Abstract
Two cases of the posterior fossa dissecting aneurysm associated with a double origin of the posterior inferior cerebellar artery (DOPICA) causing subarachnoid hemorrhage are presented. After observing a relationship between the aneurysm and DOPICA on a three dimensional rotational angiogram (3DRA), the dissecting aneurysms were successfully obliterated by surgical trapping and endovascular internal trapping, respectively. This report warrants suspecting DOPICA of an associating anomaly predisposing to dissecting aneurysm in the vertebral artery-posterior inferior cerebellar artery territory and highlights the role of 3DRA in pretreatment evaluation of unusual aneurysms accompanying a particular anatomical variation.
The aberrant origin of the posterior inferior cerebellar artery (PICA) has been described elsewhere, with a focus on its extracranial origin and the increased frequency of accompanying cerebral aneurysms3,4,11). A rare variant of aberrant origin, a double origin of the posterior inferior cerebellar artery (DOPICA), has been scarcely reported in the literature5,7,10). A retrospective study reported that the incidence of DOPICA is 1.45%8). Although it is uncertain whether DOPICA is a rare disease entity or simply an underestimated angiographic finding, some authors have suggested that patients with a DOPICA are at an increased risk for intracranial aneurysms and that DOPICA may represent a risk factor for subsequent aneurysm development10). We report two patients with ruptured dissecting aneurysm related to a DOPICA, with a special emphasis on the treatment based upon their angioarchitectures.
This 56-year-old woman presented with spontaneous subarachnoid hemorrhage (SAH) detected on a CT scan. Cerebral angiography showed an irregularly shaped aneurysm (Fig. 1A, B), strongly suspicious of dissecting origin, in the distal segment of the left PICA. The origin of the left PICA was extracranial and low-lying at the atlantooccipital space. A right vertebral injection (Fig. 1C) also showed contrast filling in the left PICA aneurysm through the vertebrobasilar junction and a small branch arising from the most distal part of the left V4 segment suspecting a DOPICA. Reconstructed three dimensional rotational angiogram (3DRA) clearly demonstrated a fusiform aneurysm, locating after the convergence of two channels of DOPICA, on the distal PICA (Fig. 1D). Surgical treatment involved trapping of the dissecting aneurysm in the distal PICA. During the operation, the diseased artery was pinkish-gray in color and relatively hard in consistency (Fig. 1E). After confirming that there was no perforating vessel in the dissected segment, trapping of the dissected PICA was performed. After the operation, the patient awoke well from anesthesia without symptoms related to the PICA occlusion. Control left VA angiogram performed 3 weeks later showed well-obliterated PICA aneurysm. The distal flow in the left PICA was sustained with collateral circulations via the anterior inferior cerebellar artery on that side and the opposite PICA, but it appeared somewhat slow on right VA angiogram (Fig. 1F).
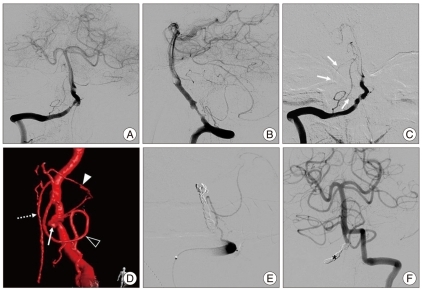
A 42-year-old man was transferred from an outside neurological service after lumbar tapping revealed bloody cerebrospinal fluid. Computed tomography (CT) scan revealed focal hemorrhage in front of the brainstem. A cerebral angiography (Fig. 2A, B) was performed and showed an irregular constriction and outpouching of the right vertebral artery (VA), which was strongly suggestive of a dissection. The origin of the right PICA was also extracranial and low-lying in the atlantooccipital space, and a small aneurysm was seen. Follow-up angiography (Fig. 2C) performed 3 days later showed the evolution of the dissection and enlargement of the aneurysmal dilatations. Reconstructed 3DRA clearly showed a smaller dissecting aneurysm near the vertebro-basilar junction and another larger aneurysm locating on the V4 from which a small branch was arising and converging into the very distal portion of the right PICA suspecting DOPICA (Fig. 2D). Endovascular treatment was chosen for internal trapping of the dissecting VA harboring aneurysms. A total of eight detachable coils were inserted in order to obliterate the dissecting VA harboring two aneurysms (Fig. 2E, F). The patient awoke promptly after the intervention without neurological deficit. The postoperative CT scan was normal, and the patient was discharged 5 days later. He was doing well at the 6-month follow-up.
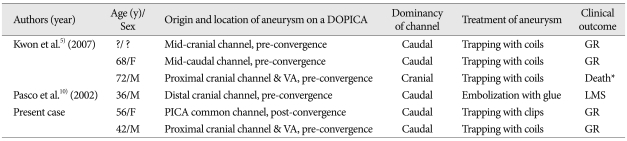
DOPICA is an anomaly in which two channels arise from the same VA and subsequently converge to constitute the distal PICA8). DOPICA depicts an embryologic remnant between the lateral spinal artery and the PICA6). The lateral spinal artery arises from either the PICA or the intradural VA and forms the caudal component of a DOPICA. The rostral component is embryologically derived from a hypertrophied radiculospinal artery8). Certain congenital anomalies may predispose an individual to aneurysmal formation. Although only a small number of DOPICA cases have been reported, a possible association between DOPICA and subsequent aneurysm formation has been suggested7,8,10). Usually, in the presence of DOPICA, the caudal root has a low origin without the regular anterior and lateral medullary segment but with a long ascending segment5,7,11). The cranial channel has most of the medullary perforators10). Distal PICA aneurysms are quite phenomenal2,9), and they are frequently of the dissecting type. Only four cases of the PICA dissecting aneurysms on a DOPICA with SAH have been described in the literature (Table 1)5,10). Two of the three cases reported by Kwon et al.5) showed a dissecting aneurysm in the cranial channel and the remaining case had an aneurysm in the caudal channel. Two patients who underwent endovascular trapping of one channel harboring an aneurysm showed good recovery after the intervention. Pasco et al.10) reported a patient with a distal PICA aneurysm who was treated with glue embolization of the cranial channel. However, a lateral medullary infarction followed, probably due to the occlusion of perforators from the cranial root. Supposing that the cranial channel gives rise to most of the medullary perforators, internal trapping of the cranial root should be done with caution. Surgical approaches to the dissecting aneurysms in the posterior fossa are relatively difficult, but surgery has the advantages of enabling visualization and confirmation of the perforators and preserving them as much as possible when trapping a dissected vessel1). Precise clip application just for the diseased vessel to preserve any critical perforator can maintain their function as the source of vital flow to the brainstem. One of our patients (Case 1) had a dissecting aneurysm after the convergence of a DOPICA, and the hemispheric branch of the PICA after the convergence was involved in and arose from the dissection. During the operation, no perforator in the dissected segment was confirmed, and clip application in both edges of the dissecting aneurysm was performed. A distal bypass was not carried out because the PICA usually carries adequate collateral flow from other cerebellar arteries. The other patient (Case 2) had two aneurysmal dilations associated with the right VA dissection on conventional angiogram. Follow-up 3DRA revealed that the lesion had become larger in size and the proximal aneurysm was located at the origin of the small cranial channel of the DOPICA. Internal occlusion of the dissected VA including two aneurysms and the proximal portion of the cranial channel of DOPICA underwent and this occlusion did not cause a worsening of the patient's neurological deficits, owing to the presence of the DOPICA as an alternative flow pathway and the right VA was not dominant.
DOPICA is rare anomaly and may represent a risk factor for subsequent aneurysm development and rupture. The key step to successful recognizing DOPICA in patients presenting with the VA-PICA dissecting aneurysm at an unusual location is a high index of suspicion, especially when extracranial origin of the PICA is accompanied. The images reconstructed by 3DRA not only provide more detailed information for evaluation of the relevant anatomy, but are also very helpful for planning of surgery or endovascular treatment.
References
1. Ali MJ, Bendok BR, Tawk RG, Getch CC, Batjer HH. Trapping and revascularization for a dissecting aneurysm of the proximal posteroinferior cerebellar artery : technical case report and review of the literature. Neurosurgery. 2002; 51:258–262. discussion 262-263. PMID: 12182429.
2. Arai K, Endo S, Hirashima Y, Takaku A. Posterior inferior cerebellar artery aneurysm associated with fenestration of the vertebral artery--case report. Neuro Med Chir (Tokyo). 1989; 29:29–31.

3. Ashley WW Jr, Chicoine MR. Subarachnoid hemorrhage caused by posterior inferior cerebellar artery aneurysm with an anomalous course of the atlantoaxial segment of the vertebral artery. Case report and review of literature. J Neurosurg. 2005; 103:356–360. PMID: 16175868.

4. Fine AD, Cardoso A, Rhoton AL Jr. Microsurgical anatomy of the extracranial-extradural origin of the posterior inferior cerebellar artery. J Neurosurg. 1999; 91:645–652. PMID: 10507387.

5. Kwon BJ, Jung C, Im SH, Lee DH, Han MH. Double origin of the posteroinferior cerebellar artery : angiographic anatomy and endovascular treatment of concurrent vertebrobasilar dissection. Neurosurgery. 2007; 61:242–247. discussion 247-248. PMID: 18091238.
6. Lasjaunias P, Vallee B, Person H, Ter Brugge K, Chiu M. The lateral spinal artery of the upper cervical spinal cord. Anatomy, normal variations, and angiographic aspects. J Neurosurg. 1985; 63:235–241. PMID: 4020445.
7. Lesley WS, Dalsania HJ. Double origin of the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2004; 25:425–427. PMID: 15037467.
8. Lesley WS, Rajab MH, Case RS. Double origin of the posterior inferior cerebellar artery : association with intracranial aneurysm on catheter angiography. AJR Am J Roentgenol. 2007; 189:893–897. PMID: 17885063.

9. Nishizaki T, Tamaki N, Nishida Y, Fujita K, Matsumoto S. Aneurysms of the distal posterior inferior cerebellar artery : experience with three cases and review of the literature. Neurosurgery. 1985; 16:829–832. PMID: 4010907.

10. Pasco A, Thouveny F, Papon X, Tanguy JY, Mercier P, Caron-Poitreau C, et al. Ruptured aneurysm on a double origin of the posterior inferior cerebellar artery : a pathological entity in an anatomical variation. Report of two cases and review of the literature. J Neurosurg. 2002; 96:127–131. PMID: 11794593.

11. Tabatabai SA, Zadeh MZ, Meybodi AT, Hashemi M. Extracranial aneurysm of the posterior inferior cerebellar artery with an aberrant origination : case report. Neurosurgery. 2007; 61:E1097–E1098. discussion E1098. PMID: 18091258.
Fig. 1
Case 1. Anteroposterior (AP) view of left vertebral artery (VA) angiogram (A) showing a peripheral aneurysm (arrow head) located on the hemispheric branch of the posterior inferior cerebellar artery (PICA) which has a low origin on the V4 (double arrowhead). Lateral view of left VA angiogram (B) demonstrating that a small cranial branch (arrow) originating from the distal V4 is directly anastomosed with the PICA. AP view of right VA angiogram (C) showing contrast filling of the aneurysm (arrowhead) through a small branch (arrow) originating on the distal V4. Reconstructed 3-dimensional rotational angiogram (D) clearly demonstrating the upper (arrows) and lower (double arrowheads) channel of double origin of the PICA and an associating aneurysm (arrowhead). Intraoperative photograph (E) showing trapping of the distal PICA (double arrowheads) harboring aneurysm (arrowhead). Follow-up right VA angiogram obtained 3 weeks after surgical trapping (F) showing a patent flow in the hemispheric branch of the left PICA (broken arrows) by collaterals and complete exclusion of the dissecting aneurysm.
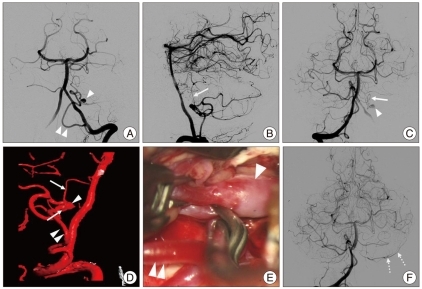
Fig. 2
Case 2. Right vertebral artery (VA) angiogram (A and B) obtained at admission showing an irregular constriction and outpouching of the right VA and revealing an extracranial origin PICA. Follow-up right VA angiogram obtained 3 days after admission (C) showing growing of aneurismal dilations from which a faint vessel arises (arrows). Enlarged, oblique view, 3DRA of the right VA (D) demonstrating that a small upper branch (arrowhead) originating from the proximal aneurysm (arrow) is directly anastomosed with the PICA (open arrowhead). The anterior spinal artery (broken arrow) originating on the V4 is located just distal to the dissection. Postoperative, lateral view of right VA angiogram (E) and AP view of left VA angiogram (F) showing total occlusion of the right VA in which are detachable coils (asterisk). PICA : posterior inferior cerebellar artery, 3DRA : three dimensional rotational angiogram, AP : anteroposterior.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download