Abstract
Iatrogenic vascular injuries during lumbar disc surgery may occur rarely but they are serious complications, which can be fatal without appropriate management. Prompt diagnosis and management of these complications are imperative to prevent a desperate outcome. A 72-year-old female with proximal left common iliac artery iatrogenic injury during lumbar discectomy was successfully treated by percutaneous deployment of a stent graft in an emergency setting. Postprocedural angiogram demonstrated complete exclusion of the iliac artery laceration. The patient became hemodynamically stable. Two weeks later she complained of vascular claudication. Follow-up angiography revealed decreased arterial flow in the opposite common iliac artery. An additional kissing stent was inserted into the right common iliac artery and the symptoms of vascular claudication disappeared. Endovascular stenting offers a safe and effective method for the treatment of an iatrogenic arterial laceration, particularly in a critical condition. But, the contralateral iliac arterial flow should be kept intact in case of proximal iliac artery injury. Otherwise, additional treatments may be needed.
Major vascular injury is a rare yet catastrophic complication of posterior lumbar disc surgery. Conventional surgical approaches for repairing injured vessels may be successful, but major procedures are required. Recently, some successful endovascular treatments for major vessel injury during or after posterior lumbar discectomy have been published1,4,5). We present a patient who sustained a proximal left common iliac artery injury during L4-5 discectomy. Although, an additional treatment was needed to resolve the delayed contralateral common iliac artery stenosis after the first procedure, the iatrogenic iliac artery laceration was successfully repaired by percutaneous endovascular stenting.
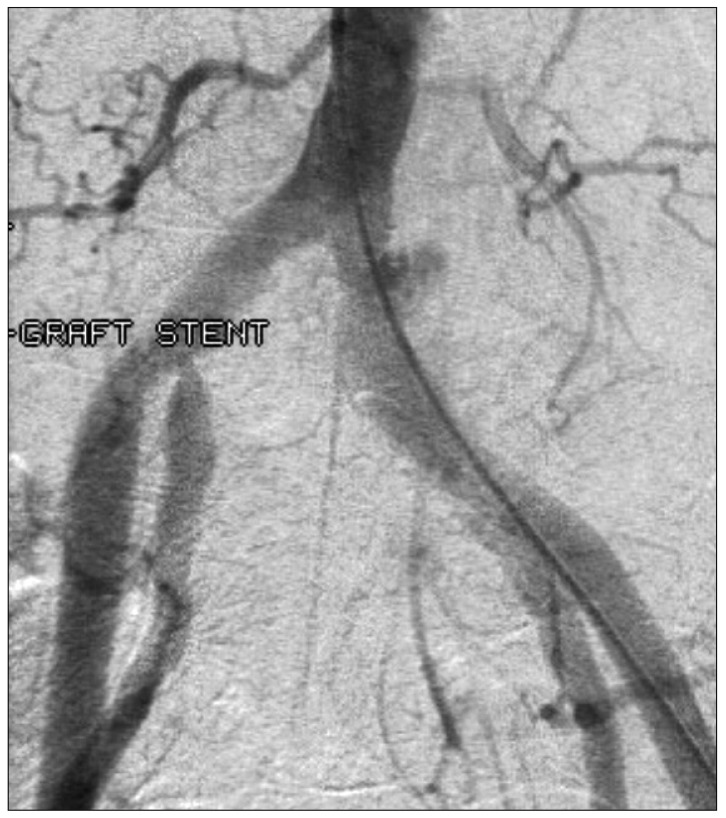
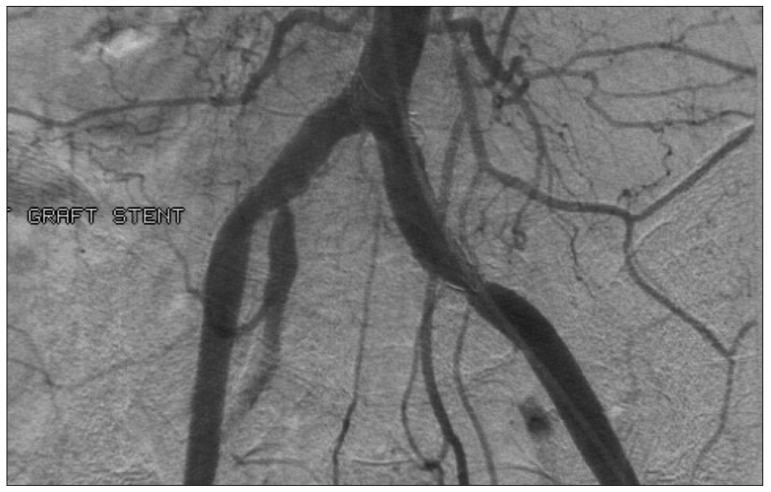
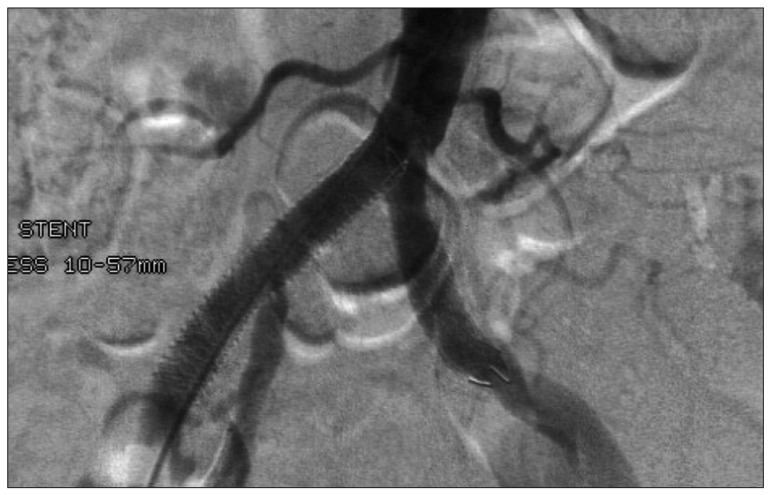
A 72-year-old female patient who had undergone lumbar discectomy at the L4-5 level one month ago, was admitted with same-level, recurrent disc herniation. The patient underwent removal of a left paracentral L4-L5 disc prolapse via microscopic posterior approach. Routine microdiscectomy was performed using pituitary rongeurs. As the discectomy was nearly completed, a sudden spurt of blood occurred immediately after the last rongeuring away the disc material. Tamponing using a combination of several Gelfoams® and surgical cottons seemed to stop the bleeding. But, a few minutes later, as soon as the combination of several Gelfoams® and surgical cottons was removed, profuse bleeding from the disc space occurred again. As the blood continued to gush out, blood pressure suddenly decreased from 110/80 mm Hg to 50/30 mm Hg. Multiple similar procedures were required to stop the leak, and the patient was consulted with general and vascular surgeons. Consultations suggested an injury to the iliac artery and hypovolemic shock. The operative wound was closed immediately. Meanwhile, the patient was ready for an emergency endovascular procedure. Diagnostic angiography confirmed a leak at the proximal left common iliac artery (Fig. 1). A Stent-Graft® (S & G Biotech, Seongnam, Korea) was inserted over a guide wire to seal the iliac laceration. Complete angiography demonstrated no leakage of contrast medium and patency of both the iliac arteries (Fig. 2). Because the iliac artery laceration was located just below the aortic bifurcation, it was required that the stent be placed proximally, and it eventually seemed to block some of the flow in the right iliac artery. The patient's vital signs were again stable after stent insertion. One week postoperatively, the patient complained of right buttock pain while walking. Angiography revealed a stenosis of the proximal right common iliac artery and decreased arterial flow (Fig. 3). An additional stent (Boston Scientific, Natick, MA, USA) was deployed to the proximal right common iliac artery in a kissing stent pattern. After that, the flow in the right common iliac artery was markedly improved (Fig. 4). The patient gradually recovered and eventually achieved a full recovery.
Iatrogenic major vascular injuries during posterior lumbar discectomy are a rare complication, but they can be life-threatening. Recent reviews estimated variable incidence ranging below 1%, but the exact incidence of vascular injury in lumbar discectomy is not known2,3,12).
Major vessels, which are in proximity to the vertebral column, are at risk of intraoperative injury because of their location. The injuries predominantly associated with upper lumbar surgery are those to the aorta and inferior vena cava. However, iliac vessel injuries are more common in lower lumbar surgery6,9).
Traditionally, vascular injury complicating lumbar discectomy was treated by direct surgical repair of the damaged vessels8). Although the current surgical outcomes are considered good, surgical repair of traumatic or postoperative vascular injury may result in considerable blood loss and more complications.
Endovascular technique is an alternative method of treating vascular injury following lumbar disc surgery. Endovascular techniques that introduce stent graft to exclude AVF or leakage following lumbar discectomy have shown an increase in technical success rates and reduction in complication rates1,5). The advantages of endovascular techniques in patients are the absence of a lower abdominal incision, minimal blood loss and a reduction in the depth and length of anesthesia, permitting shorter hospitalization compared with conventional surgery. However, proper facilities and an assortment of stent graft and other materials must be available1).
In our case, profuse bleeding occurred from the disc space at the end of operation. Fortunately, an angiographic evaluation and proper treatment of the iliac artery injury could be carried out in the emergency setting. The defect was apparently located on the proximal left common iliac artery. The intention was to seal the artery injury using a stent graft. But, another problem was the proximity between the injury site and aortic bifurcation. The possibility of luminal compromise of the contralateral common iliac due to the proximal end of the stent graft was a matter of concern. A careful employment of the stent graft at the proximal left common iliac artery was done, and not only complete sealing of the leakage but also good flow in the bilateral common iliac arteries were revealed.
Many authors advocate protection of the contralateral common iliac artery during stent placement in the proximal common iliac artery7,11,13). Spinosa et al.11) strongly recommended that, if a stent is placed at the origin of a common iliac artery, a stent should also be placed in the contralateral common iliac artery, even if it is normal. It is proposed that these "kissing stents" will prevent compromise of the contralateral iliac artery. On the other hand, Smith et al.10) reported that contralateral protection during stent placement in a proximal common iliac artery was not mandatory.
Although an immediate postoperative angiography demonstrated good flow in the bilateral common iliac arteries, delayed stenosis of the contralateral iliac artery occurred in our case. Thrombosis around the proximal end of the stent graft was assumed to be the cause of the delayed contralateral iliac artery stenosis.
References
1. Bierdrager E, Van Rooij WJ, Sluzewski M. Emergency stenting to control massive bleeding of injured iliac artery following lumbar disk surgery. Neuroradiology. 2004; 46:404–406. PMID: 15095028.

2. Erkut B, Unlü Y, Kaygin MA, Colak A, Erdem AF. Iatrogenic vascular injury during to lumbar disc surgery. Acta Neurochir (Wien). 2007; 149:511–515. discussion 516. PMID: 17387429.

3. Ewah B, Calder I. Intraoperative death during lumbar discectomy. Br J Anaesth. 1991; 66:721–723. PMID: 2064889.

4. McCarter DH, Johnstone RD, McInnes GC, Reid DB, Pollock JG, Reid AW. Iliac arteriovenous fistula following lumbar disc surgery treated by percutaneous endoluminal stent grafting. Br J Surg. 1996; 83:796–797. PMID: 8696743.

5. Nam TK, Park SW, Shim HJ, Hwang SN. Endovascular treatment for common iliac artery injury complicating lumbar disc surgery : limited usefulness of temporary balloon occlusion. J Korean Neurosurg Soc. 2009; 46:261–264. PMID: 19844629.

6. Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, Tsolakis JA. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002; 24:189–195. PMID: 12217278.

7. Rees CR, Palmaz JC, Garcia O, Roeren T, Richter GM, Gardiner G Jr, et al. Angioplasty and stenting of completely occluded iliac arteries. Radiology. 1989; 172:953–959. PMID: 2528170.

8. Salander JM, Youkey JR, Rich NM, Olson DW, Clagett GP. Vascular injury related to lumbar disk surgery. J Trauma. 1984; 24:628–631. PMID: 6748126.

9. Sande E, Myhre HO, Witsøe E, Lundbom J, Stolt-Nielsen A, Anda S. Vascular complications of lumbar disc surgery. Case report. Eur J Surg. 1991; 157:141–143. PMID: 1676309.
10. Smith JC, Watkins GE, Taylor FC, Carlson LA, Karst JG, Smith DC. Angioplasty or stent placement in the proximal common iliac artery : is protection of the contralateral side necessary? J Vasc Interv Radiol. 2001; 12:1395–1398. PMID: 11742012.

11. Spinosa DJ, Angle JF, Hagspiel KD, Pyle DA, Matsumoto AH. Iliac artery stenting : a review of devices and technical considerations. Appl Radiol. 1998; 27:10–24.
12. Szolar DH, Preidler KW, Steiner H, Riepl T, Flaschka G, Stiskal M, et al. Vascular complications in lumbar disk surgery : report of four cases. Neuroradiology. 1996; 38:521–525. PMID: 8880709.

13. Vorwerk D, Günther RW, Keulers P, Wendt G. Surgical and percutaneous management of contralateral thrombus dislodgement following stent placement and dilatation of iliac artery occlusions : technical note. Cardiovasc Intervent Radiol. 1991; 14:134–136. PMID: 1855238.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download