Abstract
Glioblastoma multiforme (GBM) is the most aggressive intracranial tumor and it commonly spreads by direct extension and infiltration into the adjacent brain tissue and along the white matter tract. The metastatic spread of GBM outside of the central nervous system (CNS) is rare. The possible mechanisms of extraneural metastasis of the GBM have been suggested. They include the lymphatic spread, the venous invasion and the direct invasion through dura and bone. We experienced a 46-year-old man who had extraneural metastasis of the GBM on his left neck. The patient was treated with surgery for 5 times, radiotherapy and chemotherapy. He had survived 6 years since first diagnosed. Although the exact mechanism of the extraneural metastasis is not well understood, this present case shows the possibility of extraneural metastasis of the GBM, especially in patients with long survival.
Glioblastoma multiforme (GBM) is the most aggressive intracranial tumor. GBM diffusely infiltrates the surrounding brain tissue, but does not typically invade blood vessels and rarely spreads outside the central nervous system (CNS). Metastasis to the outside of the CNS was accounted for in only 0.2% cases4). The most common site of extraneural metastasis of the GBM is pleura and the lung10,12). Although the exact mechanism of extraneural metastasis has been poorly understood, the lymphatic drainage, the venous system and the adjacent dura and bone have been suggested as the three possible routes of extraneural spread2). Interestingly, we experienced a rare case of extraneural metastasis of the GBM, presenting as an unusual neck mass. Herein, we report this unusual case, with review of the literature, and we suggest the risk factors of extraneural metastasis.
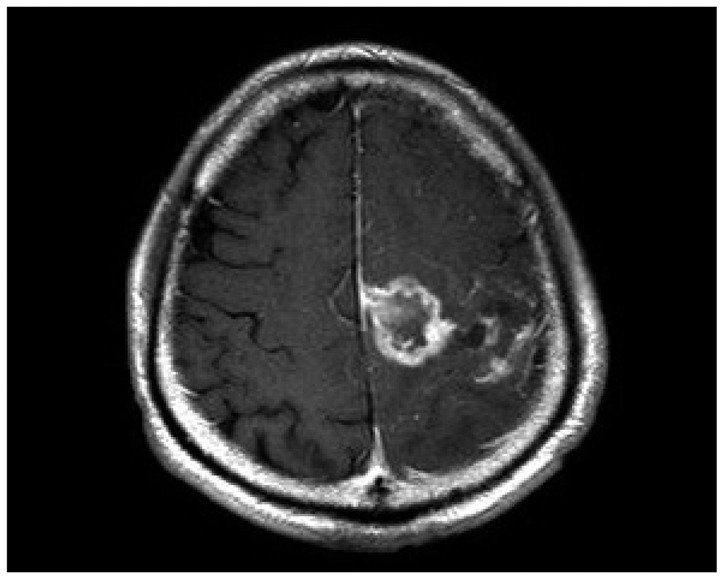
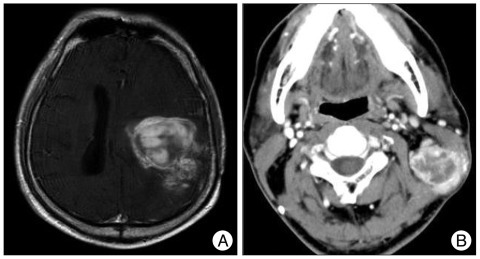
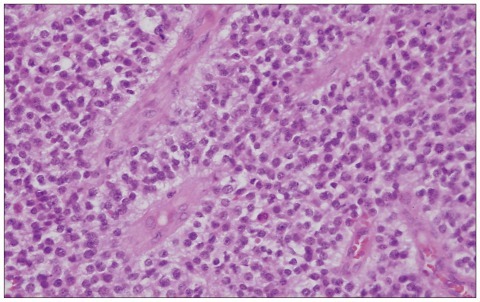
A 46-year-old man was referred to our neurosurgical unit complaining of progressive right hemiparesis. At admission, he was alert and fully oriented. Neurological examination revealed right hemiparesis (grade 3/5). In the past medical history, he had undergone a craniotomy in the left fronto-parietal region for brain tumor 10 years ago in another hospital. Although we could not obtain pathological and medical records, he informed that his brain tumor had been diagnosed as low grade glioma, and he had received radiation therapy following craniotomy. Magnetic resonance images (MRI) and computed tomography (CT) scan on admission demonstrated a poorly defined heterogenously enhancing mass with extensive peritumoral edema in the left frontal motor cortex (Fig. 1). Since the mass was located near the previous craniotomy site, we suggested that this tumor might be related with previously diagnosed glioma. Under the presumptive diagnosis of secondary tumor, malignant transformation of a low grade glioma or radiation induced glioblastoma, we performed the surgical resection of the tumor. The histopathological diagnosis was compatible with GBM (Fig. 2). After the operation, the patient made uneventful recovery and showed improvement of his right motor function. The MRI scans taken 2 weeks later showed a remnant mass in the left frontal lobe (Fig. 3). Considering his previous history of radiation therapy, we performed gamma knife radiosurgery for the remnant mass, with a marginal dose of 20 Gy to the 50% isodose line, followed by 6 cycles of adjuvant chemotherapy with the PCV regimen (i.e. procarbazine, lomustine, and vincristine). After the gamma knife radiosurgery, the patient was not followed up. Three years later, he presented with progressive weakness of the right extremities and dysarthria. The MRI showed a recurrent tumor in the left cerebral hemisphere (Fig. 4A). Surgical resection was done for the mass lesion and the histopathological findings revealed recurrence of the GBM. He remained in a stable condition during the 6 cycles of adjuvant chemotherapy with temozolomide. Since then, he underwent craniotomy two more times and shunt procedure for the recurrence of the tumor and hydrocephalus for 30 months. Five years after the initial diagnosis, a palpable mass lesion was observed on his left side of the neck. The mass was firm, tender and associated with enlarged palpable cervical lymph node. The neck CT with contrast enhancement revealed a 3×4 cm sized round mass, with peripheral rim enhancement in the left side of the neck (Fig. 4B). Mass was biopsied and the histopathology indicated a metastatic deposit of the GBM. At that time, his condition, including consciousness and motor function, worsened, and the brain MRI noted the progression of the GBM. We performed the surgical resection of the brain tumor and of the neck mass, simultaneously. The pathological specimens were shown with increased cellularity, with blood vessel proliferation and necrosis (30%). The Ki-67 proliferation index was about 50%. All pathological specimens, from both the brain tumor and the neck mass, were confirmed as GBM (Fig. 5). Despite the aggressive treatment for the GBM, the patient was aggravated and died 6 months later.
Glioblastoma multiforme is one of the most malignant neoplasms in human beings and the most common primary tumor in the cerebral hemisphere. The incidence accounts for 2 to 3 cases/100000 per year in both Europe and North America, and 75% of the patients die within 18 months from diagnosis13). GBM commonly spreads by direct extension and infiltration into the adjacent brain tissue and along the white matter tract. Although the tumor is associated with a strong tendency for local invasiveness, the metastatic spread of the GBM outside of the CNS is extremely rare. Thus, the spread outside the CNS occurs with a frequency of only 0.2%4).
The reason why the GBM rarely metastasizes is still unclear, but some hypotheses have been proposed. The first hypothesis was suggested on the basis of the short life span of patients. The severe aggressiveness of the GBM results in a very short survival period of patients. Therefore, this poor prognosis eliminates the chance of detectable metastases of GBM7). The second suggestion has been based on the barrier effect of the basement membrane. In in vitro experiments, the capillary basement membrane played an important role as a physical barrier against migration of the glioma cells into the blood stream in the brain1). As another assumption, the cellular environment of the CNS also might be related to the prevention of metastasis of the GBM, because the CNS lacks extracellular the matrix components, such as collagen and fibronectin, which are overexpressed only in the hyperplastic blood vessels. Through hyaluronic acid and other glycosaminoglycans which are main components of the extracellular spaces, the active tumor cells can migrate into the surrounding tissue. This property of the extracellular substrates can make hematogenous metastasis really rare3,9,14).
Although the exact mechanism of extraneural metastasis has been poorly understood, Cervio et al.2) suggested three possible mechanisms of extraneural spread, as follows : 1) the lymphatic cerebrospinal fluid drainage into the extraneural tissue (despite absence of an identifiable lymphatic system in the CNS); 2) the venous invasion, either via the leptomeningeal sinuses or via the intracerebral vein; 3) direct invasion through the dura and bone or through tumor cell migration along the ventriculoperitoneal shunts. Huang et al.5) described that extraneural spread after neurosurgical operation. After the surgical procedure, the tumor cells may access the lymphatic or blood circulation through the damaged blood-brain barrier (BBB). Craniotomy with tumor resection is associated with the opening of the brain vessels and can be associated with the spread of tumor cells, as previously demonstrated in the literature15). In the present case, the patient underwent several operations, which might increase the chance of distant metastasis.
In the literature, the most common sites of metastases were pleura/lungs, followed by lymph nodes, bones and liver8,11,12). In the report on the extraneural metastases of astrocytoma and glioblastoma, the distribution of metastases was, as follows : 43 (59.7%) lung and pleural, 37 (51.4%) lymph node, 22 (30.5%) bone, 16 (22.2%) liver, 5 heart, 3 adrenal gland, 2 each in the kidneys, diaphragm and mediastinum, and 1 each in the pancreas, the thyroid gland, and the peritoneum11).
For establishing the presence of extraneural metastasis, the following 4 criteria should be met16) : 1) the metastatic lesion must be histologically identified as CNS tumor; 2) the clinical history must indicate a CNS tumor as the initial neoplasm; 3) a complete autopsy must be performed to exclude the possibility of any other primary tumor; 4) the morphologic features of the primary lesion and of the metastatic lesion must be identical. In this case, the patient fulfilled these criteria.
At presentation with extraneural metastasis, this patient developed enlargement of the cervical lymph node. Since the patient showed the lymphatic involvement of the GBM as extraneural metastasis, we considered that the main pathway of extraneural metastasis might be the lymphatic spread. However, we could not exclude the hematogenous spread. The possibility of hematogenous metastasis to the neck should be included, because the patient had undergone multiple craniotomies.
Although it has been well known that surgery could be a risk factor for the extraneural metastasis of the GBM, surgery is not a prerequisite for the extraneural spread of the primary CNS tumor. Spontaneous metastases also have been reported in patients who had not experienced previous surgery6). Spontaneous spreading of the tumor was attributed to direct invasion in both the vascular and the lymphatic systems.
In summary, this patient survived for 6 years after aggressive treatments including surgery for 5 times, radiotherapy and chemotherapy. We suggest that the relatively longer lifespan of this patient might have affected the extraneural metastasis of the GBM. The damage of the cerebral vessels and of the BBB by repeated surgical manipulations could also accelerate the tumor penetration outside of the CNS.
Although the exact mechanism of the extraneural metastasis is not well understood, the GBM can metastasize to extraneural organs. Multiple craniotomies and longer survival period of the patient could be considered as risk factors of the extraneural metastasis. This present case provides proof for the possibility of extraneural metastasis of the GBM, especially in patients with longer survival. The neuro-oncologists should pay attention to the systematic survey for extraneural metastasis of the GBM.
References
1. Bernstein JJ, Woodard CA. Glioblastoma cells do not intravasate into blood vessels. Neurosurgery. 1995; 36:124–132. discussion 132. PMID: 7708148.

2. Cervio A, Piedimonte F, Salaberry J, Alcorta SC, Salvat J, Diez B, et al. Bone metastases from secondary glioblastoma multiforme : a case report. J Neurooncol. 2001; 52:141–148. PMID: 11508813.
3. Giese A, Loo MA, Rief MD, Tran N, Berens ME. Substrates for astrocytoma invasion. Neurosurgery. 1995; 37:294–301. discussion 301-302. PMID: 7477782.

4. Hsu E, Keene D, Ventureyra E, Matzinger MA, Jimenez C, Wang HS, et al. Bone marrow metastasis in astrocytic gliomata. J Neurooncol. 1998; 37:285–293. PMID: 9524086.
5. Huang P, Allam A, Taghian A, Freeman J, Duffy M, Suit HD. Growth and metastatic behavior of five human glioblastomas compared with nine other histological types of human tumor xenografts in SCID mice. J Neurosurg. 1995; 83:308–315. PMID: 7616277.

6. Liwnicz BH, Rubinstein LJ. The pathways of extraneural spread in metastasizing gliomas : a report of three cases and critical review of the literature. Hum Pathol. 1979; 10:453–467. PMID: 381159.
7. Mentrikoski M, Johnson MD, Korones DN, Scott GA. Glioblastoma multiforme in skin : a report of 2 cases and review of the literature. Am J Dermatopathol. 2008; 30:381–384. PMID: 18645311.

8. Moon KS, Jung S, Lee MC, Kim IY, Kim HW, Lee JK, et al. Metastatic glioblastoma in cervical lymph node after repeated craniotomies : report of a case with diagnosis by fine needle aspiration. J Korean Med Sci. 2004; 19:911–914. PMID: 15608410.

9. Pansera F, Pansera E. An explanation for the rarity of extraaxial metastases in brain tumors. Med Hypotheses. 1992; 39:88–89. PMID: 1435399.

10. Pasquier B, Lachard A, Pasquier D, Muller F, Couderc P, Courel-Vidard MN, et al. [Costal micrometastasis from a cerebral astrocytoma. Immunohistochemical detection (author's transl)]. Arch Anat Cytol Pathol. 1982; 30:50–55. PMID: 6282226.
11. Pasquier B, Pasquier D, N'Golet A, Panh MH, Couderc P. Extraneural metastases of astrocytomas and glioblastomas : clinicopathological study of two cases and review of literature. Cancer. 1980; 45:112–125. PMID: 6985826.

12. Rajagopalan V, El Kamar FG, Thayaparan R, Grossbard ML. Bone marrow metastases from glioblastoma multiforme--a case report and review of the literature. J Neurooncol. 2005; 72:157–161. PMID: 15925996.

13. Stark AM, Nabavi A, Mehdorn HM, BlÖmer U. Glioblastoma multiforme-report of 267 cases treated at a single institution. Surg Neurol. 2005; 63:162–169. discussion 169. PMID: 15680662.

14. Subramanian A, Harris A, Piggott K, Shieff C, Bradford R. Metastasis to and from the central nervous system--the 'relatively protected site'. Lancet Oncol. 2002; 3:498–507. PMID: 12147436.

15. Wallace CJ, Forsyth PA, Edwards DR. Lymph node metastases from glioblastoma multiforme. AJNR Am J Neuroradiol. 1996; 17:1929–1931. PMID: 8933881.
16. Weiss L. A metastasizing ependymoma of the cauda equina. Cancer. 1955; 8:161–171. PMID: 13231048.

Fig. 1
Preoperative gadolinium enhanced T1-weighted magnetic resonance image (MRI) demonstrates a mass lesion with peripheral irregular well enhancement in the left parietal region (A). Preoperative T2-weighted coronal MRI (B) and computed tomography scan (C) show bony defect (arrow) suggesting previous craniotomy near the mass lesion.
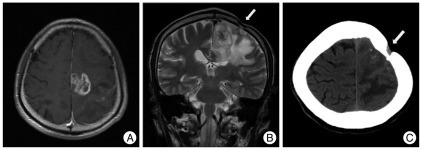
Fig. 2
Histologic findings after first operation show pleomorphic astrocytic tumor cells with mitosis and nuclear atypia (hematoxylin-eosin, original magnification, ×400).
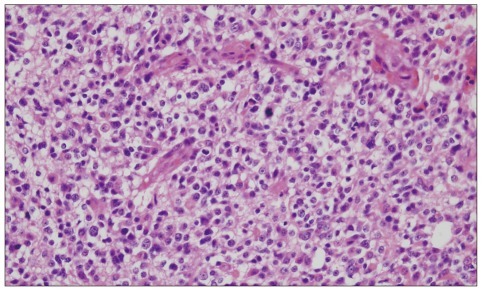
Fig. 3
Contrast enhanced magnetic resonance images taken 2 weeks after the first surgery shows remnant mass lesion in the parietal region.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download