Abstract
The waffle-cone technique is a modified stent application technique, which involves protrusion of the distal portion of a stent into an aneurysm fundus to provide neck support for subsequent coiling. The authors report two cases of wide necked basilar bifurcation aneurysms, which were not amenable to stent assisted coiling, that were treated using the waffle-cone technique with a Solitaire AB stent. A 58-year-old woman presented with severe headache. Brain CT showed subarachnoid hemorrhage and angiography demonstrated a ruptured giant basilar bifurcation aneurysm with broad neck, which was treated with a Solitaire AB stent and coils using the waffle-cone technique. The second case involved an 81-year-old man, who presented with dizziness caused by brain stem infarction. Angiography also demonstrated a large basilar bifurcation unruptured aneurysm with broad neck. Solitaire AB stent deployment using the waffle-cone technique, followed by coiling resulted in near complete obliteration of aneurysm. The waffle-cone technique with a Solitaire AB stent can be a useful alternative to conventional stent application when it is difficult to catheterize bilateral posterior cerebral arteries in patients with a wide-necked basilar bifurcation aneurysm.
The endovascular treatment of wide-necked bifurcation aneurysms remains challenging despite of the recent advances in endovascular devices and techniques. Various techniques, such as the balloon remodeling technique, stent assisted coiling, the Y stent construct, and multiple microcatheter techniques have been developed to manage these challenging aneurysms1,2,9,15). However, in wide-necked basilar bifurcation aneurysms, it can be difficult to catheterize bilateral distal posterior cerebral artery (PCA) segments if the angles between PCAs and the basilar artery are acute. In such case, the balloon remodeling technique and the Y stent construct is not possible. On the other hand, waffle-cone technique, which involves the passage and deployment of a stent in the proximal neck of an aneurysm, can allow parent artery and major branch preservation. Furthermore, this technique has been described as a viable option in patients with a wide-necked aneurysm, otherwise not amenable to endovascular treatment13,14).
The authors report two cases of wide-necked basilar bifurcation aneurysms treated using the waffle-cone technique using a Solitaire AB stent (ev3 Inc., Irvine, CA, USA) that were resolved without any complication.
A 58-year-old woman presented with severe headache for 3 days. She was alert and had no focal neurological deficit. Physical examination showed severe neck stiffness (Hunt & Hess grade II). Brain CT showed subarachnoid hemorrhage on both Sylvian cisterns, anterior interhemispheric fissure, and right ambient cistern (Fisher grade III). A round, slightly hyperdense lesion was also seen on the suprasellar cistern. Computed tomography angiograms (CTA) demonstrated a giant basilar bifurcation aneurysm, which was considered ruptured, and an unruptured anterior communicating artery (AComA) aneurysm (Fig. 1A, B, C). Time of flight (TOF) magnetic resonance angiograms (MRA) clearly visualized the inflow zone of basilar bifurcation aneurysm from the orifice to the dome. However, the basal portion of the aneurysm was not definitely visualized because of stagnant-low flow (Fig. 1D, E).
Digital subtraction angiography (DSA) showed a 25×18×17 mm broad necked (12 mm) basilar bifurcation giant aneurysm. The orifices of both PCAs and superior cerebellar arteries (SCAs) were observed to be incorporated in the giant aneurysm by 3-dimensional rotational angiography. However, main flow to left PCA came from the left internal carotid artery through the posterior communicating artery, which suggested a lower likelihood of PCA infarction after coil embolization even if the left PCA origin was accidentally occluded (Fig. 2A, B, C). Accordingly, coil embolization was planned for both aneurysms.
Embolization procedures were performed under general endotracheal anesthesia. After bilateral femoral arterial puncture, the unruptured small AComA aneurysm was obliterated first with endovascular coils via a right femoral route, and then 6F and 5F Envoy guiding catheters (Cordis neurovascular, Miami, FL, USA) were placed in the left and right vertebral arteries (VAs), respectively via bilateral femoral arterial routes. Rebar-18 microcatheter (ev3 Inc., Irvine, CA, USA) was then navigated through the right side 5F guiding catheter and placed into the giant aneurysm lumen, and two microcatheters were navigated through the left side 6F guiding catheter for double catheter technique. An Echelon-10 microcatheter (ev3 Inc., Irvine, CA, USA) was then placed deeply into the aneurysmal sac near the neck portion beyond the dome, and a proximal marker was located inside the aneurysm. A Solitaire AB intracranial stent (4×20 mm) was advanced through the Rebar-18 catheter and deployed into the aneurysmal sac distally (initially 8 mm, finally redeployed at 5 mm), and in the distal basilar artery proximally in a 'waffle-cone' manner to protect the orifices of the right P1 and both SCAs. The flared distal stent tip was located above about 5 mm above the aneurysmal neck (Fig. 2D). The waffle-cone shaped stent served as a buttress for the coil frame to prevent compromise of the right PCA, and flow in both SCAs. After stent deployment, the Rebar-18 catheter was withdrawn to the right VA level to improve basilar artery flow. Another microcatheter of Prowler Select Plus (Cordis neurovascular, Miami, FL, USA) was then introduced and the aneurysm was selected through the Solitaire stent lumen. A stable coil frame was made using Axium 14 mm×40 cm and Axium 12 mm×40 cm coils through two different microcatheters. Packing with a total of 31 coils resulted in partial obliteration of the giant aneurysm, leaving a neck remnant (Fig. 2E-I). Activated coagulation time (ACT) monitoring was performed from the beginning on the procedure. A target ACT of between 250 and 300 seconds was maintained, and a 3000 unit of heparin was injected intravenously just prior to stent deployment followed by 1.000 unit per hour. Plavix (300 mg) was administered via an L-tube by an anesthesiologist after packing several coils. After coiling, 0.5 mg of Agrastat was infused through the microcatheter to prevent thromboembolic complications.
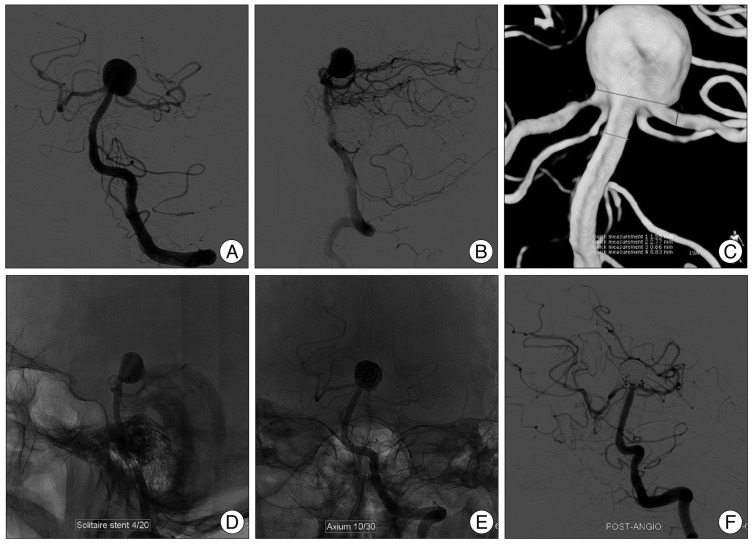
An 81-year-old man, who presented with dizziness due to a brain stem infarction was referred to our department. He was alert without focal neurological deficit. CTA showed a large unruptured basilar bifurcation aneurysm. DSA also demonstrated a large basilar bifurcation aneurysm (13×12×10 mm) with a 10 mm neck. Both P1 originated from the aneurysm (Fig. 3A, B, C). After 7 days of dual antiplatelet therapy, endovascular treatment using the waffle-cone technique was performed.
Under general endotracheal anesthesia, a 6F Envoy guiding catheter was placed on the left VA, and then a 4×20 mm Solitaire AB stent was deployed through a Rebar-18 microcatheter into the aneurysmal sac distally, and distal basilar artery proximally in a waffle-cone manner to protect the orifices of both P1s and to support the coil mass (Fig. 3D). Aneurysm selection was made through the stent lumen with a second microcatheter. Neck remnant of large basilar bifurcation aneurysm was achieved with 11 coils, with sparing of flow in both PCAs (Fig. 3E, F). Postoperatively, he was recovered well, and was discharged to home 4 days after the procedure.
Endovascular treatment of wide-necked large to giant bifurcation aneurysm is still challenging. Simple coiling is usually not possible, and various technical modifications have been developed and employed to treat this challenging lesions. These include the balloon remodeling technique, stent assisted coiling, the Y stent construction, and multiple microcatheter techniques3,5-7). However, if major arteries are incorporated with the aneurysmal fundus, and superselection of distal major vessels is not possible due to acute angles between the parent artery and distal vessels, it is not possible to place a stent across the aneurysmal neck. In this situation, the distal portion of a stent can be placed into the aneurysm sac beyond the neck to provide neck support for subsequent coiling. This intra-/extra-aneurysmal stent placement for the management of wide necked bifurcation aneurysms was first described by Horowitz et al. in 2006 as the "waffle-cone" technique because of the appearance of the stent-coil combination after intracratreatment8).
They reported successful obliteration of wide necked aneurysm in 8 patients using this technique. Since its introduction, 4 reports have been published using this technique4,10-12). The waffle-cone technique has been used to treat the bifurcation aneurysms, such as, basilar bifurcation, AComA, and middle cerebral artery bifurcation aneurysms. Initially, open cell design Neuroform stent were used for this purpose5-8,11), but recently, waffle-cone technique using a closed cell design stent has been described12). Sychra et al.14) reported their experiences of waffle-cone technique in 6 patients using the Solitaire AB stent.
Solitaire stents have the unique advantage that they have no distal platinum wire purchase, which might perforate aneurysm sacs during stent placement beyond their distal portions when the waffle-cone technique is used. The other advantage of the Solitaire stent over the Neuroform stent is that it has a closed cell design, and can be retrieved even after full deployment.
To accommodate the coils and to protect the P1 orifice, flaring of the distal end of the stent may be desirable when the waffle-cone technique is used. However, in our case distal flaring seemed minimal. To achieve more distal flaring during the waffle-cone technique, a 6 mm diameter Solitaire stent might be more suitable than the 4 mm stent if the neck diameter is more than 6 mm, as was the cases in our patients. In addition, to increase the safety and ease of the waffle-cone technique, a tapered stent with a flared end and without platinum wire purchase are desirable.
In our cases, stent-assisted coiling and Y stenting were considered initially, but angles between the PCA and distal basilar artery were too acute to catheterize the PCA, thus, we used the waffle-cone technique. In both cases, distal end of the stent was placed directly into the base of a bifurcation aneurysm and subsequent coiling was performed through the expanded and cone-shaped distal stent ends to preserve parent artery patency14). In case 1, a double microcatheter was used to insert coil because the aneurysm was very large and the main portion of the aneurysmal sac was located eccentrically with respect to its orifice. One microcatheter tip was located near the fundus beyond the dome before stent deployment. The other microcatheter was placed through the stent lumen after stent deployment. Coiling through the double microcatheter and waffle-cone stent support resulted in successful obliteration of the aneurysm without compromise of bilateral PCAs or SCAs.
This technique is also useful in cases of proximal and distal vessel diameter mismatch. If the distal vessel is too narrow to accommodate a stent, or if there is fear of distal vessel occlusion after conventional stent assisted coiling, the waffle-cone technique provides a better alternative than the conventional stent-assisted coiling technique.
Deploying a stent inside an aneurysm increases the risk of perforation. Sychra et al.14) suggested that the technique should only be used for aneurysms larger than 4 mm, because in large aneurysms, the stent can easily be placed into the aneurysm fundus and deployed avoiding the risks of periprocedural rupture. However, when a Solitaire stent is used, the risk of aneurysmal perforation is probably reduced because there is no distal platinum wire.
It is important to obliterate the inflow zone of an aneurysm to prevent coil compaction or recanalization. Thus, the identification of the inflow zone is an important aspect of the endovascular procedure. In our case 1, TOF MRA clearly visualized the inflow zone of the basilar bifurcation aneurysm from orifice to dome, but the basal portion was not clearly visualized because of the stagnant slow flow. Turbulent flow is likely to reduce TOF MRA signal intensity because of phase dispersion, and furthermore, slow flow signals are reduced by the saturation effect4). Owing to this character, TOF MRA is useful for detecting aneurysm inflow zone, which aids the coil embolization procedure4).
Even though the waffle-cone technique is a valuable alternative the stent application technique, it has several limitations. First, preservation of distal branches arising from the aneurysmal neck is not always guaranteed. Another limitation is associated with increased flow through stent directly to the aneurysm, because direct flow stress can cause coil compaction and subsequent recanalization. Early follow up angiography is mandatory for patients treated using the waffle cone technique.
Stent-assisted coiling such as, Y-configured double stenting or cross-over stenting procedure must be considered to be the first treatment options. Nevertheless, the waffle-cone technique provides an innovative alternative when it is difficult to catheterize distal segments bilaterally.
We report two cases of a wide-necked basilar bifurcation aneurysms treated using the waffle-cone technique using a Solitaire stent without complication. Because distal vessel preservation is not always guaranteed during coiling when this technique is used, Y-configured double-stenting or cross-over stenting procedure must be considered as the treatments of choice. Nevertheless, our results demonstrate that the waffle-cone technique provides an innovative alternative to conventional stent applications when it is difficult to catheterize bilateral distal segments in wide-neck bifurcation aneurysms.
References
1. Baldi S, Mounayer C, Piotin M, Spelle L, Moret J. Balloon-assisted coil placement in wide-neck bifurcation aneurysms by use of a new, compliant balloon microcatheter. AJNR Am J Neuroradiol. 2003; 24:1222–1225. PMID: 12812958.
2. Biondi A, Janardhan V, Katz JM, Salvaggio K, Riina HA, Gobin YP. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms : strategies in stent deployment and midterm follow-up. Neurosurgery. 2007; 61:460–468. discussion 468-469. PMID: 17881956.
3. Gruber DP, Crone KR. Endoscopic washout : a new technique for treating chronic subdural hematomas in infants. Pediatr Neurosurg. 1997; 27:292–295. PMID: 9655143.

4. Horikoshi T, Fukamachi A, Nishi H, Fukasawa I. Detection of intracranial aneurysms by three-dimensional time-of-flight magnetic resonance angiography. Neuroradiology. 1994; 36:203–207. PMID: 8041440.

5. Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms : eight cases using the waffle cone technique. Neurosurgery. 2006; 58:ONS-258–ONS-262. discussion ONS-262.
6. Huang Q, Xu Y, Hong B, Zhao R, Zhao W, Liu J. Stent-assisted embolization of wide-neck anterior communicating artery aneurysms : review of 21 consecutive cases. AJNR Am J Neuroradiol. 2009; 30:1502–1506. PMID: 19461055.

7. Kelly ME, Turner RD 4th, Moskowitz SI, Gonugunta V, Hussain MS, Fiorella D. Delayed migration of a self-expanding intracranial microstent. AJNR Am J Neuroradiol. 2008; 29:1959–1960. PMID: 18719038.

8. Klisch J, Clajus C, Sychra V, Eger C, Strasilla C, Rosahl S, et al. Coil embolization of anterior circulation aneurysms supported by the Solitaire AB Neurovascular Remodeling Device. Neuroradiology. 2010; 52:349–359. PMID: 19644683.

9. Moret J, Cognard C, Weill A, Castaings L, Rey A. [Reconstruction technic in the treatment of wide-neck intracranial aneurysms. Long-term angiographic and clinical results. Apropos of 56 cases]. J Neuroradiol. 1997; 24:30–44. PMID: 9303942.
10. Murao K, Yamada N, Miyamoto S, Hyuga T, Kudo T, Satow T. Identification of inflow zone of cerebral aneurysm by MRA for effective coil embolization. Surg Cereb Stroke. 2008; 36:459–463.

11. Perez-Arjona E, Fessler RD. Basilar artery to bilateral posterior cerebral artery 'Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms : report of three cases. Neurol Res. 2004; 26:276–281. PMID: 15142320.

12. Pierce DS, Rosero EB, Modrall JG, Adams-Huet B, Valentine RJ, Clagett GP, et al. Open-cell versus closed-cell stent design differences in blood flow velocities after carotid stenting. J Vasc Surg. 2009; 49:602–606. discussion 606. PMID: 19268763.

13. Ryu CW, Koh JS, Lee CY, Kim EJ. Endovascular management of the wide-neck aneurysms : the applications of the coils and catheter. Neurointervention. 2010; 5:71–78.

14. Sychra V, Klisch J, Werner M, Dettenborn C, Petrovitch A, Strasilla C, et al. Waffle-cone technique with Solitaire™ AB remodeling device : endovascular treatment of highly selected complex cerebral aneurysms. Neuroradiology. 2011; 53:961–972. PMID: 20821314.

15. Wanke I, Doerfler A, Schoch B, Stolke D, Forsting M. Treatment of wide-necked intracranial aneurysms with a self-expanding stent system : initial clinical experience. AJNR Am J Neuroradiol. 2003; 24:1192–1199. PMID: 12812954.
Fig. 1
Case 1. Brain CT, CT angiograms (CTAs) and time of flight MR angiograms showing a basilar bifurcation giant aneurysm and a small anterior communicating artery (AComA) aneurysm. Brain CT (A) showing a subarachnoid hemorrhage in both Sylvian cisterns, the anterior interhemispheric fissure and right ambient cistern (Fisher grade III). A round, slightly hyperdense lesion depicted in the suprasellar cistern. CTAs (B and C) demonstrating a large basilar bifurcation aneurysm, which was considered ruptured, and an AComA small unruptured aneurysm. MR angiograms (D and E) clearly visualizing the inflow zone of a basilar bifurcation aneurysm from orifice to dome. The basal portion of aneurysm was not definitely visualized because of stagnant blood flow.
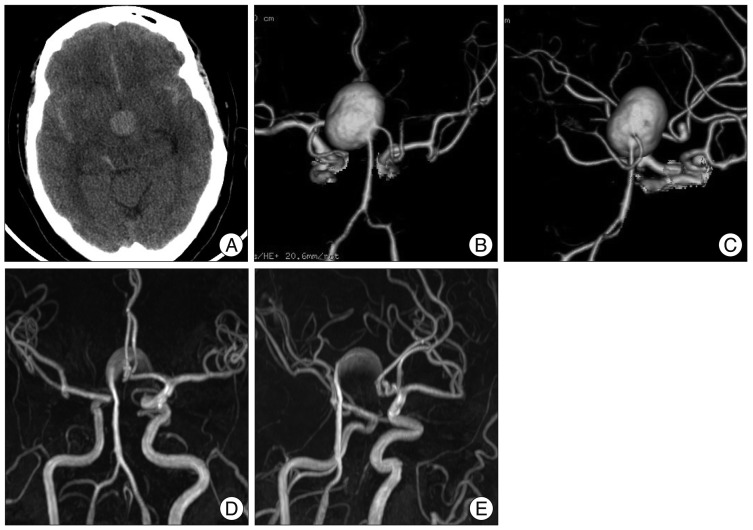
Fig. 2
Case 1. Preoperative, intraoperative and postoperative digital subtraction angiography. Preoperative AP (A) and lateral (B) vertebral angiograms showing a broad-necked giant basilar bifurcation aneurysm. Left posterior cerebral arteries (PCA) flow was visualized faintly, suggesting dominant flow from the posterior communicating artery. The orifices of both PCAs and superior cerebellar arteries (SCAs) were found to be incorporated in the giant aneurysm by 3-dimensional rotational angiography (3DRA) (C). A Solitaire intracranial stent (4×20 mm) is deployed into the aneurysmal sac distally, and into the distal basilar artery proximally in a 'waffle-cone' manner to protect the orifices of the right P1 and both SCAs (D). Partial obliteration of the giant basilar bifurcation aneurysm is achieved after 31 packing coils using the double catheter technique (E-H). Postoperative 3DRA demonstrating patent flow to both PCAs and SCAs (I).
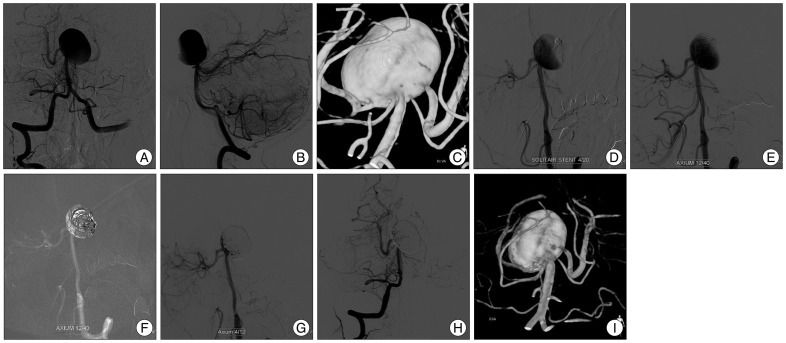
Fig. 3
Case 2. Preoperative, intraoperative and postoperative digital subtraction angiography. Preoperative AP (A) and lateral (B) vertebral angiograms showing a broad-necked, large aneurysm of basilar bifurcation. Both P1s are incorporated in the aneurysm by 3-dimensional rotational angiography (C). A 4×20 mm Solitaire stent is deployed into the aneurysmal sac distally, and the distal basilar artery proximally in a waffle-cone manner to protect the orifices of both P1s and to support the coil mass (D). Near complete obliteration of the large basilar bifurcation aneurysm is achieved with 11 coils, while sparing flows of both PCAs (E and F). PCA : posterior cerebral artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download