Abstract
A Rathke's cleft cyst (RCC) is a benign pituitary cyst derived from the remnant of Rathke's pouch, and usually presents as an intrasellar lesion with varying degrees of suprasellar extension. However, to date, a description of a primary prepontine RCC with no intrasellar component has not been reported. The author describes an exceptional case of a symptomatic RCC located behind the sella turcica in a 41-year-old woman who presented with severe headache. The author also provides an embryological hypothesis of the development of an ectopic RCC, with a special emphasis on radiologic characteristics.
Rathke's cleft cysts (RCCs) are non-neoplastic congenital lesions that develop from an epithelial remnant of Rathke's pouch, a normal component of pituitary development that gives rise to the anterior lobe, pars intermedia, and pars tuberalis of the gland. Topographically, RCCs usually occur in the sellar fossa with or without suprasellar involvement, but they can arise from every part of the craniopharyngeal duct, which is a part of Rathke's pouch11,14). Intracranial ectopic RCCs are exclusively found in the suprasellar region, likely a result of pouch remnants within the pars tuberalis above the diaphragma sellae3). In rare instances, RCCs may reside in the sphenoid sinus or clivus regions8). In this report, the author presents a case of a RCC located in the retrosellar and prepontine area.
A 41-year-old woman presented with an acute-onset headache, which progressively worsened over the following 3 days. Her condition had been unresponsive to medical treatment. This patient had signs of meningeal irritation with increased cerebrospinal fluid (CSF) cell number and protein levels. She did not show any endocrinological symptoms and signs on admission. The basal values of pituitary hormone including the gonad, thyroid, and adrenal axes were normal on laboratory evaluation.
Computed tomography (CT) scan revealed a nonenhancing homogeneous hyperdense mass confined to the retrosellar region. Mean Hounsfield unit (HU) for the central lesion was 105.1 HU. There was no bony abnormality in the sella turcica and the clivus. Magnetic resonance (MR) imaging showed an ovoid and well-demarcated mass without contrast enhancement displaying isointensity on T1-weighted images and hypointensity on T2-weighted (Fig. 1). This 25 mm-sized lesion was located just dorsal to the pituitary gland and occupied the preopontine cistern. Differential diagnosis included; craniopharyngioma, pituitary adenoma, neurenteric cyst, dermoid, and RCC.
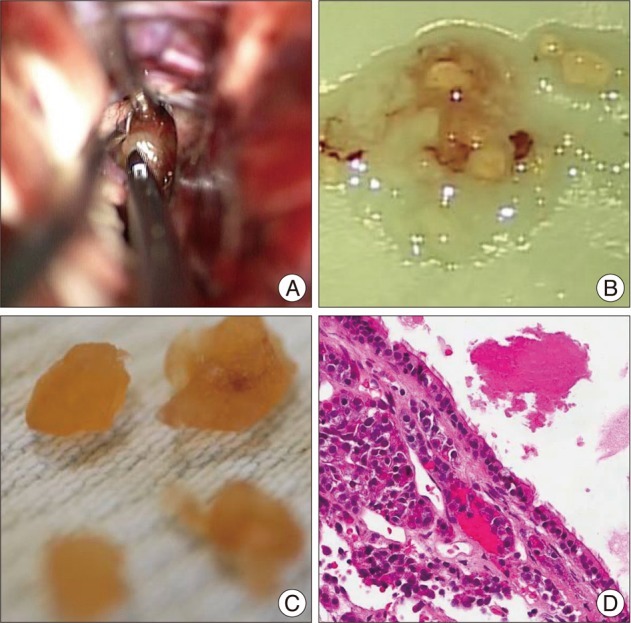
A pterional craniotomy disclosed a gray-whitish tumor, which was not attached to the infundibulum, and extended up the third ventricle. On approaching the pituitary region, the cyst was observed between the optic nerve and carotid artery. The thin capsule was opened, yellow-whitish mucinous contents evacuated, and the cyst elevated with further dissection. There was no evidence of previous hemorrhage at surgery (Fig. 2A). The tumor was gradually decompressed and totally excised through the space lateral to the carotid artery. The cyst was entirely located behind the dorsum sellae, there was no invasion into the diaphragm.
The patient recovered from the transcranial surgery. Pathological examination revealed the typical features of a RCC with columnar epitheliums and cystic contents (Fig. 2B-D). Postoperative CT scans showed no evidence of residual cyst in the prepontine cistern (Fig. 3). Her severe headache resolved postoperatively.
With the increased use and evolution of brain MR imaging technology more RCCs are being discovered; however, symptomatic cases are rare and accurate preoperative diagnoses can be difficult. Excluding pituitary adenomas, RCCs are the most common lesion in the sellar and suprasellar region. These are developmental epithelial cysts filled with mucous, gelatinous or caseous content. RCCs are well encapsulated and vary in size1). Microscopically, they are typically composed of simple or pseudostratified columnar or cuboidal epithelium, often with ciliated or mucin-secreting goblet cells.
Neuroembryologically, the origin and pathogenensis of ectopic RCC is a subject of controversy, however, it is not surprising to assume that it is similar to the mechanism for ectopic occurrence of the pituitary adenoma or craniopharyngioma2,5). Ectopic locations include the nasopharynx, the sphenoid sinus, the clivus, and the posterior fossa7,11,15). It has been proposed that RCCs originate from epithelial cell remnants of the obliterated craniopharyngeal duct along the path traversed by Rathke's pouch and that location is determined by the embryological events of the sellar and/or suprasellar region. The pars tuberalis, while developing from the ventral portion of Rathke's pouch, rotates to come in contact with the neuroectodermal layer of the developing ventral cerebral vesicle in the early embryonic period. As a result of different rates of rotation of the pars tuberalis, Rathke's pouch cells predominantly spread through sellar and suprasellar region, but few cells can be located outside the sella turcica3,8). Failure of ectopic pouch remnants beyond the pituitary fossa to regress further during development can lead to cystic dilation and formation of a symptomatic RCC.
On CT scans, the majority of RCCs are homogenous, nonenhancing, and of low-density, as are many other well-defined sellar and suprasellar lesions, including craniopharyngiomas, arachnoid cysts, and pituitary adenomas13). However, cases of mixed density RCCs with iso-, hypo-, and hyperdense foci have been reported in the literature15). The cyst in this report differed from ordinary RCCs because of its high density on CT, which was ascribed to higher protein content14). In this case, based on the CT HU density values, relatively acute hemorrhage (60-70 HU) or calcification (1000 HU) was thought unlikely and ruled out. The major differential consideration for a hyperdense RCC includes the classic colloid cyst and the rare "white" epidermoid cyst; because they may appear hyperattenuated on nonenhanced CT scans6,16). However, colloid cysts should not be mistaken for RCCs since they typically occur only at the foramen of Monro. Unlike RCCs, epidermoid cysts usually have an irregular configuration of the cyst wall and may calcify, and are usually located off midline.
Variable MR imaging characteristics of RCCs were presumed in part to be due to cholesterol contents, cell debris, mucopolysaccharides, and rarely, hemorrhage within the cysts10,16). Uncommon RCCs like the this case that have high- and isointensity on T1- and hypointensity on T2-weighted images are more likely to induce earlier symptoms, when the cysts are smaller than their CSF-like intensity counterparts12,17). A RCC with low viscosity fluid may be confused with suprasellar arachnoid cysts, since they typically have the same signal intensity as CSF. It has been suggested that the presence of waxy nodules is the most reliable diagnostic indicator of RCCs4). In the present case, the intracystic nodule was easily observed on T2-weighted images, but detection of the nodule on T1-weighted images was difficult because of similarities in the cyst fluid and nodule intensities. While T2 hypointensity is not observed in every RCC case, this is in contrast to pituitary adenomas where hypointensity on T2 would not be expected unless there were hemorrhages. RCC shows no enhancement or is limited to the cyst wall; conversely, craniopharyngiomas typically have nodular, globular, or rim enhancement on MR scanning6). In the case of ectopic RCCs in the prepontine region, the major differential diagnosis is neurenteric cyst or dermoid cyst because commonly they have a similar location15). However, dermoid cysts have the same imaging characteristics as fat because they contain liquid cholesterol. The best diagnostic clue for a neurenteric cyst is a lobulated, nonenhancing, slightly hyperintense mass in front of the medulla on both T1-weighted and T2-weighted imagings13).
RCCs may compress structures within and/or adjacent to the sella, which can elicit symptoms including visual impairment, pituitary endocrine dysfunction, and headache. Rarely, they also cause abscess formation, chronic inflammation, hyponatremia, cavernous sinus syndrome, diabetes insipidus, or meningitis1). This patient presented with severe headache of acute-onset suggestive of leakage of the cystic contents. Acute symptoms that mimicked pituitary apoplexy were noted in up to 11.0% of reported cases9).
For treating symptomatic sellar and suprasellar RCCs, the endonasal transsphenoidal route including microscopic and endoscopic is the procedure of choice. Results are reportedly good with low morbidity and recurrence rates10). Although they are rare, the transcranial approach may be required for complex cysts or entirely supra- and retrosellar lesions, which was evident in the present report. Regardless of the surgical approach chosen, treatment of retro- and suprasellar RCCs is more difficult owing to their intimate proximity to the optic chiasm and pituitary stalk3).
The author reports a rare case of a completely retrosellar type of RCC that was not attached to the pituitary fossa. The rarity of ectopic RCCs and their variable imaging features preclude preoperative diagnosis. The unique MR findings of an intracystic nodule with low signal intensity on T2-weighted image may be an indicator in differentiating RCCs from other parasellar cystic lesions.
References
1. Aho CJ, Liu C, Zelman V, Couldwell WT, Weiss MH. Surgical outcomes in 118 patients with Rathke cleft cysts. J Neurosurg. 2005; 102:189–193. PMID: 15739543.

2. Anand VK, Osborne CM, Harkey HL 3rd. Infiltrative clival pituitary adenoma of ectopic origin. Otolaryngol Head Neck Surg. 1993; 108:178–183. PMID: 8441545.

3. Barrow DL, Spector RH, Takei Y, Tindall GT. Symptomatic Rathke's cleft cysts located entirely in the suprasellar region : review of diagnosis, management, and pathogenesis. Neurosurgery. 1985; 16:766–772. PMID: 4010898.

4. Binning MJ, Gottfried ON, Osborn AG, Couldwell WT. Rathke cleft cyst intracystic nodule : a characteristic magnetic resonance imaging finding. J Neurosurg. 2005; 103:837–840. PMID: 16304987.

5. Chen CJ. Suprasellar and infrasellar craniopharyngioma with a persistent craniopharyngeal canal: case report and review of the literature. Neuroradiology. 2001; 43:760–762. PMID: 11594427.

6. Choi SH, Kwon BJ, Na DG, Kim JH, Han MH, Chang KH. Pituitary adenoma, craniopharyngioma, and Rathke cleft cyst involving both intrasellar and suprasellar regions : differentiation using MRI. Clin Radiol. 2007; 62:453–462. PMID: 17398271.

7. Chuang CC, Chen YL, Jung SM, Pai PC. A giant retroclival Rathke's cleft cyst. J Clin Neurosci. 2010; 17:1189–1191. PMID: 20627584.

8. Hanna E, Weissman J, Janecka IP. Sphenoclival Rathke's cleft cysts : embryology, clinical appearance and management. Ear Nose Throat J. 1998; 77:396–399. PMID: 9615520.

9. Kim JE, Kim JH, Kim OL, Paek SH, Kim DG, Chi JG, et al. Surgical treatment of symptomatic Rathke cleft cysts : clinical features and results with special attention to recurrence. J Neurosurg. 2004; 100:33–40. PMID: 14743909.

10. Kleinschmidt-DeMasters BK, Lillehei KO, Stears JC. The pathologic, surgical, and MR spectrum of Rathke cleft cysts. Surg Neurol. 1995; 44:19–26. discussion 26-27. PMID: 7482247.

11. Megdiche-Bazarbacha H, Ben Hammouda K, Aicha AB, Sebai R, Belghith L, Khaldi M, et al. Intrasphenoidal rathke cleft cyst. AJNR Am J Neuroradiol. 2006; 27:1098–1100. PMID: 16687551.
12. Nishioka H, Haraoka J, Izawa H, Ikeda Y. Magnetic resonance imaging, clinical manifestations, and management of Rathke's cleft cyst. Clin Endocrinol (Oxf). 2006; 64:184–188. PMID: 16430718.

13. Osborn AG, Preece MT. Intracranial cysts : radiologic-pathologic correlation and imaging approach. Radiology. 2006; 239:650–664. PMID: 16714456.

14. Panagopoulos KP, Jolesz FA, el-Azouzi M, Black PM. Mucinous cysts of the pituitary stalk. Report of two cases. J Neurosurg. 1989; 71:276–278. PMID: 2746351.
15. Ross DA, Norman D, Wilson CB. Radiologic characteristics and results of surgical management of Rathke's cysts in 43 patients. Neurosurgery. 1992; 30:173–178. discussion 178-179. PMID: 1545884.

16. Voelker JL, Campbell RL, Muller J. Clinical, radiographic, and pathological features of symptomatic Rathke's cleft cysts. J Neurosurg. 1991; 74:535–544. PMID: 2002366.

17. Zhou L, Luo L, Hui X, Chen H, Yu B, Guo G, et al. Primary Rathke's cleft cyst in the cerebellopontine angle associated with apoplexy. Childs Nerv Syst. 2010; 26:1813–1817. PMID: 20717684.

Fig. 1
Neuroimaging studies of an ectopic Rathke's cleft cyst. Computed tomography scans show a homogenous oval-shaped high density in the prepontine cistern. Magnetic resonance images depict a nonenhancing retrosellar mass with an intracystic nodule that displays iso- to slight hyperintensity on T1-weighted sequence and hypointensity on T2-weighted sequence. The nodule (*) is surrounded by thin isointense cyst fluid (arrow).
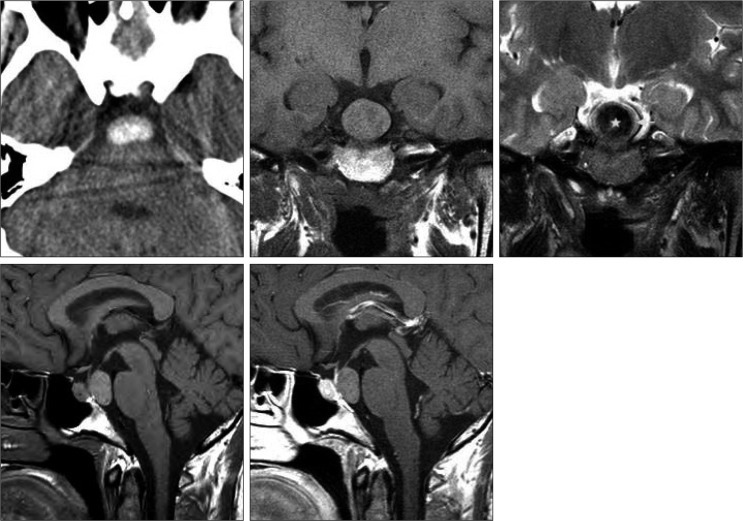
Fig. 2
Operative and pathology features of a Rathke's cleft cyst in the prepontine cistern. Intraoperative view demonstrates resection of a cyst wall with thick mucoid and white-yellow substances (A). Photomicrographs of surgical specimens show the cystic contents and the waxy nodules (B and C). Histopathological examination of cyst wall illustrates ciliated columnar epitheliums and inflammatory infiltrates (H&E, original magnification ×100) (D).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download