Abstract
Objective
To prospectively assess the diagnostic and clinical value of a new technique (3-tesla magnetic resonance myelography, 3T MRM) as compared to computed tomographic discography (disco-CT) in patients with far lateral disc herniation.
Methods
We evaluated 3T MRM and disco-CT of 25 patients, whom we suspected of suffering from far lateral disc herniation. Using an assessment scale, 4 observers examined independently both 3T MRM and disco-CT images. We analyzed observer agreement and the accentuation of each image.
Far lateral disc herniation has several terms. The terms of foraminal, intraforaminal, far-lateral, and extreme-lateral identify a disc herniation within or lateral to the limits of the intervertebral foramen or lateral interpedicular compartment (LIPC)33). Although the terms are a little bit different, they define the disc herniation as occurring beneath or lateral to the vertebral facet1,3,18,20,22). The reported incidence of far lateral lumbar disc herniation varies from 0.7% to 11.7%2,23,27,28). Because the herniated disc is lateral to the dural sac, computed tomographic (CT) myelography and myelography typically fails to diagnose these lesions. It is a relatively common for clinicians to misdiagnosis patients with degenerative lumbar disc disease if it affects this area. Surgeon should take appropriate surgical procedure into consideration that is why extraforaminal nerve root entrapment in far lateral disc herniation requires extraforaminal exploration for enough decompression.
Recently, physicians have used magnetic resonance imaging (MRI) to diagnosis lumbar degenerative disease. However, the accurate diagnosis of far lateral lumbar disc herniation presents difficulty. At present, one of the most effective diagnostic tool for far lateral disc herniation is disco-enhanced computed tomography (disco-CT). Although only this examination could differentiate disc herniation from other pathological conditions responsible for extreme lateral nerve root entrapment, it is an invasive method.
With the above in mind, we aimed to demonstrate how 3-tesla magnetic resonance myelography (3T MRM) compared to disco-CT could be a useful method for diagnosing far lateral lumbar disc herniation.
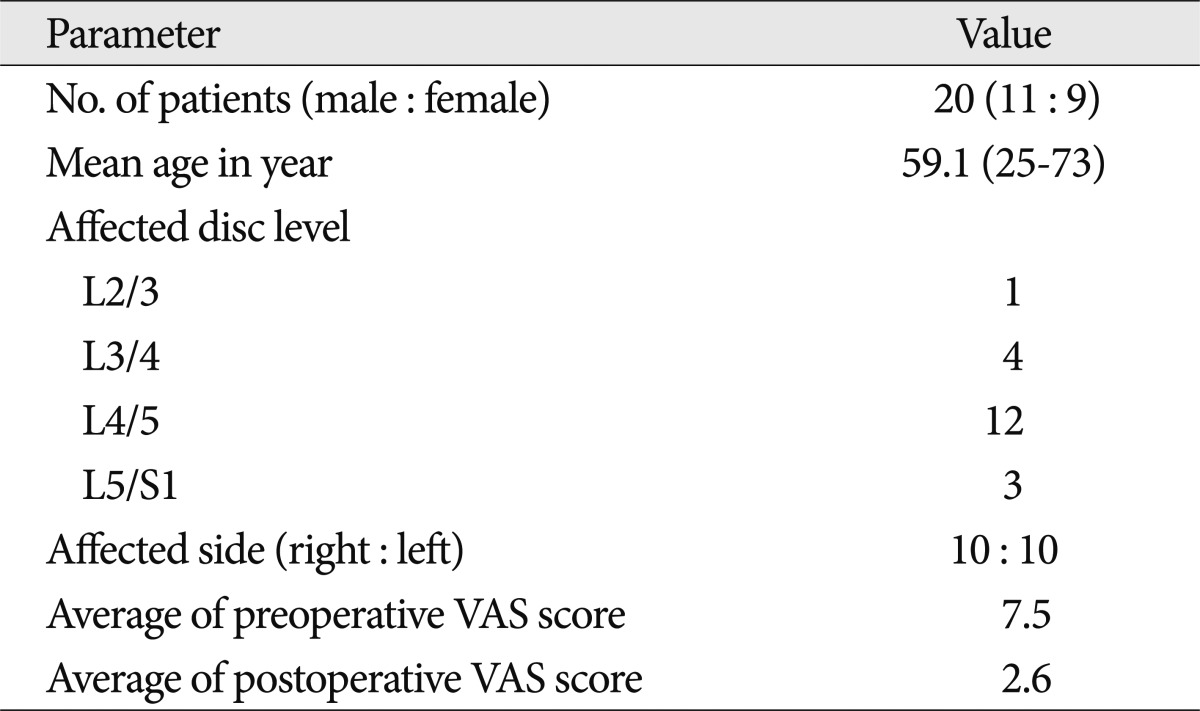
Between May 2010 and October 2011, 25 newly-admitted patients suspected of suffering from far lateral lumbar disc herniation were referred to our department. Previously, all patients underwent conventional MRI and CT. Among these 25 patients, we finally diagnosed 20 patients of the far lateral lumbar disc herniation by means of clinical findings, 3T MRM and disco-CT. Five patients who were not diagnosed as far lateral lumbar disc herniation were excluded from this study. We performed our clinical evaluations of the operative results on pre- and post-operative visual analogue scale (VAS) scores. We summarized demographic characteristics and clinical variables of the patients in Table 1.
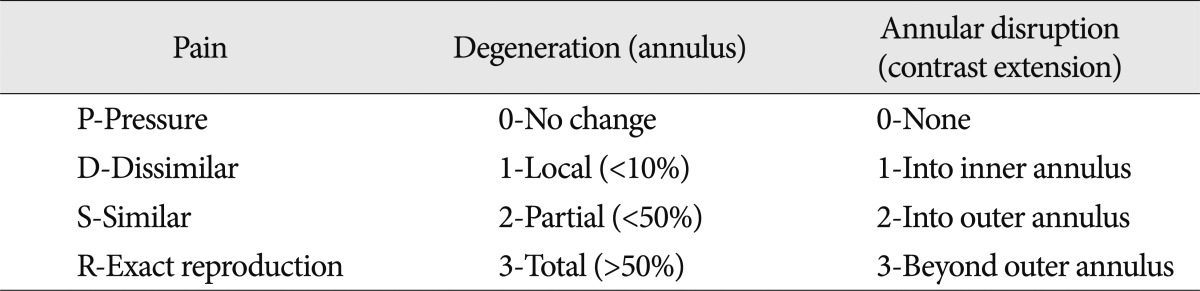
All participating patients underwent disco-CT to detect far lateral disc herniations. We completed each discography at the level responsible for the nerve root entrapment, as suggested by the CT, MRI and the clinical findings. We used the posterolateral approach, under local anesthesia, placing a 3.5-inch, 24-gauge spinal needle across the spinal canal and into the center of the nucleus and injecting up to 3.5 mL of metrizamide (concentration, 180 mgI/mL). Generally, we performed each Disco-CT from L2 to S1, with 5-mm sections, using both bony and soft tissue window settings (16-slice MDCT, Simens, Erlangen, Germany) immediately after discography. We evaluated the results according to the Dallas Discogram description11) in Table 2.
We performed the MRI with a 3-T imager (Magnetom Verio; Siemens Medical Solutions, Erlangen, Germany), using the Medic 3D sequence and obtaining all images with spine-array coils, with the patient in the supine position. For 3D-MRI images, we used echo time of 12 ms and repetition time of 22 ms, a flip angle of 20 degrees, and a matrix of 224×320. All images were completed in 399 seconds. This method is very sensitive to the presence of water in tissues and allows the suppression of adipose tissue, as in a conventional T2 image. The scans provided coronal views, and the slice thickness was 1.5 mm.
Then, we studied each patient to identify the following : 1) compression of the nerve roots and ganglions, 2) signal changes (due to perineural edema and degenerative changes) and thickening of the spinal nerve roots and ganglions. The 3T MRM technique provided a stereoscopic view of the spinal cord and nerve roots, including the dorsal root ganglia; 3T MRM can show both sides of the spinal cord and the nerve roots in one picture.
We preferred the paramedian approach, because this approach is familiar to us. We operated on 20 patients, who had finally received diagnoses of far lateral disc herniation via these methods. The same neurosurgeon operated on each patient and used the same procedure, to reduce variation in the operative results.
A professional statistician performed statistical planning and analysis for this study, using SPSS software, version 17.0 for Windows (SPSS, Chicago, IL, USA). We employed independent t-test to evaluate the difference of mean VAS score between 5 patients with nerve root signal changes on MRM and others.
Of the 25 cases, disco-CT demonstrated far lateral lumbar disc herniation in 20 patients. The rest of the patients (5/25) had negative findings. The disc levels of 20 patients were 1 at the L2-L3 level, 4 at the L3-L4 level, 12 at the L4-L5 level and 3 at the L5-S1 level. No complications were noticed. According to the Dallas Discogram description, 20 patients had total (>50%) annular degeneration and 5 of them had contrast extension beyond the outer annulus. Pain produced by disc injection was similar or an exact reproduction of the original pain. We could make an accurate diagnosis without much difficulty using these combined diagnostic modalities in conjunction with the clinical features.
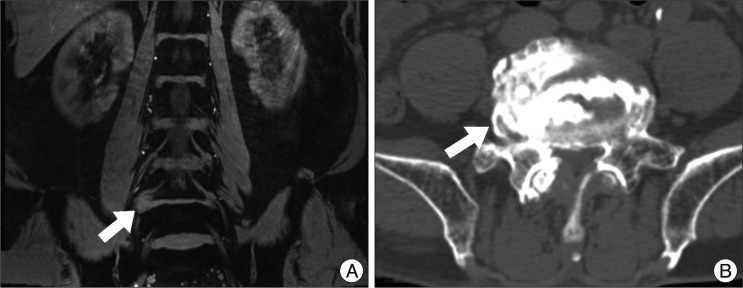
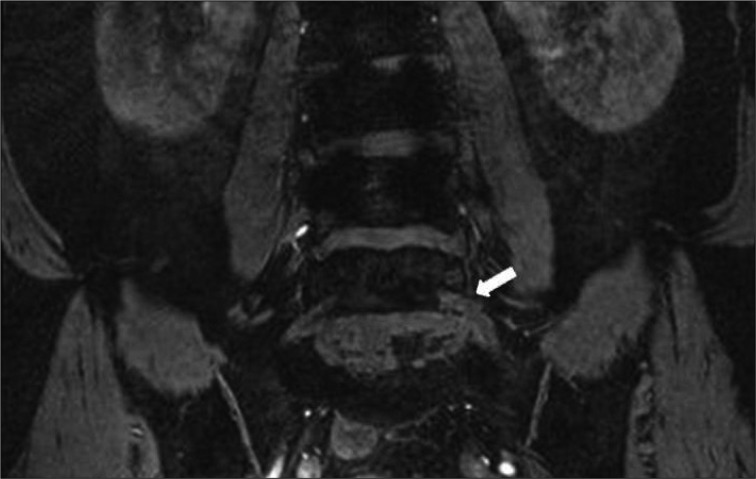
Using an assessment scale (nerve root compression, signal change), 4 observers (1 board-certified radiologists and 3 board-certified neurosurgeon) evaluated all patients by 3T MRM and independently checked the pathologic changes in all patients. Only when the all of obsevers agreed to diagnose of far lateral disc herniation, the definitive diagnosis was reached. Using 3T MRM, we diagnosed a far lateral lumbar disc herniation (nerve root compression) in 20 cases. Surprisingly, 3T MRM showed same results as disco-CT did and we demonstrated a case (Fig. 1). In addition, we detected signal changes due to damaged nerve roots in 5 patients (Fig. 2). The 3T MRM also showed the dorsal root ganglion and nerve roots, with surrounding bony structures and disc materials.
For evaluation of 3T MRM, we checked VAS score difference and signal change. The patients with signal changes and thickening of the spinal nerve roots had higher preoperative VAS scores than other patients did. However, this information had no clinical value (p=0.185). We found complete matching, and observer agreement, between high resolution images of 3T MRM and disco-CT for diagnosing far lateral disc herniation.
The condition of far lateral lumbar disc herniation usually requires surgical treatment, conservative management is only occasionally successful (10%)8,9). Abdullah et al.1) first accurately described the symptoms of lateral lumbar disc herniation, as others did later4,6,18,25,31). The symptoms comprise minimal lumbar pain and lower limb pain in the area innervated by the compressed root, often with accompanying sensorial and/or motor deficits. Symptoms alone do not differentiate this type of hernia from other hernias or compression syndromes. Therefore, diagnostic certainty is possible only with instrumental investigation.
Lindblom24) developed the discography technique in the early 1940s, partially in the hope of diagnosing such lesions. Although discography gained some popularity in the 1950s and 1960s, physicians have not utilized it widely. With the advent of thin-section, high-resolution CT, physicians can confidently diagnose the more common posterolateral and midline disc herniations without the use of intravenous or intrathecal contrast enhancement. CT may suggest the more unusual extraforaminal disc herniation, but CT done after discography allows the physician to make the diagnosis10,14,17,30,35,36). Myelography is neither sensitive nor specific. Discography is more useful than myelography, it played an ancillary role in the diagnosis of lateral lumbar disc herniation in the past; however, it is an invasive and low specificity procedure that is not always conclusive1).
Although conventional MRI provide more information than CT scan, definitive diagnosis of far lateral disc herniation through conventional MRI is still difficult. Recently, Heo et al.15) reported that in 9 of 10 patients (90.0%), nerve root compression by the herniated disc in the extraforaminal area was clearly demonstrated when compared with the asymptomatic contralateral side by using of oblique lumbar MRI technique. MRM is a relatively new imaging sequence, which is very heavily T2-weighted and produces high signal from water, with signal minimization from solid non-water structures. This imaging sequence produces similar images to conventional myelography19,29). It was first described in 199213,21,34).
O'Connell et al.26) described that the utility of the MRM in establishing the diagnosis was graded on a 4-point scale. Grade 0 and 1 indicated that it contributed no additional information or any significant information so could provide no more information than conventional MRI sequence. Grade 2 and 3 indicated that MRM helped establish the diagnosis or was essential to establish the ultimate diagnosis. According to this 4-point scale, all of our cases corresponded to grade 2 or 3. To date, MRM has shown results comparable to conventional myelography in a few studies5,7,12,16,32), but they showed no clinical correlations.
MRM is a non-invasive technique proven effective in the study of nerve root compression and spinal canal stenosis11,26). Nowadays, physicians mainly use this technique as a complement to a conventional MR examination, to evaluate nerve sheath impingement and spinal canal stenosis. Despite these studies, no studies have yet scientifically validated MRM as a technique that enhances the diagnostic accuracy of MRI in far lateral disc herniation. This may be due to poor resolutions of MRI such as 1.5 T MRI or less. Until now, no studies have reported regarding the usefulness of MRM images in assessing far lateral discs. At present, one of the most effective diagnostic tool for far lateral disc herniation is disco-enhanced computed tomography (disco-CT). We found complete matching, and observer agreement, between high resolution image of 3T MRM and disco-CT for diagnosing far lateral disc herniation. Therefore, we conducted a prospective study to evaluate the value of 3T MRM comparing with disco-CT.
References
1. Abdullah AF, Ditto EW 3rd, Byrd EB, Williams R. Extreme-lateral lumbar disc herniations. Clinical syndrome and special problems of diagnosis. J Neurosurg. 1974; 41:229–234. PMID: 4841878.
2. Abdullah AF, Wolber PG, Warfield JR, Gunadi IK. Surgical management of extreme lateral lumbar disc herniations : review of 138 cases. Neurosurgery. 1988; 22:648–653. PMID: 3374776.

3. Autricque A, Lesoin F, Bouasakao N, Clarisse J, Jomin M. [Surgical treatment of lumbar foraminal disk herniation. Value and indications for an interlaminar and extra-articular combined approach]. J Chir (Paris). 1989; 126:338–343. PMID: 2745586.
4. Brown LJ. Definitive diagnosis of extreme lateral lumbar disc herniation. Surg Neurol. 1987; 27:373–376. PMID: 3824144.

5. Crispino M, Gasparotti R, Pavia M, Bonetti M, Pittiani F, Prandini F, et al. [Magnetic resonance myelography. Preliminary experience]. Radiol Med. 1995; 89:42–48. PMID: 7716310.
6. Deburge A, Barre E, Guigui P. [Lateral lumbar disk herniation]. Chirurgie. 1994-1995; 120:568–571. PMID: 7555357.
7. Eberhardt KE, Hollenbach HP, Tomandl B, Huk WJ. Three-dimensional MR myelography of the lumbar spine : comparative case study to X-ray myelography. Eur Radiol. 1997; 7:737–742. PMID: 9166575.

8. Epstein NE. Evaluation of varied surgical approaches used in the management of 170 far-lateral lumbar disc herniations : indications and results. J Neurosurg. 1995; 83:648–656. PMID: 7674015.

9. Epstein NE. Foraminal and far lateral lumbar disc herniations : surgical alternatives and outcome measures. Spinal Cord. 2002; 40:491–500. PMID: 12235530.

11. Ferrer P, Martí-Bonmatí L, Mollá E, Casillas C. [Value of MR myelography in the diagnosis of the spine disorders]. Med Clin (Barc). 2000; 115:366–369. PMID: 11262351.
12. Freund M, Hutzelmann A, Steffens JC, Buhl R, Heller M. [MR myelography in spinal canal stenosis]. Rofo. 1997; 167:474–478. PMID: 9440892.
13. el Gammal T, Brooks BS, Freedy RM, Crews CE. MR myelography : imaging findings. AJR Am J Roentgenol. 1995; 164:173–177. PMID: 7998533.
14. Grubb SA, Lipscomb HJ, Guilford WB. The relative value of lumbar roentgenograms, metrizamide myelography, and discography in the assessment of patients with chronic low-back syndrome. Spine (Phila Pa 1976). 1987; 12:282–286. PMID: 2954225.

15. Heo DH, Lee MS, Sheen SH, Cho SM, Cho YJ, Oh SM. Simple oblique lumbar magnetic resonance imaging technique and its diagnostic value for extraforaminal disc herniation. Spine (Phila Pa 1976). 2009; 34:2419–2423. PMID: 19829256.

16. Hofman PA, Wilmink JT. Optimising the image of the intradural nerve root : the value of MR radiculography. Neuroradiology. 1996; 38:654–657. PMID: 8912322.

17. Holt EP Jr. The question of lumbar discography. J Bone Joint Surg Am. 1968; 50:720–726. PMID: 5658557.

18. Jackson RP, Glah JJ. Foraminal and extraforaminal lumbar disc herniation : diagnosis and treatment. Spine (Phila Pa 1976). 1987; 12:577–585. PMID: 3660085.

19. Jensen MC, Kelly AP, Brant-Zawadzki MN. MRI of degenerative disease of the lumbar spine. Magn Reson Q. 1994; 10:173–190. PMID: 7811610.
20. Kornberg M. Extreme lateral lumbar disc herniations. Clinical syndrome and computed tomography recognition. Spine (Phila Pa 1976). 1987; 12:586–589. PMID: 3660086.
21. Krudy AG. MR myelography using heavily T2-weighted fast spin-echo pulse sequences with fat presaturation. AJR Am J Roentgenol. 1992; 159:1315–1320. PMID: 1442408.

22. Kunogi J, Hasue M. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine (Phila Pa 1976). 1991; 16:1312–1320. PMID: 1750006.

23. Kurobane Y, Takahashi T, Tajima T, Yamakawa H, Sakamoto T, Sawaumi A, et al. Extraforaminal disc herniation. Spine (Phila Pa 1976). 1986; 11:260–268. PMID: 3715625.

24. Lindblom K. Diagnostic puncture of intervertebral disks in sciatica. Acta Orthop Scand. 1948; 17:231–239. PMID: 18879767.

25. Monod A, Desmoineaux P, Deburge A. [Lateral lumbar disk hernia]. Rev Chir Orthop Reparatrice Appar Mot. 1990; 76:538–545. PMID: 2151475.
26. O'Connell MJ, Ryan M, Powell T, Eustace S. The value of routine MR myelography at MRI of the lumbar spine. Acta Radiol. 2003; 44:665–672. PMID: 14616212.
27. O'Hara LJ, Marshall RW. Far lateral lumbar disc herniation. The key to the intertransverse approach. J Bone Joint Surg Br. 1997; 79:943–947. PMID: 9393908.
28. Porchet F, Fankhauser H, de Tribolet N. Extreme lateral lumbar disc herniation : clinical presentation in 178 patients. Acta Neurochir (Wien). 1994; 127:203–209. PMID: 7942204.

29. Ross JS, Modic MT. Current assessment of spinal degenerative disease with magnetic resonance imaging. Clin Orthop Relat Res. 1992; 68–81. PMID: 1600674.

30. Sachs BL, Vanharanta H, Spivey MA, Guyer RD, Videman T, Rashbaum RF, et al. Dallas discogram description. A new classification of CT/discography in low-back disorders. Spine (Phila Pa 1976). 1987; 12:287–294. PMID: 2954226.

31. Santini A, Pitto RP. [Ernie del disco extraforaminali della colonna lombare]. Giorn Ital J Ortop Trauma. 1991; 17:359–363.
32. Scarabino T, Giannatempo GM, Perfetto F, Popolizio T, Salvolini U. [Magnetic resonance myelography with a fast-spin-echo sequence]. Radiol Med. 1996; 91:202–206. PMID: 8628931.
33. Tessitore E, de Tribolet N. Far-lateral lumbar disc herniation : the microsurgical transmuscular approach. Neurosurgery. 2004; 54:939–942. discussion 942. PMID: 15046661.

34. VanDyke CW, Modic MT, Beale SM, Amartur S, Ross JS. 3D MR myelography. J Comput Assist Tomogr. 1992; 16:497–500. PMID: 1592941.

35. Videman T, Malmivaara A, Mooney V. The value of the axial view in assessing discograms. An experimental study with cadavers. Spine (Phila Pa 1976). 1987; 12:299–304. PMID: 3589824.

36. Weinstein J, Claverie W, Gibson S. The pain of discography. Spine (Phila Pa 1976). 1988; 13:1344–1348. PMID: 2463678.

Fig. 1
Imaging studies of 65-year-old man with right sciatica. 3-Tesla magnetic resonance myelography (3T MRM) shows same results as computed tomography discography (disco-CT). A : 3T MRM demonstrates right sided far lateral disc herniation at L4/5 level (white arrow) compressing L4 nerve root. B : Disco-CT demonstrates right sided far lateral disc herniation (white arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download