Abstract
Objective
The purpose of this study was to present the MRI and CT findings of solitary spinal bone lesions (SSBLs) with the aims of aiding the differential diagnoses of malignant tumors and benign lesions, and proposing a diagnostic strategy for obscure SSBLs.
Methods
The authors retrospectively reviewed the imaging findings of 19 patients with an obscure SSBL on MRI at our hospital from January 1994 to April 2011. The 19 patients were divided to benign groups and malignant groups according to final diagnosis. MRI and CT findings were evaluated and the results of additional work-up studies were conducted to achieve a differential diagnosis.
Results
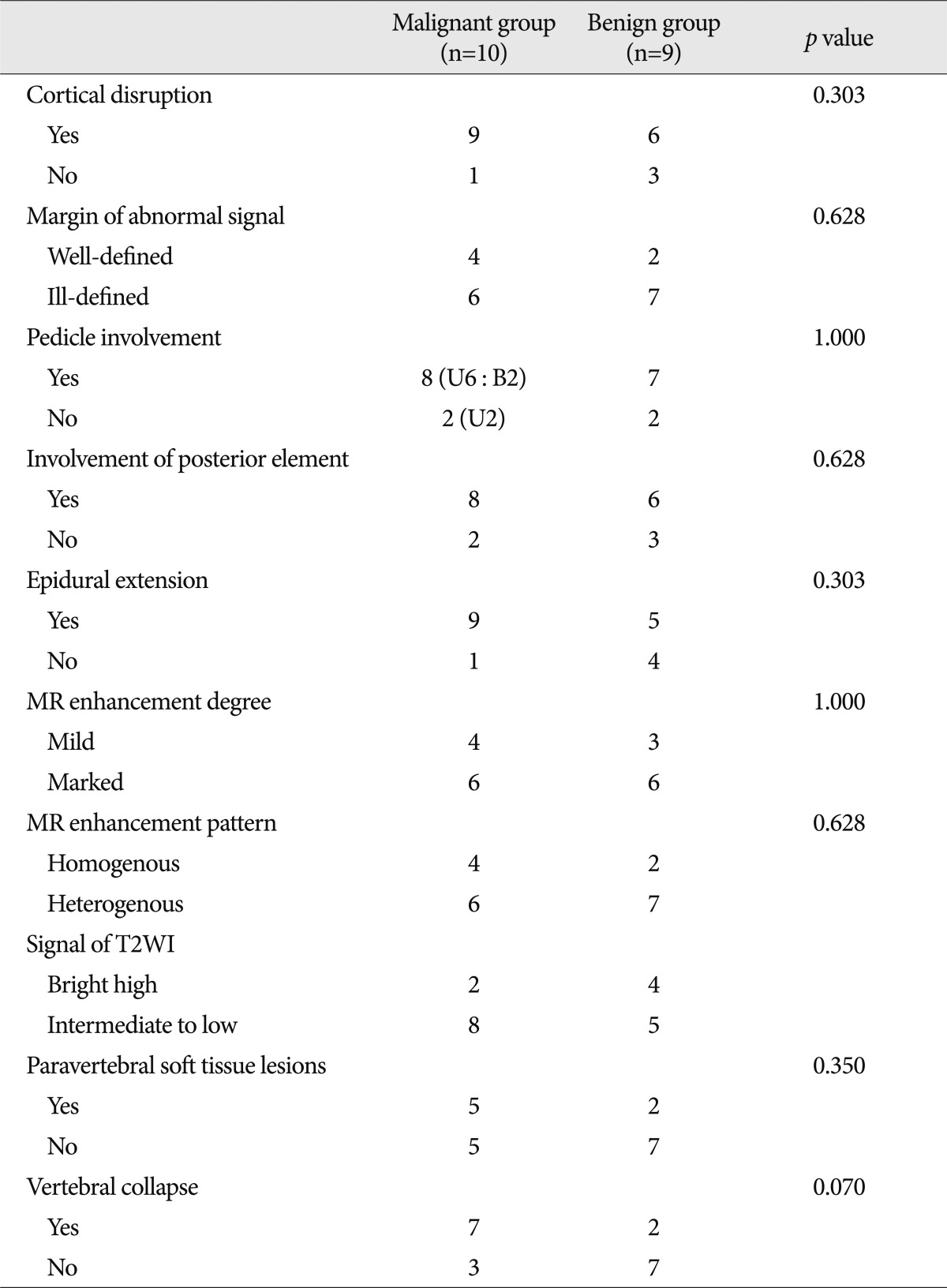
At final diagnoses, 10 (52.6%) of the 19 SSBLs were malignant tumors and 9 (47.4%) were benign lesions. The malignant tumors included 6 metastatic cancers, 3 multiple myelomas, and 1 chordoma, and the benign lesions included 4 osteomyelitis, 2 hemangiomas, 2 nonspecific chronic inflammations, and 1 giant cell tumor. No MRI characteristics examined was found to be significantly different in the benign and malignant groups. Reactive sclerotic change was observed by CT in 1 (10.0%) of the 10 malignant lesions and in 7 (77.8%) of the 9 benign lesions (p=0.005).
Conclusion
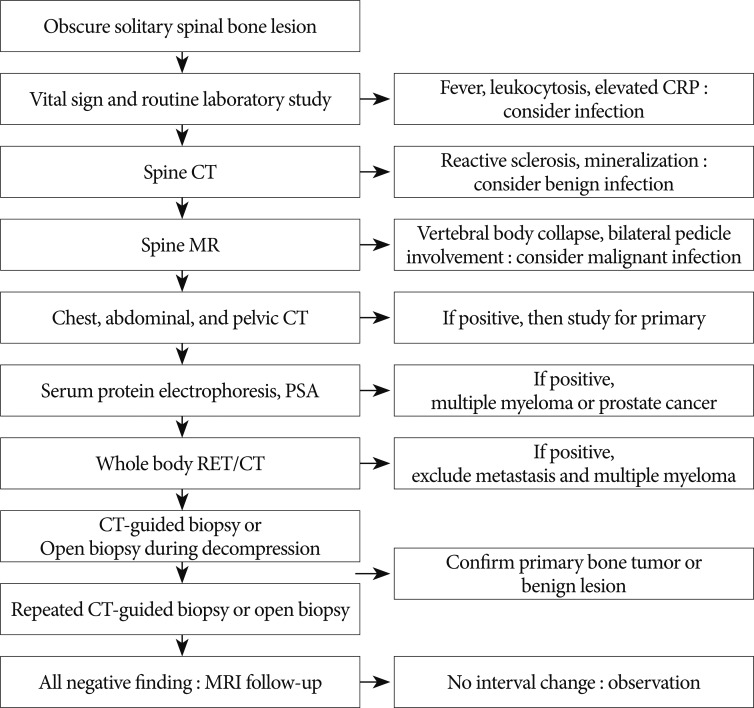
Approximately half of the obscure SSBLs were malignant tumors. CT and MRI findings in combination may aid the differential diagnosis of obscure SSBLs. In particular, sclerotic change on CT images was an important finding implying benign lesion. Finally, we suggest a possible diagnostic strategy for obscure SSBLs on MRI.
Multiple spinal bone lesions are usually malignant tumors such as metastatic disease, myeloma and lymphoproliferative disorder, and therefore these tumors can be easily diagnosed based on considerations of clinical data14). In contrast, diagnoses of solitary spinal bone lesions (SSBLs) can be difficult because a spectrum of SSBLs, including benign and malignant primary bone tumors, metastatic tumors, pseudo-tumors, can be involve the spine1,5,14,16,18). Furthermore, malignant SSBLs are associated with significant morbidity and mortality, and thus, accurate and early diagnosis is important for planning treatment.
Magnetic resonance imaging (MRI) plays a central, initial role in the differential diagnosis of SSBLs. Typical MRI findings such as location and enhancement patterns usually enable a diagnosis to be made. However, the differential diagnosis of SSBLs based on MRI findings can occasionally be difficult, because of nonspecific or atypical finding, thus, further evaluation, such as additional radiological, laboratory, and/or radionuclide studies may be necessary3,9,12,14-16). In some cases, an invasive biopsy is required to achieve a differential diagnosis, but the results may not provide final diagnosis of SSBL.
The purposes of this study were to present the MRI and CT findings of SSBLs, and our results regarding the differential diagnosis of malignant tumors and benign lesions, to suggest a diagnostic strategy for obscure SSBLs.
We retrospectively reviewed the records of 59 consecutive patients admitted for the evaluation of a SSBL found on MRI at our hospital from January 1994 to April 2011. The inclusion criteria were as follows : 1) an obscure SSBL on initial MRI requiring the differential diagnosis of a malignant tumor and benign lesion based on musculoskeletal radiologist's interpretation, 2) solitary lesion by a sequential whole spine imaging study, and 3) histological confirm based on biopsy of the spinal lesions, or the primary sites of metastatic tumors. Typical malignant tumors and benign lesions as determined by MRI were excluded based on the radiologist's opinion. Patients with a known primary malignant tumor were also excluded.
Of 59 patients, 19 fulfilled the inclusion criteria. The medical records, including the clinical manifestations and pathological results, of these 19 patients were reviewed. The 19 patients were divided into benign and malignant group based on final histological results. All MRI and CT images were reviewed by an experienced musculoskeletal radiologist. MRI findings were analyzed with respect to cortical disruption, margin of abnormal signal, pedicle involvement, posterior element involvement, degree and pattern of enhancement, epidural extension, signal of T2-weighted image (T2WI), paravertebral soft tissue lesion, and vertebral collapse. CT findings were analyzed for destructive pattern, mineralization, such as, calcification or ossification, and reactive sclerotic change.
The results of additional work-up studies performed to achieve differential diagnoses were also reviewed and evaluated. These additional studies included chest, abdominal, and pelvic CT, laboratory studies, bone scans or positron emission tomography/CT (PET/CT), and regional biopsies.
Intergroup differences of age, sex, MRI, and CT findings were analyzed using Mann-Whitney test or chi-square test (SPSS version 12.0 for Window, SPSS Inc., Chicago, IL). Statistical significance was accepted for p values of <0.05.
Patient's characteristics are shown in Table 1. The 19 patients included 8 men and 11 women of overall average age 52.8 years (range, 15-83 years). Nonspecific local pain, which affected in 15 patients, was the most common symptom. Three patients had motor weakness and one patient was asymptomatic. The lesions were located on the cervical region in 5, in the thoracic in 6, in the lumbar in 7, and in the sacral in one. According to final diagnosis, 10 (52.6%) of the 19 SSBLs were malignant tumors and 9 (47.4%) were benign lesions. Patients' mean ages were 58.4 and 46.7 years in the malignant and benign groups (p=0.236), and group gender ratios were similar.
The malignant tumors included 6 metastatic cancers, 3 multiple myelomas, and 1 chordoma. The primary histological diagnoses of metastatic tumors were lung carcinoma in 3, renal cell carcinoma in 1, cholangiocarcinoma in 1, and thyroid carcinoma in 1. Benign lesions included 4 osteomyelitis, 2 hemangiomas, 2 nonspecific chronic inflammations, and a giant cell tumor.
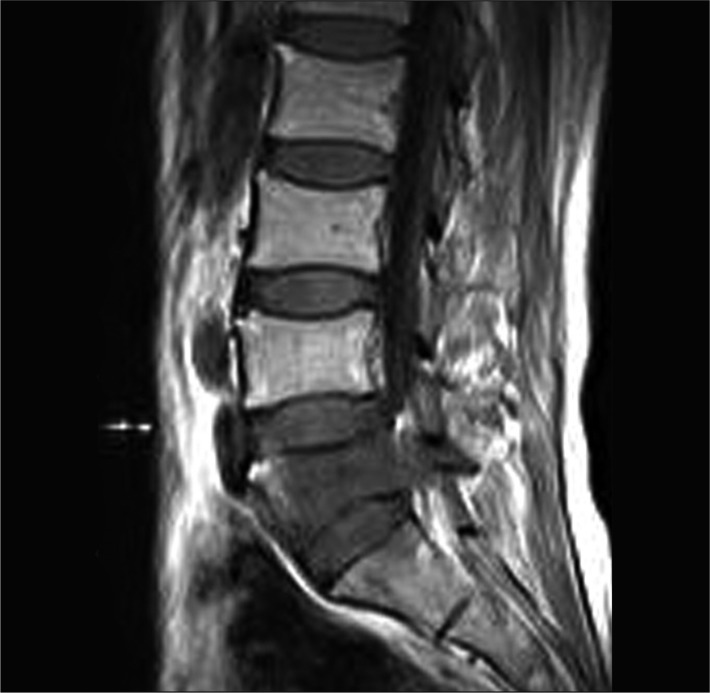
The MRI findings of malignant and benign SSBLs are described in Table 2. Vertebral body cortical disruption, lesion margins, pedicle involvement, epidural extension, MR enhancement degree and pattern, T2WI signal changes, and paravertebral soft tissue lesion were not significantly different in two groups. Two SSBLs involving bilateral pedicles were malignant tumors (Fig. 1). Vertebral collapse was observed in 7 (70.0%) of the 10 malignant lesions and in 2 (22.2%) of the 9 benign lesions, and thus, tended to be higher in malignant groups (p=0.070) (Fig. 2).
The CT findings of SSBLs are described in Table 3. Vertebral body destruction and pattern, and lesion mineralization were not significantly different in the two groups. However, reactive sclerotic change was seen in 1 (10.0%) lesion in the malignant group and in 7 (77.8%) lesions in benign group, and this difference was significant (p=0.005) (Fig. 3).
Vital signs and common laboratory test findings were non-specific, other than in a single patient with candida spondylitis who showed mild leukocytosis and a high C-reactive protein level. Conventional tumor markers including AFP, CA125, CA19-9, CEA, and PSA were checked in 6 patients in malignant group and in 5 in the benign group. Tumor markers were elevated in 3 patients with a metastatic tumor and in one patient with a benign lesion. Serum protein electrophoresis was performed for diagnosis of multiple myeloma in 5 patients in the malignant group and in 4 the benign group. A positive finding was obtained for 3 patients with multiple myeloma and for one patient with lung cancer. All 4 patients in the benign group had negative findings.
CT of the chest, abdomen, and pelvis were performed to search for primary tumors in all 19 study subjects. CT demonstrated 5 primary tumor sites except for 1 thyroid cancer. In a patient with multiple myeloma, CT showed multiple metastatic lesions in the chest and abdomen.
PET/CT was performed to search for possible metastatic and primary tumor sites in 9 patients. In a patient with thyroid cancer, the primary tumor site was demonstrated by the PET/CT. In a patient with granuloma, an additional lesion was confirmed on left acetabulum. In the other 7 patients, PET/CT provided no more information that CT of the chest, abdomen and pelvis.
A regional spinal biopsy was performed in 10 patients except for the patients with metastatic tumor and multiple myeloma. CT-guided biopsy was performed in 6 patients and open biopsy during decompression surgery was performed in 4. In 9 patients, initial biopsy findings led to final diagnosis. In one patient, first CT-guided biopsy did not lead to a final diagnosis, but repeated CT-guided biopsy confirmed the lesion as hemangioma.
Final diagnoses of the 19 SSBLs showed that 52.6% were malignant tumors and 47.4% were benign lesions. Therefore, approximately half of obscure SSBLs on MRI were malignant tumors, and most of these were secondary malignant tumors. Lung cancer and myeloma were the most common cause of malignant lesions. Chordoma was the only primary malignant tumor. Generally, metastatic disease, myeloma, and lymphoma are considered to be the most common cause of malignant spinal tumors14). Excepting hemangioma, primary benign tumors of the spine are uncommon18). Therefore, an obscure SSBL on MRI should be evaluated primarily with a focus on a metastatic tumor or myeloma. In fact, about 10% of all cancer metastases to the spine and 60% of spinal metastases are from breast, lung, or prostate cancer. Renal and gastrointestinal malignancies each account for about 5% of spinal metastasis2,10). In present study, there was no breast or prostate cancer among the SSBLs. It has been speculated that breast and prostate cancer are usually encountered as multiple metastases due to a relatively long survival9). In benign lesions, vertebral osteomyelitis predominated, but causative organisms were various, including bacteria, fungus, and mycobacterium. Furthermore, in the benign group, there were two non-specific chronic inflammations, and hemangioma and giant cell tumor were only benign tumors.
In the present study, we focused on the differential diagnosis of malignant tumors and benign lesions. In terms of demographics, ages at time of diagnosis were 58.4 and 46.7 years in malignant and benign group, respectively, which represent a non-significant. Generally, when hemangiomas are excluded from SSBLs, primary and secondary malignant tumors increase in proportion to patient's age. In patients without a known malignancy, malignant tumors increase to 50% in the fourth decade and over 90% in the seventh decade5). Fever, leukocytosis and elevation of CRP level could be characteristic for vertebral osteomyelitis. However, in our cases, vital sign and general laboratory tests provide no definite information useful for differential diagnosis, except in the single case of candida osteomyelitis. Patients with osteomyelitis showed no fever, leukocytosis, or elevation of CRP. Vertebral osteomyelitis can produce MRI patterns mimicking osseous metastases and present with nonspecific, especially in the early stages4,8). Furthermore, when evaluating SSBL, the possibility of osteomyelitis should always be considered. Essentially, clinical examination plays an important role in the diagnosis of metastasis and infection. Constant pain and weight lose are characteristic of metastasis, whereas constant pain and fever are characteristic of osteomyelitis. In addition, medical history of a percutaneous procedure, an immonocompromized state, and previous infection could be diagnostic clues of vertebral osteomyelitis.
However, the radiological findings contribute most to the differential diagnosis of SSBLs. In particular, MRI is excellent at detecting abnormalities, and has been reported to be superior to other imaging modalities in evaluation of associated softtissue, bone marrow infiltration, and intraspinal extension1,5,14,16).
MRI findings for the differential diagnosis of SSBLs include cortical disruption, margin of abnormal signal, pedicle involvement, posterior element involvement, enhancement degree and pattern, epidural extension, T2WI signal intensity, the presence of paravertebral soft tissue lesion, and vertebral collapse. Shih et al.16) reported that an ill-defined margin, pedicle involvement, a marked, heterogenous MR enhancement pattern, and an irregular nodular type paraverebral soft tissue lesion are MRI characteristics of malignant solitary vertebral collapse. In addition, pedicle change in the presence of an expansile lesion is an important MRI finding that totally excludes a benign cause. Therefore, MRI can be a useful diagnostic tool for the differential diagnosis of solitary vertebral collapse. In the present study, vertebral collapse showed a tendency to be higher in malignant group. However, MRI characteristics were not statistically significant between two groups, which may be due to our limiting the study to obscure lesions on initial MRI. In fact, definite benign and malignant lesions on MRI were excluded based on a radiologist's opinion. In addition, pedicle involvement is well-known phenomenon of metastatic tumors. However, as shown in Table 2, 7 (78%) of the 9 benign lesions showed unilateral pedicle involvement, which suggests that pedicle involvement does not imply the presence of metastatic or malignant tumor. Rather, our results indicate that bilateral pedicle involvement is probably a more reliable finding of malignant tumor. Our results are inconsistent with the previous results presenting meaningful MRI findings of malignant tumors16). We suppose that the discrepancy may be due to the inclusion criteria defined as obscure lesions on MRI. The lesions showing definite malignant features were excluded from our study. In addition, resultant cohort size was small and the MRI findings of each malignant lesion are somewhat different. Therefore, the previous MRI findings indicating malignant tumor are still important for differential diagnosis of benign and malignant lesions.
In many spinal bone tumors, MRI cannot provide further characterization of lesions due to poor detection of matrix mineralization. On the other hand, CT is useful for evaluating lesion locations and detecting bone destruction and condensation1,5,14). In particular, CT provides further information about growth rate of lesion. For example, sharp circumscribed lysis, a sclerotic rim, calcification, and ossification indicate a slow growing lesion, whereas, permeative bony destruction indicates a rapidly growing lesion. In the present study, a reactive sclerotic change was found to be statistically meaningful finding of a benign lesion. The prevalence of permeative bony destruction was relatively high for malignant lesions, but not significantly. Other bony destruction patterns were also not significantly different between the two groups. Therefore, for obscure SSBLs on MRI, CT findings, such as, reactive sclerosis could provide important differential diagnostic information. Nevertheless, for some slow-growing metastases or plasmacytomas, sclerotic lesions could be also present.
Although imaging modalities play important roles in the diagnosis, characterization and extension of spinal bone tumors, it is not enough to make a final diagnosis for obscure SSBLs, and thus, additional workup studies are required. Initially, the possibility of a metastatic tumor should be ruled out, and thus, chest, abdominal, and pelvic CT are essential. In the present study, CT was found to be useful for making a final diagnosis in solid tumor, but not for multiple myeloma, and thus, laboratory analysis including tumor makers and protein electrophoresis should be considered. However, Destombe et al. found that tumor makers are often false-positive and are of limited for identifying primary tumors3). Iizuka et al.9) reported that specific tumor makers, such as, PSA, are useful for identifying primary solid tumors. In present study, tumor marker provided little useful information for final diagnoses. Rather, than tumor markers, serum protein electrophoresis may be useful for the diagnosis of multiple myeloma.
When a CT scan fails to provide a final diagnosis, radionuclide studies, such as, bone scan and PET/CT could be considered. Bone scans (99mTc-MDP) sensitively detect spinal metastasis and allow screening of the entire skeleton in a single image, but they are relatively insensitive for multiple myeloma and tumors confined to bone marrow. Furthermore, fractures, degenerative diseases and benign lesion may be positive on bone scans6). Actually, bone scan may not aid the differential diagnosis of SSBL, and PET/CT appears to be more specific and accurate. In addition, PET/CT is useful for investigating the primary sites of metastatic tumors11). For SSBLs with a negative finding on chest, abdominal and pelvic CT, a negative PET/CT finding can rule out the presence of a metastatic tumor. Nevertheless, we recommend that inexpensive spinal CT can contribute enough the differential diagnosis of primary and benign lesions compared with PET/CT, that is, an expensive diagnostic modality.
If PET/CT findings are negative, a biopsy should be considered, though an invasive biopsy is not essential to achieve final diagnosis of metastatic tumor and hematologic tumor. However, for primary bone tumors or benign lesions, a regional biopsy can enable a final diagnosis of SSBL. Traditionally, open biopsy has been considered the gold standard for the diagnosis of musculoskeletal lesions, because it provides adequate material for histological and immunohistochemical studies in most cases. However, for vertebral and deeply seated pelvic bone lesions, open biopsy can be difficult and presents significant risks of complications12,17). Percutaneous CT-guided biopsy is both reliable and safe, and nowadays is considered the gold standard for biopsies of the musculoskeletal system13). However, for spine lesions, particularly lesions in the cervical segment, its accuracy is still lower. Accordingly, if the histological diagnosis after percutaneous biopsy is doubt or the result is not consistent with clinical and/or imaging findings, percutaneous needle biopsy should be repeated. Even repeated biopsy fails to make the histological diagnosis, serial MRI checking and clinical follow-up are recommended.
Based on our results and literature review, we suggest a possible diagnostic strategy for obscure SSBLs, as summarized in Fig. 1. However, the proposed diagnostic algorithm may be not optimal, and thus, diagnostic steps can be modified or performed at the different times based on individualized considerations.
This study has several limitations that warrant consideration. First, the cohort size was small because few patients satisfied the inclusion criteria. In addition, the definition of obscure SSBL by MRI was subject to considerable variability. Second, due to the retrospective nature of this study, additional workup studies, such as PET/CT, were not performed for all patients, and thus, we were not able to estimate the quantitative diagnostic values of individual workup studies.
Approximately half of the obscure SSBLs on MRI were found to be malignant tumors, and most of the malignant tumors were from metastasis or multiple myeloma. For benign lesions, vertebral osteomyelitis due to various causative organisms was most common. Combined CT and MRI finding was helpful for the differential diagnosis of obscure SSBLs. In particular, sclerotic change on CT images was an important finding implying benign lesion. Finally, we suggest a possible diagnostic strategy for obscure SSBLs found on MRI.
References
1. Abdel Razek AA, Castillo M. Imaging appearance of primary bony tumors and pseudo-tumors of the spine. J Neuroradiol. 2010; 37:37–50. PMID: 19781780.

2. Aebi M. Spinal metastasis in the elderly. Eur Spine J. 2003; 12(Suppl 2):S202–S213. PMID: 14505120.

3. Destombe C, Botton E, Le Gal G, Roudaut A, Jousse-Joulin S, Devauchelle-Pensec V, et al. Investigations for bone metastasis from an unknown primary. Joint Bone Spine. 2007; 74:85–89. PMID: 17218141.

4. Dunbar JA, Sandoe JA, Rao AS, Crimmins DW, Baig W, Rankine JJ. The MRI appearances of early vertebral osteomyelitis and discitis. Clin Radiol. 2010; 65:974–981. PMID: 21070900.

5. Erlemann R. Imaging and differential diagnosis of primary bone tumors and tumor-like lesions of the spine. Eur J Radiol. 2006; 58:48–67. PMID: 16431065.

6. Gosfield E 3rd, Alavi A, Kneeland B. Comparison of radionuclide bone scans and magnetic resonance imaging in detecting spinal metastases. J Nucl Med. 1993; 34:2191–2198. PMID: 8254410.
7. He MX, Zhu MH, Zhang YM, Fu QG, Wu LL. [Solitary plasmacytoma of spine : a clinical, radiologic and pathologic study of 13 cases]. Zhonghua Bing Li Xue Za Zhi. 2009; 38:307–311. PMID: 19575872.
8. Hsu CY, Yu CW, Wu MZ, Chen BB, Huang KM, Shih TT. Unusual manifestations of vertebral osteomyelitis : intraosseous lesions mimicking metastases. AJNR Am J Neuroradiol. 2008; 29:1104–1110. PMID: 18356469.

9. Iizuka Y, Iizuka H, Tsutsumi S, Nakagawa Y, Nakajima T, Sorimachi Y, et al. Diagnosis of a previously unidentified primary site in patients with spinal metastasis : diagnostic usefulness of laboratory analysis, CT scanning and CT-guided biopsy. Eur Spine J. 2009; 18:1431–1435. PMID: 19533181.

10. Katagiri H, Takahashi M, Inagaki J, Sugiura H, Ito S, Iwata H. Determining the site of the primary cancer in patients with skeletal metastasis of unknown origin : a retrospective study. Cancer. 1999; 86:533–537. PMID: 10430264.

11. Min JW, Um SW, Yim JJ, Yoo CG, Han SK, Shim YS, et al. The role of whole-body FDG PET/CT, Tc 99m MDP bone scintigraphy, and serum alkaline phosphatase in detecting bone metastasis in patients with newly diagnosed lung cancer. J Korean Med Sci. 2009; 24:275–280. PMID: 19399270.

12. Puri A, Shingade VU, Agarwal MG, Anchan C, Juvekar S, Desai S, et al. CT-guided percutaneous core needle biopsy in deep seated musculoskeletal lesions : a prospective study of 128 cases. Skeletal Radiol. 2006; 35:138–143. PMID: 16391943.

13. Rimondi E, Rossi G, Bartalena T, Ciminari R, Alberghini M, Ruggieri P, et al. Percutaneous CT-guided biopsy of the musculoskeletal system : results of 2027 cases. Eur J Radiol. 2011; 77:34–42. PMID: 20832220.

14. Rodallec MH, Feydy A, Larousserie F, Anract P, Campagna R, Babinet A, et al. Diagnostic imaging of solitary tumors of the spine : what to do and say. Radiographics. 2008; 28:1019–1041. PMID: 18635627.

15. Samartzis D, Marco RA. Osteochondroma of the sacrum : a case report and review of the literature. Spine (Phila Pa 1976). 2006; 31:E425–E429. PMID: 16741444.
16. Shih TT, Huang KM, Li YW. Solitary vertebral collapse : distinction between benign and malignant causes using MR patterns. J Magn Reson Imaging. 1999; 9:635–642. PMID: 10331758.

17. Skrzynski MC, Biermann JS, Montag A, Simon MA. Diagnostic accuracy and charge-savings of outpatient core needle biopsy compared with open biopsy of musculoskeletal tumors. J Bone Joint Surg Am. 1996; 78:644–649. PMID: 8642019.

18. Theodorou DJ, Theodorou SJ, Sartoris DJ. An imaging overview of primary tumors of the spine : Part 1. Benign tumors. Clin Imaging. 2008; 32:196–203. PMID: 18502347.
Fig. 1
Axial T1-weighted MR images showing SSBLs. A benign lesion involving unilateral pedicle (A) and a malignant lesion involving bilateral pedicles (B).
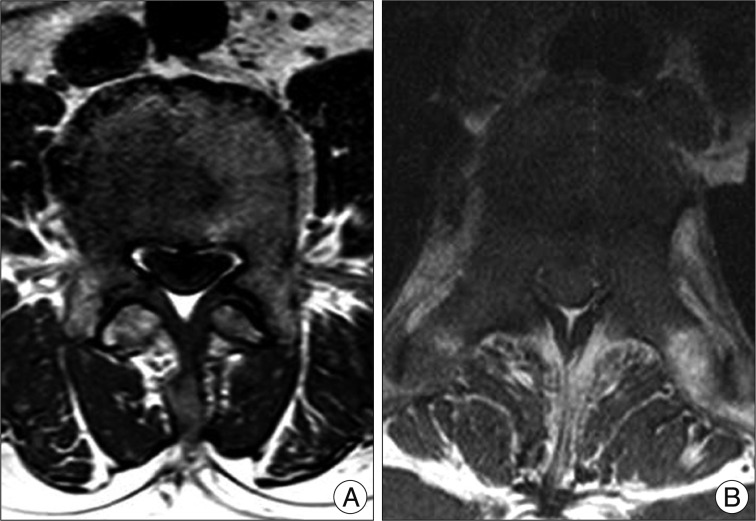
Fig. 3
Imaging findings of a SSBL diagnosed as nonspecific chronic inflammation (Case 18). Sagittal T1-weighted and axial gadolinium-enhanced MR images show a solitary lesion on T3 (A and B). Axial CT scan shows reactive sclerotic change in the lesion (C).





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download