Abstract
Methods
The records of neonates with meningomyelocele were retrospectively analyzed. Demographic and clinical characteristics as well as information, timing of surgery, and durations of hospital stay and antibiotic therapy were recorded.
Results
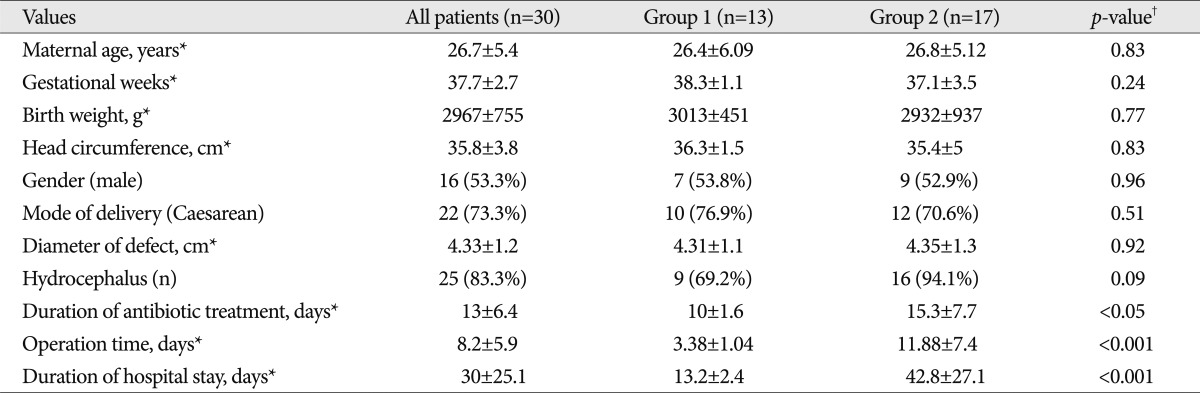
The records of 30 babies were included in the final analysis. Overall, the mean gestational age was 37.7±2.7 weeks, with a mean birth weight of 2967±755 g and head circumference of 35.8±3.8 cm. In terms of localization, 46.6% of the meningomyeloceles were lumbosacral, 40% were lumbar, 10% were thoracolumbar and 3.3% were thoracal. The mean size of the meningomyelocele sacs was 4.33±1.2 cm. Newborns underwent surgery on average of 8.2±5.9 days after birth, with an overall mean duration of hospital stay of 30±25.1 days. Patients were divided into two groups based on timing of surgery (group 1, ≤5 days; group 2, >5 days), and comparisons between groups revealed that earlier surgery was associated with significantly shorter durations of hospital stay (p<0.001) and antibiotic therapy (p<0.05).
Meningomyelocele (MMC) occurs as a result of failure of the neural canal to close posteriorly by the 26th day of gestation12). It is a devastating congenital defect of the central nervous system with no known cure, characterized by protrusion of the meninges and spinal cord through open vertebral arches leading to paralysis. Varying degrees of mental retardation, bowel and bladder dysfunction as well as orthopedic disabilities also occur in association with this debilitating disorder10,18).
The etiological mechanisms behind neural tube defects (NTDs) have yet to be completely elucidated, although their frequency has been reported to show variation depending on race, ethnic origin, geographical location and socioeconomic status6). Folic acid deficiency is one of best-documented risk factors for the development of NTDs17). The incidence of NTDs is high in Turkey, affecting 3-9 newborns in every 1000 live births11,16). Although many studies have focused on prenatal measures to decrease the frequency of MMC, research aimed at preventing the severe morbidity associated with this disorder is limited. The aim of this study was to evaluate the demographic and clinical characteristics as well as the frequency of associated anomalies in our MMC patient population, while also attempting to establish the relationship between timing of surgery and duration of hospital stay.
This retrospective study was conducted at Zekai Tahir Burak Maternity Teaching Hospital, situated in Ankara, with the approval of the local ethics committee. The medical records of newborns diagnosed with MMC between January 2009 and May 2011 were systematically reviewed, and relevant data such as demographics, findings on physical examination, presence of MMC-associated anomalies, size of the MMC defect and its localization were recorded. For those who underwent surgery, the timing of surgery as well as the post-operative duration of hospital stay (patients without complication and did not need any treatment for addition anomalies are discharged), length of antibiotic course (vancomycin or cefotaxime for meningitis/ventriculitis and/or local infection) and morbidity were also recorded. Patients were stratified into two groups based on the timing of surgery. Those who underwent surgery within the first 5 days after birth were placed in group 1 while group 2 was comprised of those who were operated later than 5 days.
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS) for Microsoft Windows, version 15.0 (SPSS Inc., Chicago, IL, USA). Comparisons between groups were made using the chi-square test for categorical variables and the Student's t-test for numerical variables. Values were provided as either percentage or mean±standard deviation, were applicable. A p-value of <0.05 was considered indicative of statistical significance.
The complete medical records of 30 patients who were retrieved were deemed suitable for analysis, the demographic and clinical characteristics of whom are summarized in Table 1. None of the mothers of the subjects included in this study had used any form of folic acid supplementation either before or during their pregnancies. A diagnosis of MMC was made antenatally by ultrasonography in 18 patients (40%). Only 3 of the births (10%) were a result of a consanguineous marriage.
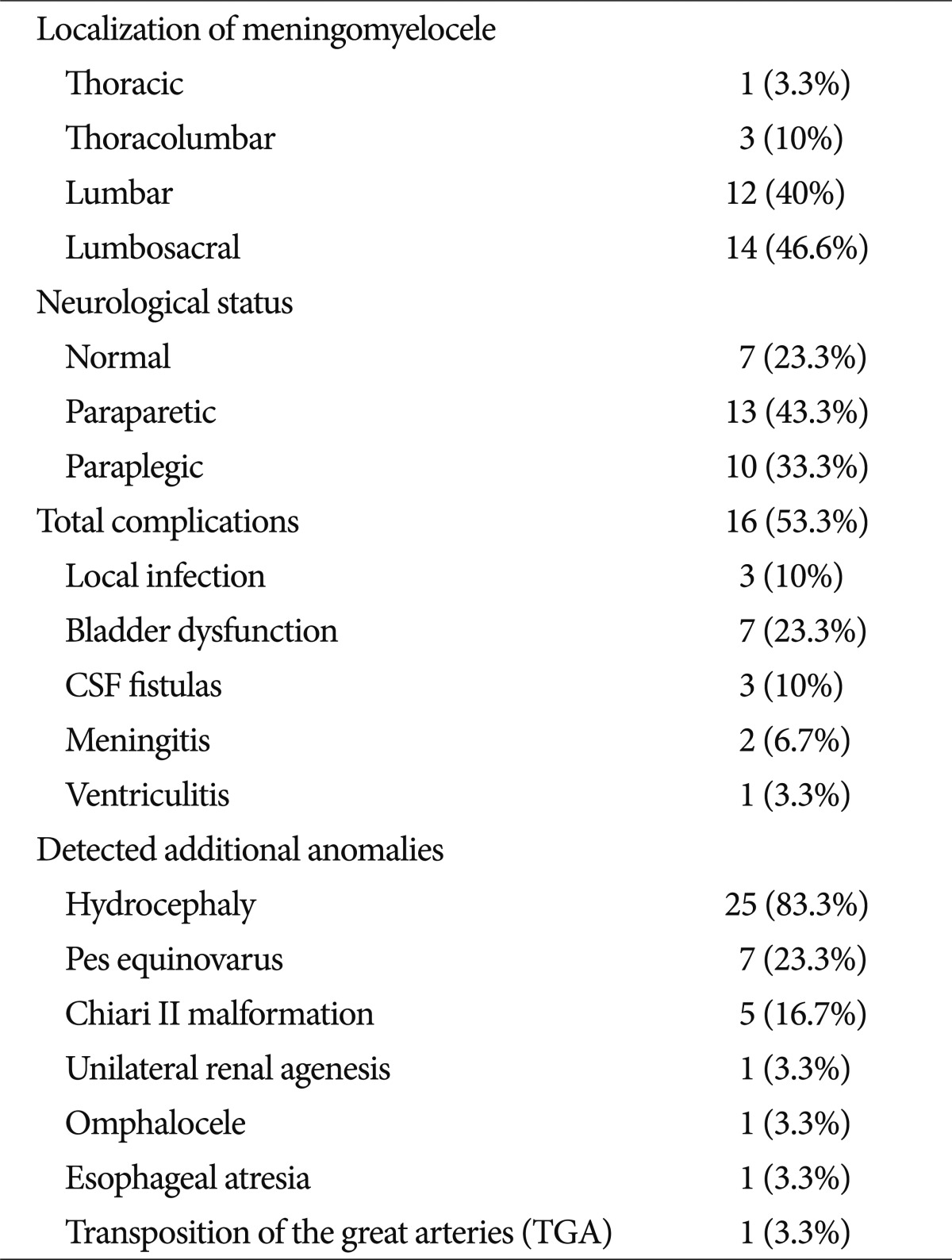
Localization of the MMC, neurological status, associated anomalies and complications are summarized in Table 2. The most frequently encountered localization was the lumbosacral area (46.6%), with 76.6% of patients having lower extremity neurological abnormality. Overall, MMC-related complications were observed in 16 patients (53.3%), the most common complication being bladder dysfunction. Hydrocephaly was the most commonly observed anomaly, occurring in 25 (83.3%) of our patients, followed by other anomalies (Table 2).
Cranial ultrasonography confirmed the presence of hydrocephaly in 25 (83.3%) patients. Overall, the mean lateral ventricle diameter was 20.2±4.8 mm, with no discernable difference between groups (p>0.05). All patients with hydrocephaly were subjected to scanning by cranial computerized tomography to confirm the diagnosis as well as to screen for the presence of other anomalies.
Comparisons between groups revealed that patients in group 1 who underwent surgery within 5 days of life had significantly lower durations of hospital stay and received shorter courses of antibiotics (p<0.001 for both) compared to patients in group 2 (Table 1).
All the newborns, except one, remained problem free related to surgery after discharge. Only one of the newborns who had transposition of the great arteries died while under follow-up in another center.
NTDs are the second most frequently encountered congenital malformations after cardiac anomalies. Due to recent advances in ultrasonography and its widespread use during antenatal follow-up, early in utero recognition of the disorder is now possible11,16). A diagnosis of MMC was made antenatally in 60% of our patients. Unfortunately, due to socio-cultural taboos regarding abortion, none of the families had consented to medical termination of pregnancy7).
Folic acid deficiency is the most widely recognized risk factor for the development of NTDs9). Preconceptional supplementation of folic acid at a daily dose of 0.4 mg has been reported to decrease NTDs rates by 60-70%17). This highlights the importance of antenatal folic acid supplementation for the prevention of NTDs. None of the mothers of the subjects included in this study had used any form of folic acid supplementation either before or during their pregnancies.
MMC most commonly occurs in the lumbar area, with a reported frequency of 60-70%8,12). In our study, lumbosacral MMC was observed in 46.6%, with a lumbar localization present in 40% of patients (Table 2). Hydrocephaly and the Chiari II malformation are the most frequently observed anomalies in association with MMC13). In our study population, hydrocephalus was present in 83.3% of patients, followed in decreasing order of other anomalies (Table 2). Taking this in to consideration, it is prudent that all patients with MMC should be screened for the presence of other anomalies that may be associated with the disorder, with the help of a careful physical examination, cranial imaging studies and urinary system ultrasonography5,8).
An early and aggressive surgical approach in babies diagnosed with MMC has been shown to be associated with lower early morbidity and mortality rates2,3).
In a retrospective study, early surgical intervention (<72 hours after birth) was found to be associated with a more favorable outcome in terms of urinary symptoms in patients with MMC, and investigators postulated that surgery within the first 24 hours increases the likelihood of maintaining urinary tract function15). In another study where the outcomes of prenatal (in utero) and postnatal surgery were compared, it was observed that prenatal intervention was associated with better motor development while also alleviating the need for shunt placement in most patients. However, authors stressed on the difficulty of the intrauterine procedure as well as the potential maternal and fetal risk posed by such surgery1,4). In a different study, corrective surgery was performed immediately after birth citing the added risk associated with in utero intervention for patients with MMC. Investigators reported on a low postoperative complication rate and less severe neurodevelopmental retardation with this approach14). With this study, we managed to demonstrate that patients operated upon within the first 5 days of life had significantly lower durations of hospital stay while also requiring shorter courses of antibiotics (p<0.001). In light of these findings, it is recommended to perform surgery as soon as possible, particularly in patients diagnosed prenatally.
MMC is a congenital disorder with significant morbidity. Our study findings suggest that early surgical intervention was associated with a shorter duration of hospital stay and antibiotic therapy as well as a lower complication rates. National policies for prevention, in utero diagnosis, and early surgical intervention are required for better prognosis.
References
1. Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011; 364:993–1004. PMID: 21306277.

2. Adzick NS, Walsh DS. Myelomeningocele : prenatal diagnosis, pathophysiology and management. Semin Pediatr Surg. 2003; 12:168–174. PMID: 12961110.
3. Bowman RM, McLone DG. Neurosurgical management of spina bifida: research issues. Dev Disabil Res Rev. 2010; 16:82–87. PMID: 20419775.

4. Bruner JP. Intrauterine surgery in myelomeningocele. Semin Fetal Neonatal Med. 2007; 12:471–476. PMID: 17716961.

5. Elliott SP, Villar R, Duncan B. Bacteriuria management and urological evaluation of patients with spina bifida and neurogenic bladder : a multicenter survey. J Urol. 2005; 173:217–220. PMID: 15592079.

6. Frey L, Hauser WA. Epidemiology of neural tube defects. Epilepsia. 2003; 44(Suppl 3):4–13. PMID: 12790881.

7. Koszutski T, Kawalski H, Kudela G, WrÓblewska J, Byrka-Owczarek K, Bohosiewicz J. Babies with myelomeningocele in Poland : parents' attitudes on fetal surgery versus termination of pregnancy. Childs Nerv Syst. 2009; 25:207–210. PMID: 18560842.

9. Medical Research Council Vitamin Research Study Group. Prevention of neural tube defects : results of the Medical Research Council Vitamin Study. Lancet. 1991; 338:131–137. PMID: 1677062.
10. Northrup H, Volcik KA. Spina bifida and other neural tube defects. Curr Probl Pediatr. 2000; 30:313–332. PMID: 11147289.

11. Onrat ST, Seyman H, Konuk M. Incidence of neural tube defects in Afyonkarahisar, Western Turkey. Genet Mol Res. 2009; 8:154–161. PMID: 19283682.

12. Padmanabhan R. Etiology, pathogenesis and prevention of neural tube defects. Congenit Anom (Kyoto). 2006; 46:55–67. PMID: 16732763.

13. Pinar H, Tatevosyants N, Singer DB. Central nervous system malformations in a perinatal/neonatal autopsy series. Pediatr Dev Pathol. 1998; 1:42–48. PMID: 10463270.

14. Pinto FC, Matushita H, Furlan AL, Alho EJ, Goldenberg DC, Bunduki V, et al. Surgical treatment of myelomeningocele carried out at 'time zero' immediately after birth. Pediatr Neurosurg. 2009; 45:114–118. PMID: 19307745.

15. Tarcan T, Onol FF, Ilker Y, Alpay H, Simşek F, Ozek M. The timing of primary neurosurgical repair significantly affects neurogenic bladder prognosis in children with myelomeningocele. J Urol. 2006; 176:1161–1165. PMID: 16890717.

16. Tunçbilek E, Boduroğlu K, Alikaşifoğlu M. Neural tube defects in Turkey : prevalence, distribution and risk factors. Turk J Pediatr. 1999; 41:299–305. PMID: 10770089.
17. Wald NJ. Folic acid and the prevention of neural-tube defects. N Engl J Med. 2004; 350:101–103. PMID: 14711907.

18. Werler MM, Mitchell AA. Neural-tube defects. N Engl J Med. 2000; 342:1135–1136. author reply 1136-1137. PMID: 10766583.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download