table 3).
Posterior C1-2 wiring techniques were introduced in 1939 by Gallie2). He reported a technique for C1 sublaminar and C2 spinous process wiring using iliac crest bone graft. To enhance rotational stability, Brooks and Jenkins modified the technique by bilaterally placing C1-2 sublaminar wires. Sonntag introduced further modification of the Gallie technique by placing a wire under the C1 lamina, around an interposed graft and the C2 spinous process7).
These posterior wiring techniques were the most common means of stabilization in the past. The rates of successful fusion range from 75 to 97% when the posterior wiring techniques are used. However, this technique requires additional external halo orthosis for successful fusion and does not completely avoid the risk of SCI or dural injury8,9). In the 1980s, interlaminar clamps were popularized as an alternative method of posterior C1-C2 fixation. However, these clamps may become dislodged and allow considerable rotation and translation18).
In an effort to enhance the fusion rate at C1-2, Magerl and Seemann13) developed a fixation procedure involving the transarticular screw technique. This technique has lead to considerable improvement in the fusion rates up to more than 95% due to minimized rotary movements and has become the gold standard for atlantoaxial fusion as it does not require intact posterior elements or the passage of sublaminar wires4,10,11,13,16,19). Although the fusion rate is high, the technique remains technically demanding, and precise knowledge of VA anatomy is necessary to avoid vascular injury. In a recent survey, the risk of VA injury was 2.2% per screw, the risk of neurological deficit was 0.1% per screw, and the mortality rate was 0.1%20). Radiographic and anatomical studies of the atlantoaxial complex suggest that up to 20% of the patients have atlantoaxial anatomy that precludes safe bilateral transarticular screw fixation1,14,21).
We assumed that the ideal posterior atlantoaxial fusion technique would achieve a higher bony fusion rate without the addition of an external halo orthosis and would be an easy surgical technique with a low risk of spinal cord or vertebral artery injury.
Nitinol is a shape memory alloy of nickel and titanium. It has shape memory character in that it is flexible and easily deformed below 10℃ (50℉) but regains its initial form, produces large forces, and becomes rigid when heated up to 30℃ (86℉). It also has high fatigue strength, moderate impact resistance, and biocompatibility12). Several spinal surgeons have focused on this characteristic and used this material in lumbar, thoracic and subaxial cervical spinal surgery. Kim et al.12) have reported the usefulness of a nitinol memory loop in surgical treatment for lumbar degenerative disorders using it as the posterior column supporter. Yu et al.22) have reported the use of shape memory loop in posterior subaxial cervical spinal fusion in an anterior-posterior combined approach.
We used a nitinol memory loop in posterior atlantoaxial fusion as a posterior column supporter. The nitinol memory loop technique has several advantages over other previous fixation techniques. This technique is similar to that utilizing interlaminar clamps in that immediate fixation is achieved, and the risk associated with sublaminar wires is avoided. However, interlaminar clamps can create an indentation on the thecal sac. We think, as the memory loop system has a smaller profile and occupies smaller space for available cord than interlaminar clamps, the risk of spinal cord compression is low.
We achieved a 100% bony fusion rate without the help of an external halo orthosis. This indicates that this new technique can produce a higher bony fusion rate and stability than posterior wiring techniques. Second, we accomplished atlantoaxial posterior fusion without vertebral artery or neural tissue injury. This technique might avoid the surgical complications seen in C1-2 screw and rod fixation techniques. Also, it is relatively easy to apply the loop without the need for wide muscle dissection for pedicle screw fixation. The technique has a shorter operation time and does not need preoperative imaging studies of vertebral artery anatomy.
However, there are several limitations to this technique. Similar to posterior wiring or interlaminar clamps, this technique can be used only in cases with intact posterior C1 and C2 elements. Thus, it cannot be used when laminectomy is required or when there is trauma-induced disruption of the posterior elements. In addition, the nitinol loop produces large forces with a shape memory effect, but the stiffness is not strong as that of cortical bone or screw and rod fixation systems12). Although we used a smaller length of the loop than that of the measured distance between the upper C1 and lower C2 rings, we maintained graft stabilization without subsidence of loop into the rings due to the aforementioned mechanical behavior of the nitinol loop.
Further investigation with more subjects and a longer follow-up period is required to determine the utility of the nitinol loop as a primary fusion construct.
For patients with atlantoaxial instability, posterior fixation with nitinol shape memory alloy is an alternative method of posterior C1-2 fusion. We believe that surgeons can reduce the operation time and technical demand of screw fixation with this technique and may avoid the risk of VA or neural tissue injury.
Acknowledgements
This paper was supported by Fund of Biomedical Research Institute, Chonbuk National University Hospital.
References
1. Abou Madawi A, Solanki G, Casey AT, Crockard HA. Variation of the groove in the axis vertebra for the vertebral artery. Implications for instrumentation. J Bone Joint Surg Br. 1997; 79:820–823. PMID: 9331044.
2. Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974; 56:1663–1674. PMID: 4434035.

3. Bahadur R, Goyal T, Dhatt SS, Tripathy SK. Transarticular screw fixation for atlantoaxial instability-modified Magerl's technique in 38 patients. J Orthop Surg Res. 2010; 5:87. PMID: 21092173.
4. Blauth M, Richter M, Lange U. [Trans-articular screw fixation of C1/C2 in atlanto-axial instability. Comparison between percutaneous and open procedures]. Orthopade. 1999; 28:651–661. PMID: 10506369.

5. Brantigan JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine (Phila Pa 1976). 1993; 18:2106–2107. PMID: 8272967.
6. Braun JT, Akyuz E, Udall H, Ogilvie JW, Brodke DS, Bachus KN. Three-dimensional analysis of 2 fusionless scoliosis treatments: a flexible ligament tether versus a rigid-shape memory alloy staple. Spine (Phila Pa 1976). 2006; 31:262–268. PMID: 16449897.

7. Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978; 60:279–284. PMID: 348703.

8. Coyne TJ, Fehlings MG, Wallace MC, Bernstein M, Tator CH. C1-C2 posterior cervical fusion: long-term evaluation of results and efficacy. Neurosurgery. 1995; 37:688–692. discussion 692-693. PMID: 8559297.
9. Dickman CA, Sonntag VK, Papadopoulos SM, Hadley MN. The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg. 1991; 74:190–198. PMID: 1988587.

10. Grob D, Jeanneret B, Aebi M, Markwalder TM. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br. 1991; 73:972–976. PMID: 1955447.

11. Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992; 5:464–475. PMID: 1490045.
12. Kim YS, Zhang HY, Moon BJ, Park KW, Ji KY, Lee WC, et al. Nitinol spring rod dynamic stabilization system and Nitinol memory loops in surgical treatment for lumbar disc disorders: short-term follow up. Neurosurg Focus. 2007; 22:E10.

13. Magerl F, Seemann PS. Kehr P, Weidner A, editors. Stable posterior fusion of the atlas and axis by transarticular screw fixation. Cervical spine I Vol 1. 1987. Vol 1. New York: Springer;p. 322–327.

14. Miyata M, Neo M, Ito H, Yoshida M, Miyaki K, Fujibayashi S, et al. Is rheumatoid arthritis a risk factor for a high-riding vertebral artery? Spine (Phila Pa 1976). 2008; 33:2007–2011. PMID: 18708934.

15. Sanders JO, Sanders AE, More R, Ashman RB. A preliminary investigation of shape memory alloys in the surgical correction of scoliosis. Spine (Phila Pa 1976). 1993; 18:1640–1646. PMID: 8235844.

16. Stillerman CB, Wilson JA. Atlanto-axial stabilization with posterior transarticular screw fixation: technical description and report of 22 cases. Neurosurgery. 1993; 32:948–954. discussion 954-955. PMID: 8327097.
17. Stokes JK, Villavicencio AT, Liu PC, Bray RS, Johnson JP. Posterior atlantoaxial stabilization: new alternative to C1-2 transarticular screws. Neurosurg Focus. 2002; 12:E6. PMID: 16212333.

18. Vender JR, Rekito AJ, Harrison SJ, McDonnell DE. The evolution of posterior cervical and occipitocervical fusion and instrumentation. Neurosurg Focus. 2004; 16:E9. PMID: 15264787.
19. Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: technical description and report of 57 cases. Spine (Phila Pa 1976). 2007; 32:643–646. PMID: 17413468.

20. Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation : results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998; 88:634–640. PMID: 9525707.

21. Yoshida M, Neo M, Fujibayashi S, Nakamura T. Comparison of the anatomical risk for vertebral artery injury associated with the C2-pedicle screw and atlantoaxial transarticular screw. Spine (Phila Pa 1976). 2006; 31:E513–E517. PMID: 16816753.

22. Yu DK, Heo DH, Cho SM, Choi JH, Sheen SH, Cho YJ. Posterior cervical fixation with nitinol shape memory loop in the anterior-posterior combined approach for the patients with three column injury of the cervical spine: preliminary report. J Korean Neurosurg Soc. 2008; 44:303–307. PMID: 19119466.

Fig. 1
A: Intraoperative findings after fixation of the C1 ring, mesh cage (arrow) and C2 lamina with a nitinol loop. B: Postoperative simple radiograph shows nitinol loop hooking the C1 ring and C2 lamina.

Fig. 2
A: Preoperative cervical computed tomography shows orthotopic type of os odontoideum. B: Magnetic resonance image shows severe cervical canal stenosis with spinal cord contusion (arrow). C: Six months postoperative cervical computed tomography shows solid bridging bone formation between C1 and C2 across the graft. D: Preoperative lateral radiograph shows orthotopic type of os odontoideum. E: Six months postoperatively, lateral radiograph demonstrates improvement of the lordotic curve and an increase in PADI from 16.00 mm to 18.53 mm. PADI: posterior atlantodental interval.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download