Abstract
Objective
This is prospective study of clinical outcomes of percutaneous plasma disc coagulation Therapy (PDCT) in patients with herniated lumbar disc disease (HLD) to evaluate the safety and efficacy in its clinical application and usefulness as a reliable alternative to microscopic discectomy.
Methods
Forty-six patients were enrolled in this study from April 2006 to June 2010. All patients had one-level HLD. Disc degeneration was graded on routine T2-weighted magnetic resonance Image (MRI) using the Pfirrmann's grading system and all index levels were grade 3 and grade 4. Indications for surgery were radiculopathy caused by disc protrusion with soft consistency. MRI was done at one month after the procedure in all patients to check post-PDCT change. The clinical outcomes were evaluated using Visual Analog Scales (VAS) score and MacNab's criteria.
Results
This study was approved by the Institutional Review Board of our institution. The age of the study population ranged from 16 to 59 years with a mean age of 37.2 years. There were 29 males and 17 females in this study. The mean period of clinical follow-up was 21 months. The average preoperative VAS score for radiculopathy was 7.4±1.4, while the final follow-up VAS score was 1.4±0.7 (p<0.001). In MacNab's criteria, 41 patients (89.1%) had achieved favorable improvement (excellent and good) until later follow-up. There were one patient from infection and two patients who needed to convert to open discectomy.
Microscopic discectomy has been a gold standard of treatment in patients with herniated lumbar disc diseases resulting in radiculopathy. It needs to dissect muscles and make a bony work including facetectomy which may cause postoperative undesirable results such as postoperative back pain, wound infection and instability to lumbar spine13,15,26).
Minimally invasive procedures, such as chemonucleolysis, nucleoplasty, percutaneous laser disc decompression (PLDD), intradiscal electrothermal therapy (IDET), decompressor, etc., have been recently introduced and performed to minimize procedure related muscle and ligament injury2,8,9,11,17,19,22,27,29). Their clinical outcomes and benefits did not reach the outcomes of microscopic discectomy and might cause complications which were not easy to deal32). Radiofrequency treatment is inaccurate and difficult to point out the lesioning area which can be related to high recurrence rate28). Laser treatment modality also has unsatisfactory clinical result and relapse rate because enough energy can not transfer to lesion area because of their conductivity and directionality4,27).
Percutaneous plasma disc coagulation therapy (PDCT) was invented to correct these weak points. PDCT uses laser source called plasma light that the rays generated in the module are concentrated at the end of dome-shaped fiber and do not travel linearly. PDCT can provide sufficient energy and transfer it to the lesion area without damage to surrounding soft and neural tissues.
This is a prospective study of clinical outcomes of PDCT in patients with herniated lumbar disc disease (HLD) to evaluate the safety and efficacy in its clinical application and usefulness as a reliable alternative to microscopic discectomy.
This study was approved by the Institutional Review Board at our institution. Between April 2006 and June 2010, 46 patients were enrolled in this study. Disc degeneration was graded on routine T2-weighted magnetic resonance image (MRI) using the Pfirrmann's grading system in all patients (Table 1)24). Grading was done on T2-weighted midsagittal (repetition time 5000 msec/echo time 130 msec) fast spin-echo images.
Inclusion criteria included patients under 60 years old, single level HLD causing radiculopathy which had no improvement after conservative treatment for at least 6 weeks, protruded disc, and disc degeneration with grade 3 and grade 4 in Pfirrmann's grade. Exclusion criteria were extruded disc herniation, spinal stenosis, existence of segmental instability or spondylolisthesis at the index level, infection, neoplastic disease, hemorrhagic diathesis, metabolic bone disease, previous surgery at the index level, and grade 5 Pfirrmann's grade.
MRI was done at one month after the procedure in all patients to check post-PDCT change. We evaluated clinical outcomes and postoperative complications at 1 month, 2 months, 6 months and every year after the procedure. Preoperative and final follow-up Visual Analog Scales (VAS) for radiculopathy were prospectively collected and used in this analysis. The measurement was assessed using a 10-point VAS with endpoint anchors of no pain (0 point) and severe pain (10 point). Results were also evaluated according to modified MacNab's criteria and categorized as excellent, good, fair, or poor.
Pre- and postoperative VAS scores for radiculopathy were compared using two-sample t-tests paired for means. A p value of <0.05 was regarded as significant.
PDCT equipment (Jeisys, Seoul, Korea) uses 980 nm wave-length diode laser as the light source and dome-shaped active fiber (plasma fiber) generates multi-wavelength plasma light in the range of 550 nm-1800 nm from the laser. Plasma fiber for PDCT was developed in 2006. Plasma fiber system can also set up a standardized process of PDCT established by computerized value of total Joule (J). Unlike a conventional laser system, it enables to reinforce an irradiation because all the every irradiation is condensed at the tip of the plasma fiber.
Under local anesthesia, the patient was placed in supine position. A diameter of needle was 1.2 mm. It was inserted percutaneously 8-10 cm away from the midline on the symptomatic side and obliquely advanced into the intervertebral disc space at the index level through the Kambin's triangle. Three-way valve was connected after the needle insertion to check the ventilation of evaporated gas during the procedure. Under C-arm monitor, 0.4 mm diameter plasma optical fiber was inserted into the intervertebral disc through the needle sheath. Plasma light was irradiated at 25W output to total energy of 500 J. The tip of the plasma fiber is rounded so that the rays do not travel straight forward but concentrated at the tip, raising the temperature up to 1000℃ at the tip. We made the three lesions. The first lesion (a) was made at transitional area between annulus fibrosus and nucleus pulposus which was just beneath the herniated disc portion. The second lesion (b) was made at the center of intervertebral disc. The third lesion (c) was made between (a) and (c). During the procedure, we checked patient's condition and ventilation of evaporated gas through opening the three way valve (Fig. 1).
Forty-six patients were enrolled in this study. This study consisted of 29 men and 17 women whose mean age was 37.2 years (range : 16-59). Symptom duration ranged from 6 weeks to 15 weeks (mean 8.5 weeks). The mean procedure time was 33 minutes. All patients were discharged right after the procedure. All the patients were periodically followed up in the outpatient clinic after the procedure. Median follow-up period was 21 months (range 6 to 36 months). There was no complication related to the procedure during the period.
The mean pre-PDCT VAS score was 7.47 (range 0 to 10). VAS score was decreased down to 2.37 right after the procedure and well maintained until final follow-up. The mean post-PDCT VAS score was 1.5 at final follow-up. This difference between pre-PDCT and post-PDCT VAS score was statistically significant (p<0.001) by paired t-test (Fig. 2).
The results in MacNab's criteria were excellent in 26 patients, good in 15 patients, fair in 3 patients and poor in 2 patients (Fig. 3). Forty-one patients (89.1%) showed excellent and good results in MacNab's criteria right after the procedure and well maintained until final follow-up. Three patients with fair outcome had 50% reduction of radiculopathy after procedure and had been taking pain medications. Two patients with poor outcome showed no improvement after the procedure and needed to convert to open discectomy.
We checked intervertebral disc degeneration of index level using Pfirrmann's grading system. Pfirrmann's grades were 14 patients in grade 3 and 32 patients in grade 4 before the procedure. MRI were done at 1 month after the procedure in all patients to check post-PDCT change. Fourteen patients showed decreased severity of disc herniation at the index level after PDCT (Fig. 4). The degree of disc herniation had no change in 32 patients. There was one case of spondylodiscitis which was well treated with antibiotics.
In general, patients with HLD can be managed with conservative treatments. Decompression surgery should be considered for patients who experience neurologic deterioration during the period of conservative treatment. Microdiscectomy has been widely performed as a gold standard treatment25). Microdiscectomy can be performed in any type of disc herniation which is extruded or protruded. Microdiscectomy provides good clinical outcome in patient with HLD. However, the complication rate of lumbar discectomy has been reported as 2-14%18,31), and injury of normal spinal ligament and muscle structures at the index level is inevitable. In addition, excessive removal of the nucleus may induce collapsed disc space25), which may cause undesirable results sometimes. Especially, There is sometimes a possibility that microcxdiscectomy can be an overtreatment for protruded and not ruptured HLD with moderate or severe degree. Partial removal of nucleus with minimal injury of surrounding normal ligament and muscle structures has been shown to decompress herniated disc, to relieve pressure on nerve roots and to maintain disc height20). Lumbar transforaminal epidural steroid injection has showed the short-term relief of radicular pain but long-term relief in a few studies3). Moreover one study showed that patients treated with PDD had significantly reduced pain and better quality of life scores than those treated using repeated transforaminal epidural steroid injection14).
Minimally invasive procedures have been developed to minimize the occurrence of morbidity related to open surgery. Advantages of all minimally invasive procedures are small incision, less muscle and ligament injury, no need for general anesthesia, and short hospital stay. However, each procedure has limitations and weak points such as inadequate decompression, rigid cannula, and difficulty in usage. Also, there are only few procedures which are available for the patients with HLD to alleviate radiculopathy8,11). PDD for symptomatic contained cervical disc herniation showed good results more than conservative treatments5). In patients with HLD, there is evidence that early intervention including surgery provides for a better short-term relief of radicular pain as compared to prolonged conservative care16), and PDCT outcomes showed same tendency as early surgery respect to improvement of VAS pain score. Moreover, minimally invasive procedures can be a good treatment modality in patients who are not available for open surgery because of their poor general conditions or who have an antipathy to open surgery.
PDCT can be a one of minimally invasive treatment option for HLD refractory to conservative treatment. Clinical improvement in minimally invasive treatments using laser energy is based upon laser-induced evaporation of water within the disc; this results in a very slight decrease in disc size due to water loss. Because the intervertebral disc is essentially a closed hydraulic system, a small decrease in volume leads to a significantly larger decrease of intradiscal pressure; in vitro experiments confirm this10,11,27,29,32). Laser energy is applied through the fiber, resulting in vaporization of nucleus pulposus contents27,32). Short term decrease in pressure is due to evaporation of water content within the nucleus pulposus; long term effects are thought to be due to protein denaturation, which limits the ability of the nucleus to reabsorb additional water and increase a tension of the disc tissue4,7,27). This mechanism hypothetically results in a more even distribution of weight across the intervertebral disc7,27).
There is no clear consensus regarding the most effective and safest laser or the ideal wavelength that should be used. Most lasers provide 1200 J of energy in a pulsatile fashion. High energy laser carries the risk of tissue burns, but low energy lasers may be insufficient to induce adequate vaporization. Lasers near the infrared region currently used in PLDD include neodymium : yttrium-aluminum-garnet laser (Nd : YAG), holmium : yttrium-aluminum-garnet laser (Ho : YAG), and diode laser. Lasers with visible green radiation include double-frequency Nd : YAG laser and potassium-titanyl-phosphate laser. Most lasers use a 3 mm outer cannula combined with a fiberoptic viewing cable29). PLDD uses directional laser beam energy that can be accumulated and penetrate anterior structure of disc which can cause injury of anterior longitudinal ligament, bowels, nerve roots, and end-plates, but cannot provide sufficient energy to disc itself.
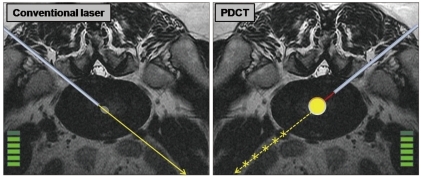
PDCT was designed to correct and improve this directional property of laser in 2006. It uses plasma laser. The major difference of the plasma light from conventional laser is that the rays generated in the module are concentrated at the end of the fiber and do not travel linearly forward (Fig. 5). According to our experimental study for the temperature measurement inside the disc using 8-channel automatic temperature meter, the tissues 3 mm away from the fiber tip which radiates plasma light whose directionality was 5% or less remained at the temperature not higher than 40℃. Therefore, a 6 mm diameter fire-sphere is created around fiber tip which means coagulation area or lesioning area (Fig. 1). The plasma light without directionality creates fire-sphere and provides sufficient effect with the least output power because all the energy is concentrated at the tip of the fiber. Even though energy output is excessive, the surrounding tissues including nerve root are safe. Three lesions which are made by fire-sphere are communicated each other and the sufficient decompression of intradiscal volume can be achieved. Chen et al.6) reported that the change in intradiscal pressure after nucleoplasty was negligible in older and degenerative discs, whereas intradiscal pressure was markedly reduced in younger and healthy discs in a cadaver study.
For avoiding the thermal damage of end plate, preservation of disc height and water content of nucleus pulposus may be very important factor in PDCT because it was easy to position the fiber tip in the middle of disc space in patients with well-maintained height of disc. In order to check these two factors, we have used Pfirrmann's grading system. We selected the patients with grade 3 and grade 4 disc degeneration. HLD with Pfirrmann's grade 1 and grade 2 disc degeneration is rare. Pfirrmann's grade 5 is not feasible for PDCT.
Success rates of previous PLDD using conventional laser have been reported vary from 56% to 87% and complications including procedure-related intraoperative neural injury have been described from 2.6% to 8%30). Sporadic cases of thermal injury to the cauda equina, disc herniation, and osteonecrosis of the vertebral endplates following IDET and nucleoplasty have been reported1,12,21). Transient nerve injury appears to be the most common complication after these procedures. In this study, there was one case of spondylodiscitis related to PDCT during the follow-up period. Spondylodiscitis is a well-recognized complication of diagnostic discography, with an overall incidence of 1% to 4%23). Complication rate of PDCT may be similar to that of discogram.
The results of this study indicate that PDCT is a safe and effective percutaneous treatment for the HLD patients with symptomatic radiculopathy between unsuccessful conservative therapy and other operative methods. In addition, PDCT is useful for the selective patient with mild to moderate disc degeneration. Further studies on PDCT in comparison with other previously known procedures are needed. Strict control of inclusion criteria could prevent misuse of PDCT and bring about long-term successful results.
References
1. Bhagia SM, Slipman CW, Nirschl M, Isaac Z, El-Abd O, Sharps LS, et al. Side effects and complications after percutaneous disc decompression using coblation technology. Am J Phys Med Rehabil. 2006; 85:6–13. PMID: 16357543.

2. Bonaldi G. Automated percutaneous lumbar discectomy : technique, indications and clinical follow-up in over 1000 patients. Neuroradiology. 2003; 45:735–743. PMID: 13680028.

3. Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009; 12:233–251. PMID: 19165306.
4. Castro WH, Halm H, Jerosch J, Schilgen M, Winkelmann W. [Changes in the lumbar intervertebral disk following use of the Holmium-Yag laser--a biomechanical study]. Z Orthop Ihre Grenzgeb. 1993; 131:610–614. PMID: 8310755.
5. Cesaroni A, Nardi PV. Plasma disc decompression for contained cervical disc herniation : a randomized, controlled trial. Eur Spine J. 2010; 19:477–486. PMID: 19902277.

6. Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine (Phila Pa 1976). 2003; 28:661–665. PMID: 12671352.

7. Choi JY, Tanenbaum BS, Milner TE, Dao XV, Nelson JS, Sobol EN, et al. Theramal, mechanical, optical, and morphologic changes in bovine nucleus pulposus induced by Nd:YAG (lambda=132 microm) laser irradiation. Lasers Surg Med. 2001; 28:248–254. PMID: 11295760.

8. Choy DS. Percutaneous laser disc decompression (PLDD) : twelve years' experience with 752 procedures in 518 patients. J Clin Laser Med Surg. 1998; 16:325–331. PMID: 10204439.

9. Choy DS, Case RB, Fielding W, Hughes J, Liebler W, Ascher P. Percutaneous laser nucleolysis of lumbar disks. N Engl J Med. 1987; 317:771–772. PMID: 3627193.

10. Choy DS, Diwan S. In vitro and in vivo fall of intradiscal pressure with laser disc decompression. J Clin Laser Med Surg. 1992; 10:435–437. PMID: 10148211.

11. Choy DS, Michelsen J, Getrajdman G, Diwan S. Percutaneous laser disc decompression : an update--Spring 1992. J Clin Laser Med Surg. 1992; 10:177–184. PMID: 10147861.
12. Cohen SP, Larkin T, Abdi S, Chang A, Stojanovic M. Risk factors for failure and complications of intradiscal electrothermal therapy : a pilot study. Spine (Phila Pa 1976). 2003; 28:1142–1147. PMID: 12782982.

13. German JW, Adamo MA, Hoppenot RG, Blossom JH, Nagle HA. Perioperative results following lumbar discectomy : comparison of minimally invasive discectomy and standard microdiscectomy. Neurosurg Focus. 2008; 25:E20. PMID: 18673050.
14. Gerszten PC, Smuck M, Rathmell JP, Simopoulos TT, Bhagia SM, Mocek CK, et al. Plasma disc decompression compared with fluoroscopy-guided transforaminal epidural steroid injections for symptomatic contained lumbar disc herniation : a prospective, randomized, controlled trial. J Neurosurg Spine. 2010; 12:357–371. PMID: 20201654.

15. Hopp E, Tsou PM. Postdecompression lumbar instability. Clin Orthop Relat Res. 1988; 227:143–151. PMID: 2962798.

16. Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc : a systematic review. Eur Spine J. 2011; 20:513–522. PMID: 20949289.

17. Javid MJ, Nordby EJ, Ford LT, Hejna WJ, Whisler WW, Burton C, et al. Safety and efficacy of chymopapain (Chymodiactin) in herniated nucleus pulposus with sciatica. Results of a randomized, double-blind study. JAMA. 1983; 249:2489–2494. PMID: 6341632.

18. Kahanovitz N, Viola K, Muculloch J. Limited surgical discectomy and microdiscectomy. A clinical comparison. Spine (Phila Pa 1976). 1989; 14:79–81. PMID: 2913673.
19. Lee SJ, Oh SH, Lee KS, Yi HJ, Bak KH, Kim JM. Nucleoplasty as an alternative intradiscal therapy in patients with lumbar disc herniation. J Korean Neurosurg Soc. 2003; 33:388–392.
20. Li J, Yan DL, Zhang ZH. Percutaneous cervical nucleoplasty in the treatment of cervical disc herniation. Eur Spine J. 2008; 17:1664–1669. PMID: 18830638.

21. Manchikanti L, Derby R, Benyamin RM, Helm S, Hirsch JA. A systematic review of mechanical lumbar disc decompression with nucleoplasty. Pain Physician. 2009; 12:561–572. PMID: 19461823.
22. Nordby EJ, Wright PH, Schofield SR. Safety of chemonucleolysis. Adverse effects reported in the United States, 1982-1991. Clin Orthop Relat Res. 1993; 122–134. PMID: 8339472.

23. Osti OL, Fraser RD, Vernon-Roberts B. Discitis after discography. The role of prophylactic antibiotics. J Bone Joint Surg Br. 1990; 72:271–274. PMID: 2312567.

24. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–1878. PMID: 11568697.

25. Ramirez LF, Thisted R. Using a national health care data base to determine surgical complications in community hospitals : lumbar discectomy as an example. Neurosurgery. 1989; 25:218–225. PMID: 2770986.

26. Rosen C, Rothman S, Zigler J, Capen D. Lumbar facet fracture as a possible source of pain after lumbar laminectomy. Spine (Phila Pa 1976). 1991; 16:S234–S238. PMID: 1862418.

27. Schenk B, Brouwer PA, van Buchem MA. Experimental basis of percutaneous laser disc decompression (PLDD) : a review of literature. Lasers Med Sci. 2006; 21:245–249. PMID: 16937074.

28. Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for lumbar facet pain. Spine (Phila Pa 1976). 2004; 29:2471–2473. PMID: 15507813.

29. Singh V, Derby R. Percutaneous lumbar disc decompression. Pain Physician. 2006; 9:139–146. PMID: 16703975.
30. Singh V, Manchikanti L, Benyamin RM, Helm S, Hirsch JA. Percutaneous lumbar laser disc decompression : a systematic review of current evidence. Pain Physician. 2009; 12:573–588. PMID: 19461824.
31. Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine (Phila Pa 1976). 1982; 7:604–607. PMID: 7167834.
32. Tassi GP. Comparison of results of 500 microdiscectomies and 500 percutaneous laser disc decompression procedures for lumbar disc herniation. Photomed Laser Surg. 2006; 24:694–697. PMID: 17199468.

Fig. 1
The first lesion (a) was made transitional area between annulus fibrosus and nucleus pulposus which was just beneath the herniated disc portion. The second lesion (b) was made at the center of intervertebral disc. The third lesion (c) was made between (a) and (b). Three lesions which are made by fireball are communicated each other and the sufficient decompression of intradiscal volume can be achieved.

Fig. 2
Mean VAS score was improved from 7.43 to 2.37 immediately after the procedure and well maintained until final follow-up. VAS : Visual Analog Scales, PDCT : percutaneous plasma disc oagulation therapy.

Fig. 3
Forty-one patients (89.1%) showed excellent and good clinical result in modified MacNab's criteria right after the procedure and well maintained until final follow-up.
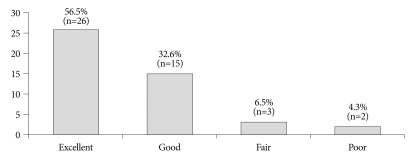
Fig. 4
A female patient (24 years old) who had great improvement right after PDCT. She took post-PDCT MRI one month later which showed improved disc herniation at the corresponding level. PDCT : percutaneous plasma disc oagulation therapy, MRI : magnetic resonance image.

Fig. 5
Comparison between conventional laser and PDCT. Conventional laser uses directional laser beam energy that can be accumulated and penetrated to anterior structure of disc which can cause injury of anterior longitudinal ligament, bowels, nerve root, and end-plate. Conventional laster cannot provide sufficient energy to disc itself. PDCT uses plasma laser. The major difference of the plasma light from conventional laser is that the rays generated in the module are concentrated at the end of the fiber and do not travel linearly. The plasma light without directionality creates fireball and provides sufficient effect with the least output power because all the energy is concentrated at the tip of the fiber. PDCT : percutaneous plasma disc oagulation therapy.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download