Abstract
This report describes a rare case of postoperative hyperventilation attack after an endoscopic third ventriculostomy in a 46-year-old woman. About 60 min after the termination of the operation, an intractable hyperventilation started with respiratory rate of 65 breaths/min and EtCO2, 16.3 mm Hg. Sedation with benzodiazepine, thiopental sodium, fentanyl, and propofol/remifentanil infusion was tried under a rebreathing mask at a 4 L/min of oxygen. With aggressive sedative challenges, ventilation pattern was gradually returned to normal during the 22 hrs of time after the surgery. A central neurogenic hyperventilation was suspected due to the stimulating central respiratory center by cold acidic irrigation solution during the neuroendoscopic procedure.
Endoscopic third ventriculostomy is a minimal invasive technique with approximately 6-8% of complication rate, those are CSF leak, pneumocephalus, subdural hematoma, bradycardia/asystole, injury to periventricular structures, etc17). Hyperventilation attack after an endoscopic third ventriculostomy has been also reported and these cases were regarded to the result of central mechanisms2,14). A generous irrigation during the endoscopic surgery may cause the disturbance of electrolytes, pH, and temperature, thus producing a direct stimulus over the respiratory centers located on the brainstem2).
We present a case of hyperventilation attack after an endoscopic third ventriculostomy operation which was hardly controlled with various sedative challenges.
A 46-year-old woman (159 cm, 59 kg) suffered from several years of headache and memory disturbance was scheduled for the endoscopic third ventriculostomy for aqueductal stenosis with hydrocephalus (Fig. 1). She had no notable family or medical history except a urinary incontinence surgery operated one month ago. There were no other specific events at that time.
BP was 130/80 mm Hg, HR 90 bpm, BT 36.6℃, and SpO2 99%. The level of serum calcium was 8.7 mg/dL (normal; 8.6-10.6) and potassium was 3.5 mEq/L (normal; 3.5-5.5). Under standard monitoring, 0.2 mg of glycopyrrolate was intravenously injected as premedication. Anesthesia was conducted with 60 mg of propofol, 100 µg of fentanyl, and 50 mg of rocuronium, then maintained with sevoflurane and equal mixture of O2 and N2O. The third ventriculostomy was performed with a neuroendoscopy through burr hole on the skull, and then an EVD catheter was inserted to the Rt. lateral ventricle for further drainage of CSF. About 200-300 mL of normal saline stored at room temperature was irrigated while the procedure and the fluid were naturally drained. Vital signs were stable during the surgery, and the patient was extubated after 130 min of anesthesia. During the 30 min of recovery at postanesthesia care unit, BP showed 140/80 mm Hg, HR 90-100 bpm, and SpO2 98% with 6 L of oxygen by a venturi mask. The patient looked comfortable.
During taking a postoperative brain CT, the patient became nervous. Postoperative pH was 7.477, pCO2 20.7 mm Hg, pO2 137 mm Hg, BE -0.63 mmol/L, HCO3 15.1 mmol/L, SaO2 98%, and K 3.7 mEq/L. Twenty min after IV injection of sodium bicarbonate 40 mEq, a regular pattern hyperventilation started. The patient vomited and eyeballs deviated upward with respiratory rate (RR) of 50 breaths/min. A total dose of midazolam 3 mg, lorazepam 8 mg, and diazepam 22.5 mg were IV injected for 5 hrs, however, the RR increased to the 65 breaths/min and muscle rigidity was observed. Laboratory tests showed that pH 7.58, pCO2 16.3 mm Hg, pO2 107 mm Hg, BE -4.7 mmol/L, HCO3 15.1 mmol/L, SaO2 97.3%, K 2.8 mEq/L, and ionized Ca 3.45 mg/dL (normal; 4.07-5.17).
Breathing sound was nonspecific on auscultation and BP showed 107/70 mm Hg, HR 110 bpm, and SpO2 99% in room air. Midazolam 5 mg and fentanyl 100 µg were IV injected with 4 L/min oxygen via a rebreathing mask, however, no notable changes were observed. Therefore, propofol was infused during the 2 hrs and RR decreased up to the 45 breaths/min. For further decrement of respiration, remifentanil infusion was added, however, it was stopped few minutes later because VT rather than RR decreased and upper airway obstruction was observed. Without definite improvement, thiopental sodium 250 mg was IV injected in attempt to cease self respiration, however, only VT decreased and recovered immediately. Blood gas tests were pH 7.52, pCO2 27.7 mm Hg, pO2 214 mm Hg, BE 0.7 mmol/L, HCO3 22.5 mmol/L, and SaO2 98.1%.
RR progressively decreased to the 27 breaths/min during the five hours after the infusion of propofol, therefore, we stopped the infusion of propofol and waited for the patient awake. With consciousness turning back, RR increased to the 34 beats/min, but no further increase was observed. RR slowly decreased to the 20 breaths/min within 10 hrs. The results of blood gas tests showed normal (Fig. 2).
BP was maintained within 100-150/60-90 mm Hg, HR 70-109 bpm, and BT 37.0-37.3℃ during the hyperventilation period. Thyroid function test, levels of troponin-I, CK-MB, D-dimer, and Fbg were all in normal ranges. The patient had postoperative dizziness and left side motor weakness with gait disturbance just after the operation (Lt. G4/Rt. G5), however, no evidence of hemorrhage or infarct was observed on brain CT. Preoperative symptoms such as headache and memory disturbance were resolved after the operation and she discharged without complications 20 days after physical therapy.
Hyperventilation is defined as breathing in excess of the metabolic needs of the body, eliminating more CO2 than is produced3). The symptoms are dyspnea, parasthesia, muscle spasm, and those results from overstimulation of the autonomic nervous system such as sweating, nausea, and vomiting. Tachycardia and refractory cardiac arrhythmia often occur due to the increased sympathetic activity. Also, chest pain or tightness may produce symptoms or diseases related to coronary vasoconstriction. Hyperventilation also causes cerebral vasoconstriction and decrease cerebral blood flow, thus light-headedness, dizziness, loss of consciousness, and even seizure may be developed10).
Common causes of peripheral organic hyperventilation are pulmonary embolism, asthma, pneumothorax, ischemic heart disease, congestive heart failure, hyperthyroidism, pheochromocytoma, drug/alcohol withdrawal, fever, and pain10). When hyperventilation occurs, peripheral organic causes should be ruled out first. It is quite predictable and detectable with physical, laboratory, and radiological tests. In this patient case, it was not suspected because vital signs were relatively stable and laboratory tests were within normal ranges including D-dimer, troponin-I, CK-MB, and thyroid hormone. Breathing sound, ECG, postoperative brain CT, and chest X-ray were not specific, either.
As the patient was found to be nervous all the time and afraid of hair shaving, psychogenic hyperventilation (non-organic hyperventilation) was suspected first. A psychogenic hyperventilation is a picture of panic disorder and common in the third and fourth decade female with 6-11% of occurrence4). Some medications and conditions such as hyperventilation itself, breath-holding, CO2 inhalation, sodium lactate or bicarbonate infusion, or sympathetic stimulator administration are known to provoke HVS in panic patients5). The pathophysiology of lactate induced HVS is still unclear, however, metabolic controlled central hypercapnia mechanism is highly suspected. According the mechanism, sodium lactate metabolizes to bicarbonate, which transverses blood-brain-barrier poorly and induces metabolic alkalosis. Hypoventilation may develop due to the compensatory mechanism, thus CO2 retention may occur. Further, sodium bicarbonate hydrolyzed to carbonic acid, which dissociates to CO2 and water. CO2, unlike bicarbonate, freely penetrates the blood-brain-barrier, and then hypercapnia sets off the brain-stem CO2 chemoreceptors, leading to hyperventilation. Only panic patients show such responses, because they have a lower threshold for anxiety producing and their PaCO2 receptors are more responsive to the changes in PaCO2 than normal people5). Usually 10 mL/kg of 0.5 M (or 5 mL/kg of 1 M) sodium lactate or 8 mL/kg of 0.5 M sodium bicarbonate is often used to provoke hyperventilation and the onset of hyperventilation is 12.03 min on an average9). In this patient, only 40 mL of 0.5 M sodium bicarbonate was injected. A typical aspect of hyperventilation was observed 20 min after sodium bicarbonate injection, however, the blood gas study taken before the attack already suggested severe respiratory alkalosis. Also, in a lactate provocation test, panic symptoms subsided within 20 to 30 min if lactate infusion was stopped immediately after a patient panics, not like this case. Moreover, according to other reports, psychogenic hyperventilation was subsided when sedation reached proper level of depth8,11,15), different from this case. In this case, propofol was infused at the dose of 60 µg/kg/min to the already fully sedated patient, however, hyperventilation was sustained. These findings imply that this attack may not be simply caused by a psychiatric problem or lactate administration.
Central organic hyperventilation (central neurogenic hyperventilation, CNH) is defined as respiratory alkalosis induced by lesions in the CNS without other organic diseases1). Hyperventilation persists during the sleeping in CNH and the characteristics of CNH are normal or increased arterial oxygen tension, decreased arterial carbon dioxide tension, and respiratory alkalosis in the absence of cardiac, pulmonary, and respiration-stimulating drugs12). Although the pathophysiologic mechanism of CNH is unclear, dysfunction of the reticular formation of the midbrain and upper pons is thought to be correlated with this syndrome1). Most of cases of CNH is derived from CNS tumor especially lymphoma, and invasion of tumor to brainstem and low CSF pH due to local production of acidic substance are regarded for the reason7). Not only tumor, but ischemia or trauma can also provoke CNH. Among the five cases of postoperative hyperventilation reported previously2,8,11,14,15), two intractable hyperventilations occurred after endoscopic third ventriculostomy (Table 1)2,14). During neuroendoscopic surgery, continuous or intermittent rinsing is required to get good direct vision. Large volume of normal saline or Ringer's solution is often used and it exits the brain passively through a specific evacuation channel. Fàbregas et al.2) reported complications of neuroendoscopy in 100 patients and hyperventilation was shown in one case among them. They assumed that complications might be caused by the excessive irrigation pressure (≥30 mm Hg) applied to brain structures, especially to the respiratory centers; 49 percent of patients showed irrigation pressure higher than 30 mm Hg, 25% showed over 50 mm Hg, and 4 patients over 100 mm Hg in their study. Changes in ionic composition, pH, body temperature, and the flow direction of CSF by irrigation fluid are another possible explanations producing direct stimulus over the respiratory centers located on the brainstem2). Sung et al.14) reported a case of hyperventilation which used 3000 mL of normal saline at room temperature with maximum pumping pressure of 500 mm Hg for endoscopic irrigation. Late arousal and hyperventilation over 66 breaths/min were observed postoperatively, with no response to massive sedatives. Ventilatory care was done following orotracheal intubation, and weaning was accomplished on the next day without problems. This case, also, was given large volume and high pressure of irrigation fluid as the reason of transient injury of periventricular structures. In our case, the exact pressure of irrigation fluid was not measured, however, it was regarded to be high enough to give transient injury to brainstem.
Treatments of hyperventilation are different depending on the causes. If hyperventilation is originated from peripheral organic causes, correction of each abnormality is mandatory. Reassurance is essential to treat psychogenic hyperventilation and antidepressants and benzodiazepines are often regarded as the drug of choice5). The efficacy of propofol is still debating. Tomioka et al.15) described that midazolam was effective for HVS while propofol was not, but Kim et al.8) reported that propofol was quite effective. Opioid was effective in CNH, so it suggested that opioids bound to the both mu and delta receptors decreased respiratory rate, rhythmicity, and pattern, as well as responsivity to CO21,7), however, it was not seen in our case. A synergic effect of remifentanil and massive sedatives might induce respiratory depression, therefore, therapeutic dose of opioid could not be used. If it was used at first with fewer sedatives, it could have been effective. Rebreathing with a paper bag could be a good choice during the hyperventilation period, however, it should be used with caution. It can be dangerous in hyperventilation due to pulmonary or cardiac disease, because hypoxemia may result in cardiac arrest. Tomioka et al.15) experienced that rebreathing with a paper bag was not effective, and van den Hout et al.16) reported that paper bag ventilation increased alveolar CO2 more significantly only with patients' expectation to do so. We did not use the paper bag because the patient was already sedated with massive sedatives and had a history of vomiting once. In this case, a rebreathing mask was applied with a low flow rate of oxygen to accumulate CO2 in the mask space and provide higher inspiring O2 with secure the vision of patient's airway.
In neurosurgical anesthesia, a hyperventilation method is often used to improve intracranial compliance and in such cases, PaCO2 tension should be maintained between 25 and 30 mm Hg to avoid cerebral hypoxia. In a case study, eight piglets hyperventilated to PaCO2 less than 20 mm Hg revealed that brain blood flow decreased up to 40% at 30 min following the induction of respiratory alkalosis6). In other study with human volunteers, EEG abnormalities and paresthesias occurred at the PaCO2 less than 20 mm Hg, and these effects were reversed by hyperbaric oxygenation13). However, in this patient, PaCO2 was decreased to 16.3 mm Hg and remained less than 20 mm Hg for 3-5 hrs which might have caused cerebral vasoconstriction. The prompt use of mechanical ventilation can decrease complications. Additionally, a generous irrigation method is emphasized in the neuroendoscopic surgeries, and intracranial pressure is recommended to be monitored to prevent the complications associated with brain dysfunctions.
This case is thought to be a central neurogenic hyperventilation. When unexplainable hyperventilation attack arises, peripheral organic causes should be ruled out first, then a psychogenic or a central neurogenic hyperventilation to be considered. To avoid cardiac and cerebral ischemia, supplemental oxygen and early restoration of normal PaCO2 level and normal breathing pattern are necessary.
References
1. Adachi YU, Sano H, Doi M, Sato S. Central neurogenic hyperventilation treated with intravenous fentanyl followed by transdermal application. J Anesth. 2007; 21:417–419. PMID: 17680198.

2. Fàbregas N, LÓpez A, Valero R, Carrero E, Caral L, Ferrer E. Anesthetic management of surgical neuroendoscopies : usefulness of monitoring the pressure inside the neuroendoscope. J Neurosurg Anesthesiol. 2000; 12:21–28. PMID: 10636616.
3. Folgering H. The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis. 1999; 54:365–372. PMID: 10546483.
4. Foster GT, Vaziri ND, Sassoon CS. Respiratory alkalosis. Respir Care. 2001; 46:384–391. PMID: 11262557.
5. Hales RE, Yudofsky SC. Textbook of clinical psychiatry. 2003. ed 4. Washington D.C.: American Psychiatric Publishing Inc;p. 543–565.
6. Hansen NB, Nowicki PT, Miller RR, Malone T, Bickers RG, Menke JA. Alterations in cerebral blood flow and oxygen consumption during prolonged hypocarbia. Pediatr Res. 1986; 20:147–150. PMID: 3080728.

7. Jaeckle KA, Digre KB, Jones CR, Bailey PL, McMahill PC. Central neurogenic hyperventilation : pharmacologic intervention with morphine sulfate and correlative analysis of respiratory, sleep, and ocular motor dysfunction. Neurology. 1990; 40:1715–1720. PMID: 2234427.
8. Kim G, Bae JH, Lim SW. Hyperventilation attack during recovery from general anesthesia : a case report. Korean J Anesthesiol. 2005; 49:735–738.

9. Liebowitz MR, Fyer AJ, Gorman JM, Dillon D, Appleby IL, Levy G, et al. Lactate provocation of panic attacks. I. Clinical and behavioral findings. Arch Gen Psychiatry. 1984; 41:764–770. PMID: 6742978.
10. Mason RJ, Broaddus VC, Martin TR, King TE Jr, Schraufnagel DE, Murray JF, et al. Murray & Nadel's textbook of respiratory medicine. 2010. ed 5. Philadelphia: Saunders Elsevier;p. 1842–1847.
11. Mizuno J, Morita S, Itou Y, Honda M, Momoeda K, Hanaoka K. [Hyperventilation syndrome before induction of and after awakening from general anesthesia]. Masui. 2009; 58:768–771. PMID: 19522275.
12. Plum F, Swanson AG. Central neurogenic hyperventilation in man. AMA Arch Neurol Psychiatry. 1959; 81:535–549.

13. Reivich M, Cohen PJ, Greenbaum L. Alterations in the electroencephalogram of awake man produced by hyperventilation : effects of 100% oxygen at 3 atmospheres absolute pressure. Neurology. 1966; 16:304.
14. Sung HJ, Sohn JT, Kim JG, Shin IW, Ok SH, Lee HK, et al. Acute respiratory alkalosis occurring after endoscopic third ventriculostomy : a case report. Korean J Anesthesiol. 2010; 59:S194–S196. PMID: 21286439.
15. Tomioka S, Takechi M, Ohshita N, Nakajo N. Propofol is not effective for hyperventilation syndrome. Anesth Analg. 2001; 92:781–782. PMID: 11226118.

16. van den Hout MA, Boek C, van der Molen GM, Jansen A, Griez E. Rebreathing to cope with hyperventilation : experimental tests of the paper bag method. J Behav Med. 1988; 11:303–310. PMID: 3139884.

17. Walker ML. Complications of third ventriculostomy. Neurosurg Clin N Am. 2004; 15:61–66. PMID: 15062404.

Fig. 1
Preoperative magnetic resonance image (A : Axial, T2-weighted, B : Saggital, T1-enhanced) showing lateral and third ventricular enlargement.
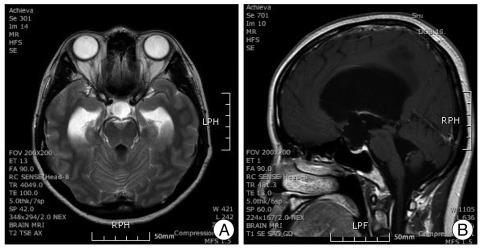
Fig. 2
Respiratory changes during hyperventilation period. Respiratory rate was slowly decreased to 20 breaths per minute during 21 hrs.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download