Abstract
The authors describe a case of choriocarcinoma that metastasized to the cerebral cortex, vertebral body, and intramedullary spinal cord. A 21-year-old woman presented with sudden headache, vomiting and a visual field defect. Brain computed tomography and magnetic resonance examinations revealed an intracranial hemorrhage in the left temporo-parietal lobe and two enhancing nodules in the left temporal and right frontal lobe. After several days, the size of the hemorrhage increased, and a new hemorrhage was identified in the right frontal lobe. The hematoma and enhancing mass in the left temporo-parietal lobe were surgically removed. Choriocarcinoma was diagnosed after histological examination. At 6 days after the operation, her consciousness had worsened and she was in a state of stupor. The size of the hematoma in the right frontal lobe was enlarged. We performed an emergency operation to remove the hematoma and enhancing mass. Her mental status recovered slowly. Two months thereafter, she complained of paraplegia with sensory loss below the nipples. Whole spine magnetic resonance imaging revealed a well-enhancing mass in the thoracic intramedullary spinal cord and L2 vertebral body. Despite chemotherapy and radiotherapy, the patient died 13 months after the diagnosis.
Choriocarcinoma is a malignant form of gestational trophoblastic neoplasia10). The prognosis is considered to be very poor, and metastases often develop early3). The most common sites for metastasis are the vulvo-vaginal region, the lungs, the liver and the brain3,5,9,10). The spinal metastasis of choriocarcinoma is extremely rare11). Four cases of metastasis to the lumbar vertebral column and 2 cases to the epidural space have been reported3,6,7,10,11,14). To the best of our knowledge, no cases of metastasis in the intramedullary spinal cord have been reported in the literature. In this study, we report the case of a patient with multiple metastases to the lungs, the brain, the lumbar spinal column and the intramedullary spinal cord.
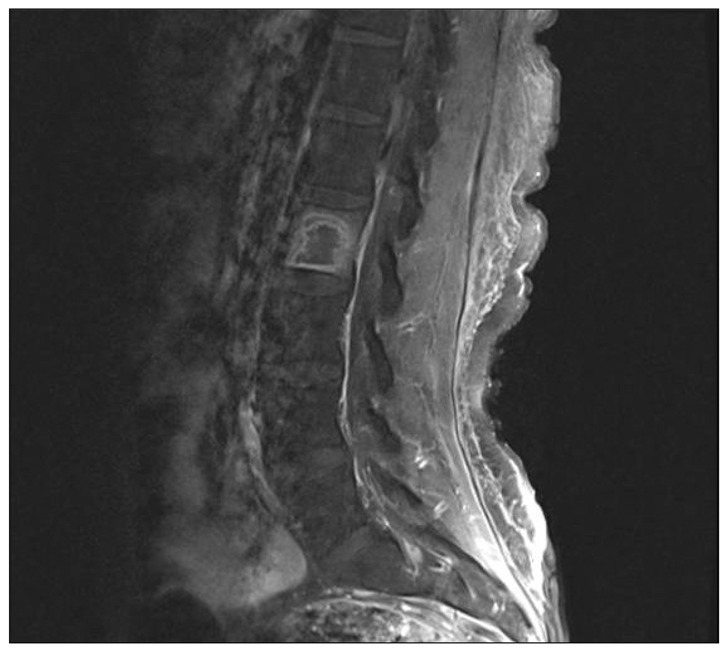
A 21-year-old woman was admitted to hospital with complaints of headache, nausea, and a visual field defect. She had a history of curettage for a complete hydatidiform mole 10 months earlier. Her mental status was drowsy. The result of visual field examination was right homonymous hemianopsia. A computed tomography (CT) scan of the brain showed a hematoma in the left temporo-parietal region. Magnetic resonance imaging (MRI) revealed a hematoma in the left temporo-parietal lobe and two enhancing nodular masses in the left temporal and right frontal regions (Fig. 1). The enhancing nodular mass in the left temporal region appeared to be associated with the hematoma. Three days after admission, her mental status suddenly began to deteriorate. A repeat CT scan revealed an increase in size of the hematoma in the left temporo-parietal region and a new hemorrhage in the right frontal region. Emergent craniotomy was performed and hematoma with the nodular mass in the left temporo-parietal region was removed. Histological examination of the mass revealed abundant trophoblastic cells, which was compatible with a diagnosis of choriocarcinoma (Fig. 2). Although there were no abnormal findings in the patient's chest X-ray on admission, a CT scan of the chest showed multi-sized multiple nodules in both lungs, and these were all suspected to be hemorrhagic metastases. Her mental status improved gradually, but worsened to stupor 6 days after the initial operation. A brain CT scan demonstrated that the size of the hematoma in the right frontal region had increased. Emergent craniotomy allowed the hematoma and another enhancing mass to be removed. As expected, the histological results for this mass revealed a choriocarcinoma. Her postoperative beta-human chorionic gonadotropin level in serum was above 100000 mIU/mL. Although her condition was improved progressively, she complained of paraplegia and sensory loss below the nipples 2 months after the second operation. Thoracic MRI showed a well-enhancing intramedullary mass from the T3 to the T5 level (Fig. 3). Lumbar MRI revealed a rim-enhancing mass in the L2 vertebral body (Fig. 4). Radiotherapy and multiagent chemotherapy were performed for treatment of the thoracic and lumbar spine lesions, but this could not be continued because of an exacerbation of the patient's general condition and side effects. The patient died from respiratory failure 13 months after the diagnosis.
Choriocarcinoma most often originates in the trophoblastic tissue of a hydatidiform mole but may also originate from the germinal epithelium of the testes, ovaries, or a normal placenta3). Hydatidiform moles are thought to be benign, but choriocarcinomas develop in 1% of these patients3,4). Early, hematogenous, and widespread metastasis is well documented3,7,11). Approximately 30% of patients with choriocarcinoma show metastases at the time of diagnosis12). The favored sites of involvement are the lungs (94% of all metastatic choriocarcinoma), vagina (44%), liver (28%) and brain (28%), followed by the skin, gastrointestinal tract, kidney, breast, and bones3,7,13). While metastasizing within the central nervous system, these tumors are known for their tendency to produce hematoma and intracranial hemorrhages, causing morbidity and mortality in these patients1,13), as in our case.
Choriocarcinoma is one of the malignant tumors most sensitive to chemotherapy11). Patients with a low risk have been treated with single agent methotrexate or dactinomycin, but EMA/CO (etoposide, methotrexate, dactinomycin, cyclosphosphamide, and oncovin) therapy has been considered the most effective treatment regimen for patients with a high-risk2). Remission rates in the nonmetastatic stage of choriocarcinoma are 98% to 100%, and more than 75% even in cases of metastatic choriocarcinoma1,8,9).
The effectiveness of surgical treatment for cerebral metastases has been reported. Surgery is indicated in cases with massive mass effect due to intracerebral hematoma or tumor mass. Use of blood clots biopsy specimens is important for determining the etiology5,13). Suction evacuation of the hematoma may cause loss of material for histopathologic evaluation and may thus miss the opportunity for diagnosis13). It is important to examine the tissue from the wall of the hematoma to exclude a hemorrhagic metastasis13).
The spinal metastasis of choriocarcinoma is very rare. Only 6 cases have been reported (Table 1). Despite improvements in treatment modality, the prognosis for these cases of spinal metastasis is unfavorable. Because these patients generally have a poor outcome within a few weeks after initiating presentation, early recognition and treatment of choriocarcinoma might enable a reduction the mortality rate.
We document an uncommon case of metastatic choriocarcinoma to the lung, brain, lumbar vertebral body and intramedullary spinal cord. This is the first case of intramedullary spinal cord metastasis of choriocarcinoma. Furthermore, the authors emphasize that the possibility of choriocarcinoma should be borne in mind when observing any intracranial hemorrhage in a woman of child-bearing age.
References
1. Athanassiou A, Begent RH, Newlands ES, Parker D, Rustin GJ, Bagshawe KD. Central nervous system metastases of choriocarcinoma. 23 years' experience at Charing Cross Hospital. Cancer. 1983; 52:1728–1735. PMID: 6684500.

2. Bagshawe KD. Treatment of high-risk choriocarcinoma. J Reprod Med. 1984; 29:813–820. PMID: 6097685.
3. Beşkonakli E, Cayli S, Kulaçoğlu S. Metastatic choriocarcinoma in the thoracic extradural space : case report. Spinal Cord. 1998; 36:366–367. PMID: 9601120.

4. Chandra SA, Gilbert EF, Viseskul C, Strother CM, Haning RV, Javid MJ. Neonatal intracranial choriocarcinoma. Arch Pathol Lab Med. 1990; 114:1079–1082. PMID: 2222151.
5. Chang IB, Cho BM, Park SH, Yoon DY, Oh SM. Metastatic choriocarcinoma with multiple neoplastic intracranial microaneurysms : case report. J Neurosurg. 2008; 108:1014–1017. PMID: 18447721.

6. Kuten A, Cohen Y, Tatcher M, Kobrin I, Robinson E. Pregnancy and delivery after successful treatment of epidural metastatic choriocarcinoma. Gynecol Oncol. 1978; 6:464–466. PMID: 738625.

7. Lee JH, Park CW, Chung DH, Kim WK. A case of lumbar metastasis of choriocarcinoma masquerading as an extraosseous extension of vertebral hemangioma. J Korean Neurosurg Soc. 2010; 47:143–147. PMID: 20224716.

8. Lewis JL Jr. Diagnosis and management of gestational trophoblastic disease. Cancer. 1993; 71:1639–1647. PMID: 8381709.

9. Lurain JR. Management of high-risk gestational trophoblastic disease. J Reprod Med. 1998; 43:44–52. PMID: 9475149.
10. Menegaz RA, Resende AD, da Silva CS, Barcelos AC, Murta EF. Metastasis of choriocarcinoma to lumbar and sacral column. Eur J Obstet Gynecol Reprod Biol. 2004; 113:110–113. PMID: 15036724.

11. Naito Y, Akeda K, Kasai Y, Matsumine A, Tabata T, Nagao K, et al. Lumbar metastasis of choriocarcinoma. Spine (Phila Pa 1976). 2009; 34:E538–E543. PMID: 19564760.

12. Sierra-Bergua B, Sánchez-Marteles M, Cabrerizo-García JL, Sanjoaquin-Conde I. Choriocarcinoma with pulmonary and cerebral metastases. Singapore Med J. 2008; 49:e286–e288. PMID: 18946601.
13. Suresh TN, Santosh V, Shastry Kolluri VR, Jayakumar PN, Yasha TC, Mahadevan A, et al. Intracranial haemorrhage resulting from unsuspected choriocarcinoma metastasis. Neurol India. 2001; 49:231–236. PMID: 11593238.
14. Vani R, Kuntal R, Koteshwar RK. Choriocarcinoma following term pregnancy with bone metastasis. Int J Gynaecol Obstet. 1993; 40:252–253. PMID: 8096480.

Fig. 1
Preoperative brain MRI scan showing a hematoma in the left temporo-parietal region and two enhancing nodular lesions in the right frontal and left temporal regions.
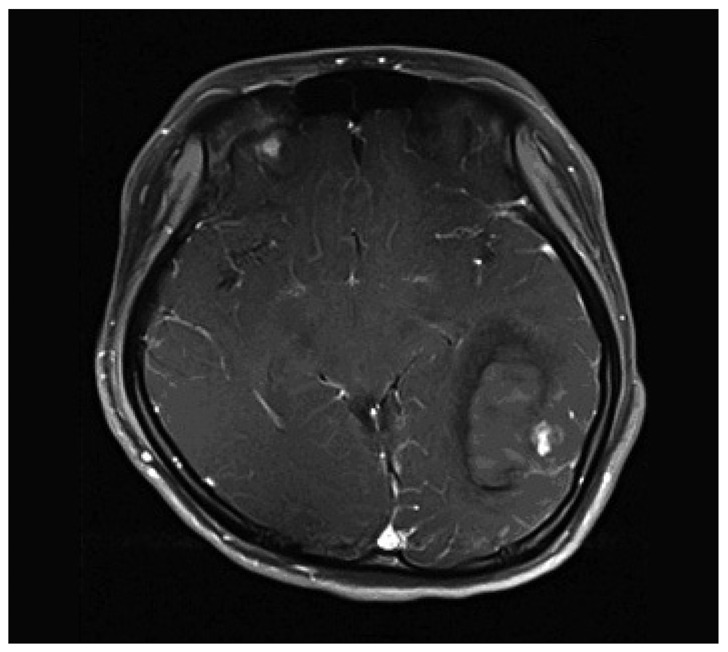
Fig. 2
Histologic section of the enhancing mass showing trophoblastic cells (H&E, original magnification ×200).

Fig. 3
A : Sagittal T2-weighted MRI of the thoracic spine, showing the edematous swelling of the spinal cord. B : Axial T2-weighted MRI showing an intramedullary high-signal intensity lesion. C : Sagittal T1-weighted MRI obtained after Gd injection. The tumor appears heterogeneously hyperintense. D : Axial Gd-enhanced T1-weighted MRI showing a well-enhancing intramedullary mass.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download