Abstract
In conventional percutaneous disc surgery, introducing instruments into disc space starts by inserting a guide needle into the triangular working zone. However, landing the guide needle tip on the annular window is a challenging step in endoscopic discectomy. Surgeons tend to repeat the needling procedure to reach an optimal position on the annular target. Obturator guiding technique is a modification of standard endoscopic lumbar discectomy, in which, obturator is used to access triangular working zone instead of a guide needle. Obturator guiding technique provides more vivid feedback and easy manipulation. This technique decreases the steps of inserting instruments and takes safer route from the peritoneum.
One of the most important steps in percutaneous endoscopic lumbar discectomy (PELD) is inserting a guide needle into the annulus18). Since obturator and working cannula follow the route of a guide needle, inserting a guide needle could determine the success of a surgery. Most surgeons recommend that the needle should arrive at the medial pedicle or mid-pedicular line when it touches the annulus7,10,12,18,19). However, the obligation that the tip of a guide needle should land on the exact annular landmark poses a significant challenge during endoscopic surgery. It is not easy to accurately predict the final destination of a needle on the annulus because it is affected by multiple factors like the size of the neural foramen, the needle entry from the midline, and the width of the pedicle. Often guide needle will not go in the direction a surgeon would normally project5). If the needle tip is not in the optimal position, adjustment of the needle tip is corrected only by repeating the needling procedure13). Multiple C-arm monitoring is also mandatory in both the AP and lateral planes.
With the new technique, we tried to enhance the safety and reduce drawbacks associated with this needling process. We evaluated the feasibility of this technique by the number of attempts required to insert an obturator into the working zone. Further, we have described the geometrical background behind this new technique.
Forty-one consecutive patients were treated using the obturator guiding technique. The patients had not responded to at least 2 weeks of medical treatment. They had equivalent symptoms due to herniated disc fragments. Patients with lateral recess stenosis, bony spurs, foraminal/extraforaminal disc and instability were not included. L5/S1 cases with high iliac crests were also excluded. The levels of surgeries were L2/3 in 4 patients, L3/4 in 7 patients, and L5/S1 in 3 patients; L4/5 was the most common level with 27 patients. All procedures were done under general anesthesia.
The feasibility of the obturator guiding technique was evaluated by the numbers of attempts to insert an obturator into triangular working zone. The attempt consists of moving the tip of an obturator from the lateral facet to the annulus in the triangular working zone. Whenever the obturator was withdrawn and inserted again from the lateral facet, the number of attempts increased. The clinical results were determined to be excellent, good, fair, or poor, according to the MacNab classification21).
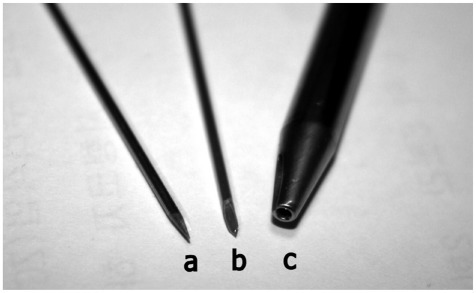
For this new technique, we designed a new guide wire (Fig. 1). This new guide wire replaces first two instruments in conventional PELD technique; guide needle and guide wire (Fig. 1). New guide wire has a diameter of 1.22 mm (about the diameter of a conventional guide needle) which is thicker than conventional guide wire. New guide wire also has a very sharp tip to navigate through soft tissue to the lateral facet. This new guide wire shortens conventional two steps of inserting a guide needle and then a guide wire to one step of inserting a new guide wire.
The patient is placed in the prone position. The perpendicular view of the lateral border on the axial scan is used to project a line between an entry point and the neural foramen. The entry point is usually 8-14 cm from the midline. The point is marked on the skin under fluoroscopic guidance. The entry point is projected to have 25 degrees (from coronal plane) for L4-5, 35 degrees for L3-4, 40 for L2-3, and 45 for L1-2. A stab incision is made with a number 11 blade. It is inserted under the biplanar guidance of fluoroscopy. The new guide wire is designed not to slip off from the lateral facet with its sharp tip when obturator is introduced; it is aimed at the lateral border of the superior facet targeting an area just posterior to the disc space (Fig. 2). This target area can be verified by pre-operative CT or MRI. After securing the wire on the facet, obturator (YESS system; Richard Wolf, Knittlingen, Germany) is introduced gently by twisting back and forth (Fig. 2). For easier introduction of the obturator, a deeper skin incision is required. Once bony contact is established, the new guide wire is removed and the tip of the obturator should be directed towards the ventral border of the facet by elevating the other end of the obturator. The obturator is slid into the triangular working zone by twisting back and forth while pushing it against the facet (Fig. 3). The ventrolateral and ventral borders of the facet work as guiding rail. The obturator should not lose contact with the facet at any time. Having a 6 mm diameter, obturator is usually engaged between the annulus and the facet before it reaches the medial pedicle. Based on this engagement, the working sheath is introduced. Under endoscopic guidance, the discectomy is started. Rest of the procedure of removing disc material is not different from conventional technique.
According to the MacNab criteria, 26 patients had excellent results, 13 patients had good results, and 2 patients had fair results. There were no approach-related complications, such as dysesthesia and nerve root injuries. In 37 cases, the obturator was introduced into the triangular working zone in just 1 attempt. Two attempts were required in 2 cases, and 3 attempts were required in 2 cases.
The conventional endoscopic technique requires a guide needle to access the disc space which is the final destination of the all endoscopic instruments. This has been true from the beginning of the percutaneous surgery since Hijikata8), Friedman6), Onik et al.23) and Schreiber and Suezawa29) started their procedures. In the obturator (or dilator) guiding technique, surgeons navigate obturator to reach the triangular working zone instead of conventional guide needle. Although new guide wire reaches the lateral facet, the role of a conventional guide needle to reach the disc space is carried out by an obturator. In conventional technique, the stylet of the needle is withdrawn and replaced by a fine Kischner wire, while the needle is still in the disc space13). However, this stage happens on the lateral facet in the obturator guiding technique. While new guide wire tip is on the lateral facet, obturator is inserted based on that bony resistance. Additional guiding from the lateral face is carried out with the obturator into the disc space in the new technique. Conventional 18G needle is not necessary in the new technique.
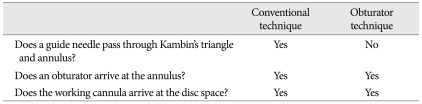
Inserting a guide needle into the disc space has been a universal feature of all endoscopic lumbar discectomy4,9,19,20,24,25,27,31). Usually, it is a 6-10 inch long 18-G needle, of which the target is the annular window on the dorsolateral aspect of the intervertebral disc30,32). 2012However, the remainder of the procedures is not different from the conventional technique. An obturator arrives at the annulus and a working cannula is introduced and a discectomy is started under endoscopic view as usual (Table 1). The indication of this technique is not different from ordinary PELD surgery either. Any intracanalicular lumbar disc fragment that could be approached through the neural foramen could be candidate for this technique.
An issue with the conventional guide needle is that it is difficult to manipulate. When a needle is longer than 3.5 inches, needle navigation is challenging because it follows the path of least resistance5). The angle of the needle bevel face is another factor that determines the direction of a needle. Since the needle is deflected by tissue resistance, the needle will often not go in the direction surgeons would normally expect5). When redirection is required, a guide needle has to be withdrawn first. Then, it is redirected and advanced again. The amount of redirection varies according to tissue resistance, the bevel of the needle, and the surgeon's skill. When it is not optimally oriented, the needling procedure has to be repeated13). This could be problematic when it is introduced into the triangular working zone bound by the exiting nerve root and dura over the dorsolateral aspect of the intervertebral disk. The obturator technique can enhance the feasibility and safety by a difference in manipulation technique. An obturator has a 6 mm diameter and is made of metal. It is not deflected by the bevel face. The rounded tip does not cut through structures around Kambin's triangle. Rather, the blunt end has a tendency to push the nerve root aside11). When an obturator is redirected, it does not require a repeated withdrawal and advancing procedure; it is simply redirected as much as the surgeon desires (Fig. 4). The amount of redirection can be controlled very accurately. When the obturator contacts the bone and annulus, the feedback is more vivid than a conventional guide wire. This feature is very helpful when the obturator is inserted between the exiting nerve root and the facet.
Another benefit of this technique is that it allows more room from important structures; the peritoneum, epidural space, and dura. In this technique, new guide wire is aimed at a lateral facet, which is more dorsal than a target in the conventional technique. In this way, the chance of violating the peritoneum or bowel could be decreased (Fig. 5). Also, it allows more distance from the epidural space and dura by eliminating a needle tract into the annulus (Fig. 6A). When we compare the position of a needle (18 G) and working cannula (7 mm diameter) in the conventional technique, the needle track is always closer to the epidural space than the tip of a working cannula (Fig. 6A). Since it has a bigger diameter (6 mm), an obturator has a greater chance of engagement between the annulus and the facet before it enters the epidural space. This feature prevents inadvertent violation of the epidural space by the obturator. This is especially true when the height of a neural foramen is narrower than the diameter of an obturator (Fig. 6B). When the neural foramen is small, a shallower access angle or more lateral skin entry point is usually required24). However, the greatest restriction to the shallower access angle in the conventional technique comes from the final destination of a guide needle on the annulus. To prevent a dural injury, the needle should not reach more medially than the innermost margin of the pedicle30). In this technique, the bigger diameter of an obturator allows more tangential access angle for a rigid endoscope because of the absence of the needle track and the obturator engagement between the facet and the annulus.
If a conventional guide needle is used for this technique to arrive at the lateral facet, the commercial guide wire could slip off the lateral facet. Although it should withstand the pressure of introducing an obturator while it is anchored on the lateral facet, the wire often slips off because the tip is rounded. By using a sharp new guide wire, we could also skip the procedure of inserting and removing a guide needle. Also, new guide wire provides better resistance because it is thicker than conventional guide wire. The new guide wire can be easily prepared by sharpening the tip of any K-wire with 1.2 mm diameter.
Traditionally PELD has been regarded as more safe procedure than open laminectomy2). The main benefit of this procedure is less damage to the musculo-ligamentous structures and shorter hospital stay7,11,13,22). However, PELD procedures are not completely free from surgical complications. Recently Ahn et al.2) reported 1.1% of symptomatic dural tears from 816 consecutive cases. All of the patients underwent open repair regarding herniated nerve fibers through the dural defect. Typical symptom of dural injury was relapse of intractable radicular pain, which is characterized by electric shock-like in nature. Motor weakness may also accompany this compli-cation3). Temporary dysesthesia has been most common complication reported previously. This complication showed incidence of 2-6.53% according to the authors3,14,18,26-28). The symptom is postulated to come from irritation of the exiting root or traversing root during the operation. Confirmation of the safe triangle is important preventing this issue18).
Although hematomas and infection are commonly observed with open discectomy procedures, they are not common with percutaneous procedures. Kotilainen et al.17) evaluated the incidence of postoperative epidural hematomas by means of magnetic resonance imaging (MRI) in 44 patients who underwent successful surgery for lumbar disc herniation. They found out significantly less hematomas with percutaneous procedures. However, retroperitoneal hematomas or psoas muscle hematomas were more commonly reported1,15,27). Kim et al.15) reported large psoas muscle hematoma after lumbar endoscopic discectomy, which was absorbed spontaneously with conservative treatment. They postulated the origin of the hematoma to be the segmental artery. Savitz27) postulated psoas muscle bleeding was from the perianular veins or muscle layers. Although infection is rare complication of PELD14), one case of pyogenic spondylodiscitis was originated by inappropriate approach during surgery. Kim et al.16) reported large pyogenic spondylodiscitis after endoscopic discectomy. This case has to do with the contact of instrument with the intestine during the surgery because the causative organism turned out to be E. Coli16).
We evaluated the feasibility of the obturator guiding technique in 41 cases. However, absolute number of cases is not enough to compare the incidence of complication with previous reports. Further study is required to prove its benefit in preventing real incidence of complication.
The obturator guiding technique is a modification of a standard endoscopic lumbar discectomy. An obturator can be manipulated more easily and safely when it is introduced into the triangular working zone since the needle track can be eliminated. We can also decrease the risk of violating the epidural space and the peritoneum.
Acknowledgements
Byung Kwan Choi was supported for 2 years by Pusan National University Research Grant.
References
1. Ahn Y, Kim JU, Lee BH, Lee SH, Park JD, Hong DH, et al. Postoperative retroperitoneal hematoma following transforaminal percutaneous endoscopic lumbar discectomy. J Neurosurg Spine. 2009; 10:595–602. PMID: 19558294.

2. Ahn Y, Lee HY, Lee SH, Lee JH. Dural tears in percutaneous endoscopic lumbar discectomy. Eur Spine J. 2011; 20:58–64. PMID: 20582555.

3. Ahn Y, Lee SH, Lee JH, Kim JU, Liu WC. Transforaminal percutaneous endoscopic lumbar discectomy for upper lumbar disc herniation : clinical outcome, prognostic factors, and technical consideration. Acta Neurochir (Wien). 2009; 151:199–206. PMID: 19229467.

4. Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation : surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976). 2004; 29:E326–E332. PMID: 15303041.
5. Czervionke LF, Fenton DS. Fenton DS, Czervionke LF, editors. Basic Needle Manipulation Technique. Image-Guided Spine Intervention. 2003. Philadelphia: Saunders;p. 1–7.
6. Friedman WA. Percutaneous discectomy : an alternative to chemonucleolysis? Neurosurgery. 1983; 13:542–547. PMID: 6227832.
7. Hermantin FU, Peters T, Quartararo L, Kambin P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999; 81:958–965. PMID: 10428127.

8. Hijikata SA. A method of percutaneous nuclear extraction. J Toden Hosp. 1975; 5:39–44.
9. Kambin P. Percutaneous endoscopic discectomy. J Neurosurg. 1993; 79:968–969. author reply 969-970. PMID: 8246071.
10. Kambin P. Kambin P, editor. Posterolateral percutaneous lumbar discectomy and decompression. Arthroscopic Microdiscectomy : Minimal Intervention in Spinal Surgery. 1991. Baltimore: Williams & Wilkins;p. 67–100.
11. Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res. 1987; 145–154. PMID: 3652568.
12. Kambin P, McCullen G, Parke W, Regan JJ, Schaffer JL, Yuan H. Minimally invasive arthroscopic spinal surgery. Instr Course Lect. 1997; 46:143–161. PMID: 9143957.
13. Kambin P, Schaffer JL. Percutaneous lumbar discectomy. Review of 100 patients and current practice. Clin Orthop Relat Res. 1989; 24–34. PMID: 2910608.
14. Kambin P, Zhou L. Arthroscopic discectomy of the lumbar spine. Clin Orthop Relat Res. 1997; 49–57. PMID: 9137176.

15. Kim HS, Ju CI, Kim SW, Kim JG. Huge psoas muscle hematoma due to lumbar segmental vessel injury following percutaneous endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2009; 45:192–195. PMID: 19352485.

16. Kim WJ, Lim ST, Lee SH. Pyogenic psoas abscess and secondary spondylodiscitis as a rare complication of percutaneous endoscopic lumbar discectomy : a case report. Joint Dis Rel Surg. 2005; 16:163–166.
17. Kotilainen E, Alanen A, Erkintalo M, Helenius H, Valtonen S. Postoperative hematomas after successful lumbar microdiscectomy or percutaneous nucleotomy : a magnetic resonance imaging study. Surg Neurol. 1994; 41:98–105. PMID: 8115960.

18. Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo). 2008; 48:383–388. discussion 388-389. PMID: 18812679.

19. Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation : classification of disc migration and surgical approaches. Eur Spine J. 2007; 16:431–437. PMID: 16972067.

20. Lee SH, Kang BU, Ahn Y, Choi G, Choi YG, Ahn KU, et al. Operative failure of percutaneous endoscopic lumbar discectomy : a radiologic analysis of 55 cases. Spine (Phila Pa 1976). 2006; 31:E285–E290. PMID: 16648734.
21. Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971; 53:891–903. PMID: 4326746.
22. Mayer HM, Brock M. Percutaneous endoscopic discectomy : surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993; 78:216–225. PMID: 8267686.

23. Onik G, Helms CA, Ginsburg L, Hoaglund FT, Morris J. Percutaneous lumbar diskectomy using a new aspiration probe. AJR Am J Roentgenol. 1985; 144:1137–1140. PMID: 3873792.

24. Ruetten S, Komp M, Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach-technique and prospective results of 463 patients. Spine (Phila Pa 1976). 2005; 30:2570–2578. PMID: 16284597.

25. Ruetten S, Komp M, Merk H, Godolias G. Recurrent lumbar disc herniation after conventional discectomy : a prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech. 2009; 22:122–129. PMID: 19342934.
26. Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique : a prospective, randomized, controlled study. J Neurosurg Spine. 2009; 10:476–485. PMID: 19442011.

27. Savitz MH. Same-day microsurgical arthroscopic lateral-approach laser-assisted (SMALL) fluoroscopic discectomy. J Neurosurg. 1994; 80:1039–1045. PMID: 8189259.

28. Savitz MH, Doughty H, Burns P. Percutaneous lumbar discectomy with a working endoscope and laser assistance. Neurosurg Focus. 1998; 4:e9. PMID: 17206772.

29. Schreiber A, Suezawa Y. Transdiscoscopic percutaneous nucleotomy in disk herniation. Orthop Rev. 1986; 15:35–38. PMID: 3453439.
30. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation : surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). 2002; 27:722–731. PMID: 11923665.
31. Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery : foraminal approach. Surg Technol Int. 2003; 11:255–263. PMID: 12931309.
32. Yeung AT, Yeung CA. Kim DH, Fessler RG, Regan JJ, editors. Posterolateral selective endoscopic diskectomy : the YESS Technique. Endoscopic Spine Surgery and Instrumentation : Percutaneous Procedures. 2005. New York: Thieme Medical Pub;p. 201–211.
Fig. 2
An obturator (O) is slid in while a new guide wire (G) is anchored on the target area (T) on the lateral facet.

Fig. 3
Once bony contact along the facet is established, the tip of the obturator should be directed towards the ventral border of the facet by elevating the other end of the obturator. The obturator is slid into the safe triangle by twisting back and forth while pushing it against the facet.

Fig. 4
Difference of redirection methods in two techniques. A : For the conventional technique, a guide needle has to be withdrawn first (dotted arrow), redirected, and then advanced again (arrow). B : For an obturator, it can be redirected without withdrawing it.
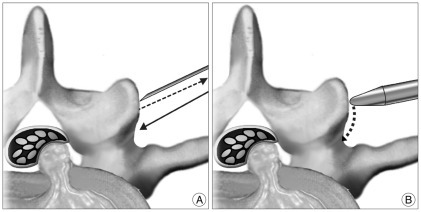
Fig. 5
When a needle (or new guide wire) is aimed at a more dorsal target (O) than a target in conventional technique (C), the chance of violating the peritoneum can be decreased by the distance, d.
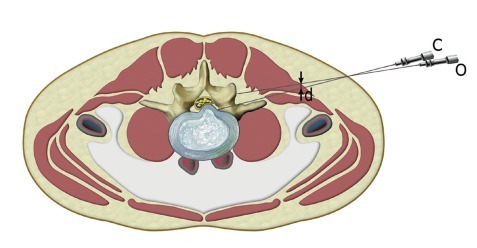
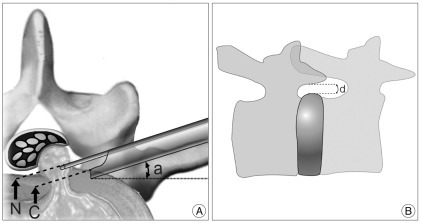
Fig. 6
Relationship between the size of the neural foramen and the chance of violating the epidural space. A : A needle track (N) is always closer to the epidural space than the tip of a working cannula (C). When the needle track (N) can be eliminated, the chance of violating the epidural space could be decreased. The access angle (a) could be decreased to have a shallower approach without increasing the risk of violating the epidural space. B : When the height of a neural foramen, d, is smaller than the diameter of an obturator, it is engaged between the annulus and pedicle before the tip enters the epidural space.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download