Abstract
Objective
Occipital neuralgia is characterized by paroxysmal jabbing pain in the dermatomes of the greater or lesser occipital nerves caused by irritation of these nerves. Although several therapies have been reported, they have only temporary therapeutic effects. We report the results of pulsed radiofrequency treatment of the occipital nerve, which was used to treat occipital neuralgia.
Methods
Patients were diagnosed with occipital neuralgia according to the International Classification of Headache Disorders classification criteria. We performed pulsed radiofrequency neuromodulation when patients presented with clinical findings suggestive occipital neuralgia with positive diagnostic block of the occipital nerves with local anesthetics. Patients were analyzed according to age, duration of symptoms, surgical results, complications and recurrence. Pain was measured every month after the procedure using the visual analog and total pain indexes.
Results
From 2010, ten patients were included in the study. The mean age was 52 years (34-70 years). The mean follow-up period was 7.5 months (6-10 months). Mean Visual Analog Scale and mean total pain index scores declined by 6.1 units and 192.1 units, respectively, during the follow-up period. No complications were reported.
Occipital neuralgia (ON) is a rare neurological disorder characterized by paroxysmal shooting or stabbing pain in the dermatomes of the greater occipital nerve (GON) or lesser occipital nerve (LON)5). Clinical presentation and a temporary improvement with local anesthetic diagnostic block of the GON or LON confirm the diagnosis5). The primary treatment of ON is conservative and focuses on reducing secondary muscle tension and improving posture. In cases of continual pain, nerve blocks may be applied or invasive procedures such as occipital nerve stimulation, neurolysis of the occipital nerves, or dorsal root entry zone rhizotomy may be performed20,21). However, the effects of nerve blocks are temporary, and surgical treatments are invasive and have risk and complications1,13,23). In this study, we present the clinical outcome of 10 patients with ON treated by pulsed radiofrequency (PRF).
From 2010, January to 2011, March, ten consecutive patients with ON were treated by PRF at our institute. All patients in this study were diagnosed with ON according to the International Classification of Headache Disorders classification criteria5). All patients presented with complaints of severe sharp stabbing pain in the occipital area. The duration of pain attacks varied from several minutes to several days, and the frequency varied from several times per month to several times per day. Palpation of the occipital area or upper neck on the affected side usually revealed muscle tenderness and in most cases precipitated pain attacks. All patients provided complete histories and underwent physical examinations followed by diagnostic tests such as computed tomography and magnetic resonance imaging. None of the patients responded to conservative management, including medications and physical therapy. All patients received GON and LON blocks with 1.0% lidocaine and dexamethasone twice by one week interval. Temporary pain relief of 50% or more was considered a positive response to the nerve blocks, and was one of the most important factors in patient selection for PRF, but the effects were temporary. These patients underwent PRF neuromodulation of the GON and LON for medically intractable ON (Fig. 1).
We performed fluoroscopically guided GON and LON PRF using a NeuroTherm NT1000 (NeuroTherm, Inc., Middleton, MA, USA) radiofrequency generator. In the operating room, each patient was placed in a sitting position on the procedure table and the posterior neck area was prepped with betadine and aseptically draped with sterile towels. The skin was anesthetized with 5% lidocaine gel. A disposable 22-gauge, 5 cm radiofrequency cannula (Model S-505, NeuroTherm, Inc., Middleton, MA, USA) with a 5 mm active tip was inserted at the levels of both the GON and LON (Fig. 2). The introducer needle was withdrawn and a disposable RF electrode (Model RFDE-5, NeuroTherm, Inc., Middleton, MA, USA) was advanced. Selective sensory nerve stimulation (50 Hz) showed concordant pain below 0.5 V, which confirmed localization of the PRF electrode. Motor nerve stimulation was then tested at 2 Hz to exclude the uncorrelated nerve. After stimulation, PRF was performed at 42℃ for a total of 240 pulses at each site.
In all patients, pain was measured before the primary diagnostic block and every month after PRF neuromodulation by the same blinded physician who had made the initial assessments. Pain was assessed using a Visual Analog Scale (VAS) (0 cm-no pain; 10 cm-worst possible pain imagined). Pain was also assessed using the Total Pain Index (TPI)3). The TPI is an incorporated pain scale of the weighted intensity and duration of headache attacks.
The age of the patients ranged between 34 to 70 years with a median age of 52 years. The patient sample consisted of seven (70%) women and three (30%) men. The mean total follow-up time of the patient series was 7.5 months, ranging from 6 to 10 months. The majority of patients presented with bilateral symptoms (60%, 6 of 10 patients) and the remaining four (40%) patients suffered from unilateral ON: two on the right and two on the left side.
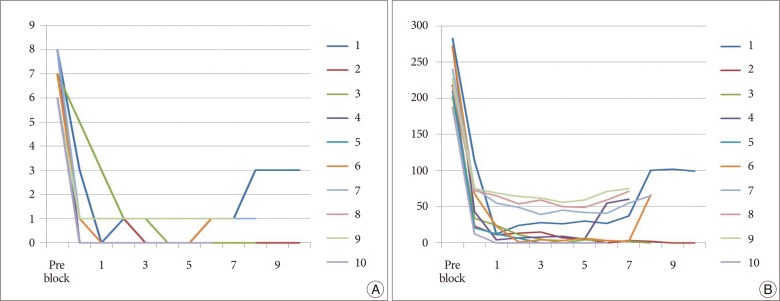
Mean VAS scores and mean TPI scores of the 10 treated patients are presented in Table 1. Significant improvements in pain (VAS, TPI) were found in months 1-6 compared with the pre-diagnostic block period (p<0.05) (Fig. 3). The mean VAS score before the pre-diagnostic block period was 6.9 and declined to 1.2 and 0.8 at post PRF and last follow-up period, respectively (p<0.001, and p<0.001). The mean TPI score before the pre-diagnostic block period was 232.7 and declined to 53.7 and 40.6 at post PRF and last follow-up period, respectively (p<0.001, and p<0.001) (Fig. 3).
Of the 10 patients, 8 (80%) completely stopped using analgesics following PRF treatment. One patient (10%) reported a substantial reduction in analgesic requirements and pharmacotherapy was maintained in one patient who had partial recurrence of headaches (Table 1).
There were neither intraoperative nor postoperative complications that would lead to any type of significant morbidity or mortality. No adverse effects of treatment were observed.
ON is a neuralgiform disorder defined as a shooting or stabbing pain originates in the suboccipital region and radiates over the vertex1). Hypo- or dysesthesia in the dermatome of the GON or LON, as well as tenderness to pressure over the course of the GON or LON can accompany the pain, and constant pain can persist between paroxysms. No data are available about the prevalence or incidence of ON. The most common cause of ON is irritation of the GON or LON. The GON is more frequently involved (90%) than the LON (10%). In 8.7% of patients, both GON and LON are responsible for ON4). Vision impairment/ocular pain (67%), tinnitus (33%), dizziness (50%), nausea (50%), and congested nose (17%) can be present because of connections to cranial nerves V, VIII, IX, X, and the cervical sympathetic ganglion7,15).
The most common treatment modality for ON is blockade of the GON and LON, which interrupts the pain cycle and reflex muscle spasms and relieves the symptoms. Many studies have shown that occipital nerve block is an effective treatment modality for ON. In a small (n=10) retrospective study by Kuhn et al.7), the GON was infiltrated with corticosteroids after a positive test block with bupivacaine. The authors observed pain relief of less than 1 week in 10% of patients, 1 week in 30%, 2 weeks in 30%, 1 month in 10%, and more than 2.5 months in 20% of patients. Hammond and Danta4) observed short-term effects (less than 1 week) in 64% of patients after 1 infiltration with local anesthetic; 36% of the patients reported effects lasting longer than 1 month. All of these effects were of short duration. Injection of depot methylprednisolone into the GON and LON regions produced complete headache relief for periods of only 10-77 days15).
When nerve block failto relief ON, cervical dorsal root ganglion PRF, and occipital nerve stimulation can be performed for medically intractable ON4,7,14,15,22). Weiner and Reed first reported 13 patients who underwent 17 occipital nerve stimulation procedures for medically intractable ON. With follow-ups ranging from 18 months to 6 years, good to excellent results were seen in 12 of 13 patients as defined by greater than 50% pain relief and requiring little or no pain medications. The 13th patient was explanted following resolution of symptoms22). Slavin et al.12,13) carried out trial stimulations in 14 patients with medically intractable ON. Definitive neurostimulators were implanted subcutaneously in 10 patients who had reductions in pain of greater than 50%. After a mean follow-up of 22 months, 70% of these patients still had good results. Other studies also report comparable results6,11). However, occipital nerve stimulation may be associated with possible complications such as infection, lead migration, hardware erosions, electrode fractures, disconnections, and sepsis13). When a prospective review explored the long-term effects of PRF treatment adjacent to the cervical dorsal root ganglion, the authors found that cervical dorsal root ganglion PRF also have serious complications occurred when a radiofrequency cannula was inserted at the level of the cervical dorsal root ganglion from posterior to frontal under the C-arm fluoroscopic guidance due to insertion into the cervical subarachnoid space or into vessels in this region. Potential risks include infection, stroke, paralysis and cerebrospinal fluid leakage23).
To date, one case report and one prospective trial have been published concerning PRF neuromodulation in ON10,16). In the case report, the patient showed 70% pain relief lasting 4 months. After recurrence of pain, the PRF neuromodulation procedure was repeated with again 70% pain relief lasting 5 months. Of the 19 patients included in the prospective trial, 68.4%, 57.9%, and 52.6% reported improvement of 50% or more 1, 2, and 6 months after PRF neuromodulation, respectively. There were significant improvements in the use of medication and in quality-of-life parameters.
Compared with the results of other treatment modalities, PRF shows higher efficacy without any complications18-21). PRF treatment is safer, and therefore, should be the preferred treatment for ON16). We used PRF for the GON and LON, and we observed pain relief for a minimum of 6 months. Meanwhile, none of the patients in our study have exhibited any side effects related to our procedure.
When performed PRF for ON, electrode approximation of the target nerve is very important. In our study, the puncture sites of the GON and LON were determined by external landmarks as described below2,8,9,17). On average, the GON is situated 3.8 cm lateral from the midline and one quarter of the distance along a line connecting the external occipital protuberance to the mastoid (or 2 cm lateral and 2 cm inferior to the external occipital protuberance). The authors used the relationship between the GON and the occipital artery for detecting the GON. At first, the authors identified the occipital artery pulsation about 2.5 cm from the midline, and the GON was located medial to the occipital artery. More detailed information regarding the puncture sites is provided in Fig. 2. The needle (22G) is introduced until there is bone contact or paresthesia is elicited. Subsequently, the needle is slightly withdrawn. Sensory and motor nerve stimulations are then performed and we can easily find the target nerves.
Several limitations of our study are worth mentioning. First, although the VAS and TPI are validated tools for the quantification of pain, they are subjective outcome measures because they are dependent on personal interpretations and variation. Second, the small sample size limits the power of our outcome observations.
The results of this retrospective clinical study support the hypothesis that PRF provides long-term reduction in headaches with minimal procedural risk in selected patients with medically intractable ON. PRF should be considered an effective treatment modality for ON, especially in medically intractable ON patients. Future long-term prospective controlled clinical trials are warranted to establish more definitive conclusions.
References
1. Afridi SK, Shields KG, Bhola R, Goadsby PJ. Greater occipital nerve injection in primary headache syndromes--prolonged effects from a single injection. Pain. 2006; 122:126–129. PMID: 16527404.

2. Becser N, Bovim G, Sjaastad O. Extracranial nerves in the posterior part of the head. Anatomic variations and their possible clinical significance. Spine (Phila Pa 1976). 1998; 23:1435–1441. PMID: 9670393.
3. Bovim G, Fredriksen TA, Stolt-Nielsen A, Sjaastad O. Neurolysis of the greater occipital nerve in cervicogenic headache. A follow up study. Headache. 1992; 32:175–179. PMID: 1582835.

4. Hammond SR, Danta G. Occipital neuralgia. Clin Exp Neurol. 1978; 15:258–270. PMID: 756019.
5. Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24(Suppl 1):9–160. PMID: 14979299.
6. Kapural L, Mekhail N, Hayek SM, Stanton-Hicks M, Malak O. Occipital nerve electrical stimulation via the midline approach and subcutaneous surgical leads for treatment of severe occipital neuralgia: a pilot study. Anesth Analg. 2005; 101:171–174. PMID: 15976227.

7. Kuhn WF, Kuhn SC, Gilberstadt H. Occipital neuralgias: clinical recognition of a complicated headache. A case series and literature review. J Orofac Pain. 1997; 11:158–165. PMID: 10332322.
8. Loukas M, El-Sedfy A, Tubbs RS, Louis RG Jr, Wartmann CH, Curry B, et al. Identification of greater occipital nerve landmarks for the treatment of occipital neuralgia. Folia Morphol (Warsz). 2006; 65:337–342. PMID: 17171613.
9. Natsis K, Baraliakos X, Appell HJ, Tsikaras P, Gigis I, Koebke J. The course of the greater occipital nerve in the suboccipital region: a proposal for setting landmarks for local anesthesia in patients with occipital neuralgia. Clin Anat. 2006; 19:332–336. PMID: 16258972.

10. Navani A, Mahajan G, Kreis P, Fishman SM. A case of pulsed radiofrequency lesioning for occipital neuralgia. Pain Med. 2006; 7:453–456. PMID: 17014606.

11. Nörenberg E, Winkelmüller W. [The epifacial electric stimulation of the occipital nerve in cases of therapy-resistant neuralgia of the occipital nerve]. Schmerz. 2001; 15:197–199. PMID: 11810356.
12. Slavin KV, Colpan ME, Munawar N, Wess C, Nersesyan H. Trigeminal and occipital peripheral nerve stimulation for craniofacial pain: a single-institution experience and review of the literature. Neurosurg Focus. 2006; 21:E5. PMID: 17341049.

13. Slavin KV, Nersesyan H, Wess C. Peripheral neurostimulation for treatment of intractable occipital neuralgia. Neurosurgery. 2006; 58:112–119. discussion 112-119. PMID: 16385335.

14. Van Zundert J, Lamé IE, de Louw A, Jansen J, Kessels F, Patijn J, et al. Percutaneous pulsed radiofrequency treatment of the cervical dorsal root ganglion in the treatment of chronic cervical pain syndromes: a clinical audit. Neuromodulation. 2003; 6:6–14. PMID: 22150908.

15. Vanelderen P, Lataster A, Levy R, Mekhail N, van Kleef M, Van Zundert J. 8. Occipital neuralgia. Pain Pract. 2010; 10:137–144. PMID: 20415731.
16. Vanelderen P, Rouwette T, De Vooght P, Puylaert M, Heylen R, Vissers K, et al. Pulsed radiofrequency for the treatment of occipital neuralgia: a prospective study with 6 months of follow-up. Reg Anesth Pain Med. 2010; 35:148–151. PMID: 20301822.
17. Vital JM, Grenier F, Dautheribes M, Baspeyre H, Lavignolle B, Sénégas J. An anatomic and dynamic study of the greater occipital nerve (n. of Arnold). Applications to the treatment of Arnold's neuralgia. Surg Radiol Anat. 1989; 11:205–210. PMID: 2588096.

18. Volcy M, Tepper SJ, Rapoport AM, Sheftell FD, Bigal ME. Botulinum toxin A for the treatment of greater occipital neuralgia and trigeminal neuralgia: a case report with pathophysiological considerations. Cephalalgia. 2006; 26:336–340. PMID: 16472343.

19. Wang H, Chen H, Jiang H. Experience in acupuncture treatment of occipital neuralgia. J Tradit Chin Med. 2002; 22:183. PMID: 12400421.
20. Wanke R, Bues E. [Operative therapy of severe occipital neuralgia]. Chirurg. 1953; 24:306–311. PMID: 13094777.
22. Weiner RL. Subcutaneous occipital region stimulation for intractable headache syndromes. Prog Neurol Surg. 2011; 24:77–85. PMID: 21422778.

23. Zhang J, Shi DS, Wang R. Pulsed radiofrequency of the second cervical ganglion (C2) for the treatment of cervicogenic headache. J Headache Pain. 2011; 12:569–571. PMID: 21611808.

Fig. 2
Anatomic landmarks for the needle insertion point of the greater occipital nerve and lesser occipital nerve. blue circle: external occipital protuberance, GON: greater occipital nerve, LON: lesser occipital nerve, OA: occipital artery.

Fig. 3
Graphs showing pain degree changes over a 6 month period according to various pain measurement: visual analogue scale (A), total pain index (B).




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download