Abstract
Aneurysmal bone cyst (ABC) is benign vascular lesion destructing the cortical bone by the expansion of the vascular channel in the diploic space that usually involve long bone and spine. Orbital ABC is rare and the clinical symptoms deteriorate rapidly after initial slow-progression period for a few months. A 12-year-old female patient visited ophthalmologist due to proptosis and upward gaze limitation of the right eye, and orbital mass was noted in the upper part of right eye on orbital MRI. Five months later, exophthalmos was worsened rapidly with other features of ophthalmoplegia. Orbital mass was enlarged on MRI with intracranial extension. Surgery was done through frontal craniotomy and intracranial portion of the tumor was removed. Destructed orbital roof and mass in the orbit was also removed, and surrounding bone which was suspected to have lesion was resected as much as possible. Histopathological diagnosis was aneurysmal bone cyst. Postoperative course was satisfactory and the patient's eye symptoms improved. Authors report a rare case of orbital ABC with review of the literature. Exact diagnosis by imaging studies is important and it is recommended to perform surgical resection before rapid-progressing period and to resect the mass completely to prevent recurrence.
Aneurysmal bone cyst (ABC) is the rare, benign, vascular, multicystic lesion of the bone with unknown origin that usually involves the long bone and spine4,11). Venous channel in the diploic space is enlarged, which caused destruction of the cortical bone. About 20% of ABC occurs at the spine, but rarely in the cranium with the incidence of 1 to 6%5,11,19). If it involves the cranium, cranial vault is the most frequent site. Orbital ABC has been reported only 25 cases to our knowledge1,4,11,12,14,15,19,24).
Clinical symptoms and signs of orbital ABC is similar to those of other orbital mass, and radiological diagnosis can be made with computed tomographic (CT) images and magnetic resonance (MR) images, and plain films. After initial symptoms and signs noted, it progress slowly for a few months, followed by rapid-deterioration. The proper management is complete surgical excision, and any remnant lesion is the causes of recurrence. ABC is highly vascular tumor and attention should be paid to the excessive blood loss during surgery11-13).
Authors experienced a rare case of orbital ABC with intracranial extension, which was treated by surgical intervention and present its clinical, pathological, and radiological characteristics with literature review.
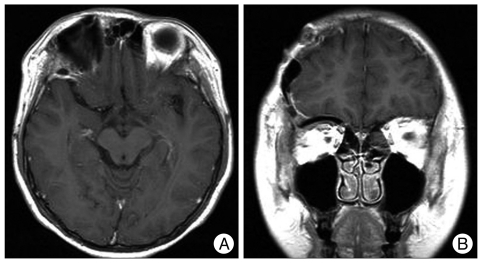
A 12-year-old female patient presented to the ophthalmic clinic with mild proptosis, limitation of extraocular muscle movement (EOM), and inferior eyeball deviation of the right eye. There was no relevant past history such as head injury. MR images showed a multiloculated mass, about 2.5×2.4 centimeter in the upper part of right eye which compressed right eyeball. The cyst was showed low-signal intensity on T1-weighted image (T1WI), and iso-signal intensity on T2-weighted image and flair image. Cystic wall was enhanced strongly after injection of Gd-DTPA (gadolinium enhancement) (Fig. 1). Under the impression of venous anomaly, conservative care was followed.
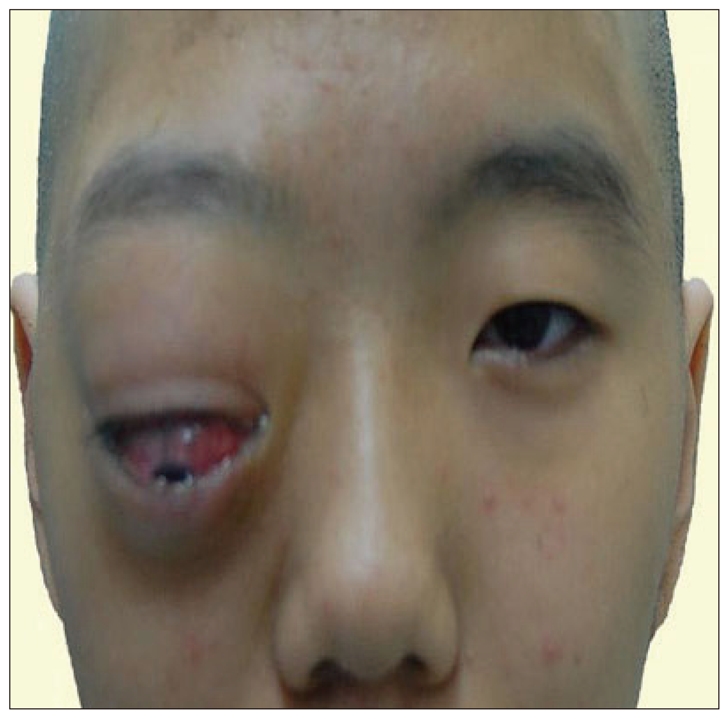
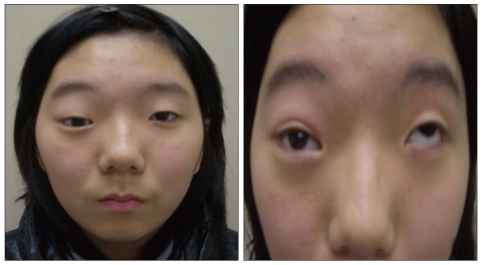
Five months later, exophthalmos progressed rapidly with conjuctival ecchymosis, limitation of EOM, and downward eyeball deviation, and she was refered to neurosurgery department. Examination revealed a marked non-pulsatile exopthalmos with double vision in all directions. Right eyeball was fixed in downward gaze state and visual acuity was 20/200 (Fig. 2).
Plain films of the skull showed radiolucent lesion in the orbital roof of right eye that was surrounded by thin marginal shell of sclerotic cortical bone (Fig. 3A). Brain CT revealed a expansive osseous lesion that was multiloculated with peripheral enhancement. Both inner and outer tables were thinned, but their integrity was preserved (Fig. 3B).
Brain MR images showed a enlarged mass, about 4.4×4.0 centimeter which extended superior to frontal lobe and inferior to right eyeball with compression. A well-circumscribed multicystic mass with peripheral hypointense capsule and internal hypointense septation on T1WI. T2-weighted MR images showed multilobulated mass with iso-signal intensity. The cystic cavities were filled with heterogenous, but hyperintense hemorrhagic fluid-fluid levels on all sequence. Cystic wall was enhanced strongly after injection of Gd-DTPA (Fig. 3C, D).
Operation was done by frontal craniotomy. The dura of the frontal base was detached off the orbital roof which was tumor itself, was destructed severely, and was extended intracranially. The mass was entirely extradural in nature. The tumor showed high vascularity and bone was destructed severely. Orbital mass was removed completely, and resection was continued more deeply into the optic foramen. It was removed totally under the surgical microscope with special attention to preserve the optic nerve. Bony margins, which was suspected portion to have the pathological change, were also totally resected. Macroscopically, the tumor was cystic, hemorrhagic appearance in some areas. After removing the tumor, orbital roof was reconstructed using Codman Cranioplastic kits®, Leibinger plate®, and PolyBone®.
The patient refused transfusion because of the religious reason, the surgery was planned according to the "bloodless surgery" manual. During surgery, Cell Saver® (Autologous Blood Recovery System) was used to collect the blood in operating field. The autologous blood transfusion was delivered during surgery, and any surgical bleeding was controlled immediately, using electrical coagulator and bone wax, and surgical procedures was performed as fast as possible.
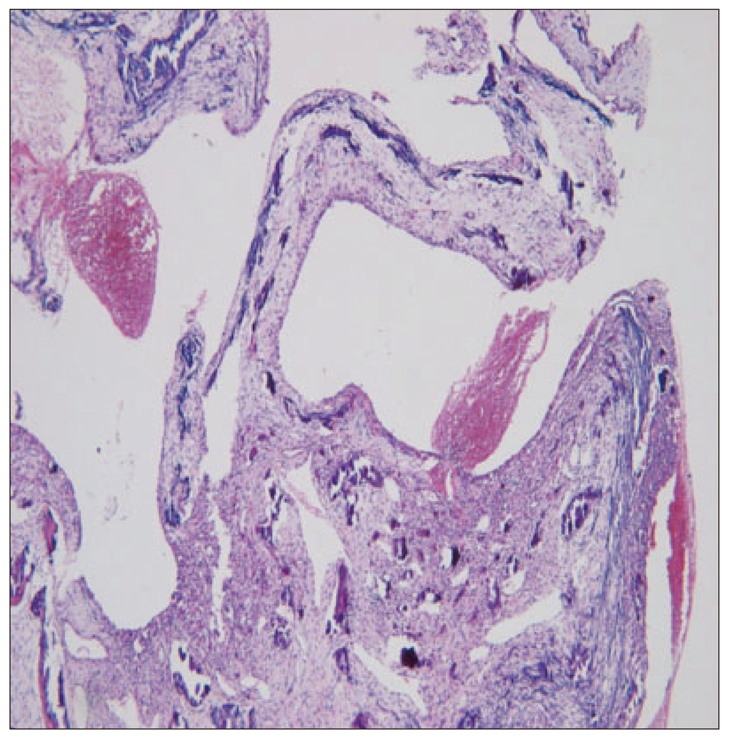
As for pathologic findings, blood-containing cystic spaces were separated by fibroblasts and reactive bone formation was also discovered. These led to the confirming diagnosis of ABC (Fig. 4).
Postoperatively, clinical symptoms and signs were greatly improved. Exophthalmos was subsided, limitation of EOM was restored, and visual acuity improved to 20/33 on 14 days after the operation. Follow-up MR image taken 7 months after the operation revealed no evidence of mass in the orbit (Fig. 5). At the 13 months after the surgical resection, mild downward eyeball deviation was remained, and diplopia was presented on left lateral gaze with minimal disturbance of eye motions on medical and upward gaze (Fig. 6).
Aneurysmal bone cyst causes lytic changes in the diploic space of bone, filled with products of blood components, destructing cortical bone11-14). In 1942, Jaffe and Lichitenstein first described the term ABC as "peculiar blood-containing cysts of large size"13). Most of ABC involve the metaphysis of the long bone, such as a femur, and one-fifth of ABC involve the spine3,5-7). Only 1 to 6% of the cases was reported to occur in the cranial bone4,11,19). In up to 85% of cases, it occurs at the age of 20 or less, a mean age of 13. It shows the female predominance slightly10,12).
In ABC, the cortical bone is expanded and destructed by the venous channel with increased pressure in the diploic space, even though the precise nature and origin of ABC is unclear13). ABC is defined as a distinct entity, classified into primary or secondary according to the presence or absence of an associated lesion, such as giant cell tumor, chondroblastoma, osteoblastoma, osteosarcoma, chondromyxoid fibroma, and fibrous dysplasia2,13,14,18). It causes local hemodynamic disturbance, like arterio-venous shunts or malformations, which would increase venous pressure. These lead the subsequent bony resorption and destruction of the vascular bed, which would form ABC eventually11).
The first cranial ABC was reported by Odeku and Mainwaring in 1965, which occurred in occipital bone, presenting painful swelling on occipital area. Surgical resection was attempted, but the patient died of cardiac arrest unfortunately. In the cranium, the vault is the frequent site for ABC, but the sphenoid, ethmoid, and orbit are rarely involved. Cranial ABC causes destruction of both inner and outer table of the skull, resulting in painful or painless mass by external expansion and neurological symptoms by compressing the brain or cranial nerve4,11,16,18).
The first ABC involving the orbit was reported by Fite DJ et al. in 19684). Eight-year-old female patient was presented with exophthalmos of the right eye, which was treated by total tumor resection. Thereafter, orbital involvement was reported in 25 cases1,4,11,12,14,15,19,24). Among these 25 cases, orbital roof was involved in 19 cases, and medial wall was involved in 4 cases, lateral wall 2 cases. Exophthalmos is noted in all cases, and diplopia in 7 cases, decreased vision in 6 cases. The symptoms of increased intracranial pressure was noted in 3 cases. Tumor was removed totally in 19 cases and recurrence was noted in 2 of 19 (10.52%). Subtotal resection was performed in 5 of 25 orbital ABCs, and tumor recurred in all cases. In author's case, tumor was resected totally and recurrence was not noted at 13 months after surgery4,11,14,18).
After initial diagnosis, the progression of ABC is gradual in the first several months, followed by rapid clinical deterioration12). Of the 25 cases of orbital ABC, period of initial slow-progression was average 14 weeks (8 days to 6 months), and then clinical symptoms and signs deteriorated rapidly, causing painful exophthalmos, ptosis, diplopia, limitation of EOM and decreased vision by compressing on the orbital contents such as extraocular muscles, optic and oculomotor nerve. Many patients consulted the doctor during the phase of rapid growth. In most cases, ABC extended into the intracranial space, compressing the frontal lobe. This suggests the importance of early treatment before neurological deficit develops4,11-13).
In the diagnosis of ABC, imaging studies are important. Aneurysmal bone cyst was named according to the features of plain skull films, that is single or multiple blown-out lytic lesion. The lytic lesion is surrounded by a thin marginal shell of sclerotic cortical bone4,8). On the computed tomography of brain, it appears as an expansive multioculated osseous lesion with the enhancement on peripheral capsule and internal septation of lesion after intravenous contrast11,12,18).
Magnetic resonance imaging of ABC reveals the characteristic appearance of the lesions. The lesions may be surrounded by a fibrous capsule with hypointense signal intensity on all sequences. And, they may have internal septations with hypointense signal intensity, separating multiple cystic components2,11,15,22,23). If associated fibro-osseous lesions are shown on CT and/or MRI, the diagnosis of ABC should be strongly suspected11). Angiographic features can sometimes reveal the blood supply to these vascular lesions and may also occasionally reveal arteriovenous shunts.
Gross pathological evaluation typically shows an ABC to be composed of individual cysts filled with unclotted liquid blood and blood-tinged serous fluid. Microscopically, ABC appears as blood-filled cavernous spaces with a paucity of endothelial cells. The cysts are seperated by septa composed of fibrous tissue which contains multinucleated giants cells and possibly osteoid tissue2,8,17,19).
Total surgical excision is the treatment of choice in the management of ABC, and any remnant lesion is the reason of recurrence. The recurrence rate after total excision is known to be 10 to 20%. It is related to the age of the patient, size of the lesion, the presence of mitosis, and more importantly, the incompleteness of the resection2,5,9,13,19). In the cranium and the spine, there is also an added difficulty in that it is often impossible to reach and excise the lesion completely. This is especially true if the lesion is located in the skull base, for example in the roof, the medial and lateral walls of the orbit, the paranasal sinuses, and the petrous temporal bone. In these cases, partial excision or intralesional curettage with adjunctive therapy such as preoperative embolization or postoperative radiotherapy or stereotactic radiosurgery should be considered2,5,8,11,20,21). Also, ABC is highly vascular tumor and special attention should be paid to the possible excessive blood loss during surgery, and preoperative embolization may be helpful to prevent blood loss.
In conclusion, ABC is rare benign vascular lesion of bone that can occur very rarely in the orbit. It may cause local swelling of bone and surrounding tissue as well as symptoms including diplopia, limitation of EOM, and headache. Authors report a rare case of ABC involving the orbit, which was treated by surgical excision with good result.
References
1. Borkar SA, Kasliwal MK, Sinha S, Sharma BS. MR imaging in aneurysmal bone cyst of the orbit. Turk Neurosurg. 2008; 18:183–186. PMID: 18597234.
2. Bozbuğa M, Turan Süslü H. Aneurysmal bone cyst of the sphenoid bone extending into the ethmoid sinus, nasal cavity and orbita in a child. Turk Neurosurg. 2009; 19:172–176. PMID: 19431130.
3. Bush CH, Drane WE. Treatment of an aneurysmal bone cyst of the spine by radionuclide ablation. AJNR Am J Neuroradiol. 2000; 21:592–594. PMID: 10730658.
4. Cakirer S, Cakirer D, Kabukcuoglu F. Aneurysmal bone cyst of the orbit : a case of rare location and review of the literature. Clin Imaging. 2002; 26:386–391. PMID: 12427433.
5. Capote-Moreno A, Acero J, García-Recuero I, Ruiz J, Serrano R, de Paz V. Giant aneurysmal bone cyst of the mandible with unusual presentation. Med Oral Patol Oral Cir Bucal. 2009; 14:E137–E140. PMID: 19242394.
6. Chan G, Arkader A, Kleposki R, Dormans JP. Case report : primary aneurysmal bone cyst of the epiphysis. Clin Orthop Relat Res. 2010; 468:1168–1172. PMID: 20107940.
7. Chen SH, Huang TJ, Hsueh S, Lee YY, Hsu RWW. Unusual bleeding of aneurysmal bone cyst in the upper thoracic spine. Chang Gung Med J. 2002; 25:183–188. PMID: 12022739.
8. Chidambaram B, Santosh V, Balasubramaniam V. Aneurysmal bone cyst of the temporal bone. Childs Nerv Syst. 2001; 17:411–414. PMID: 11465795.

9. Docquier PL, Delloye C, Galant C. Histology can be predictive of the clinical course of a primary aneurysmal bone cyst. Arch Orthop Trauma Surg. 2010; 130:481–487. PMID: 19430802.

10. Errani C, Schuster S, Biagini R, Casadei R, De Paolis M, Bertoni F, et al. Reconstruction with fascia lata allograft of the posterior vertebra elements after resection for aneurysmal bone cyst in a child. Eur Spine J. 2007; 16:1531–1535. PMID: 17426986.

11. Gan YC, Hockley AD. Aneurysmal bone cysts of the cranium in children. Report of three cases and brief review of the literature. J Neurosurg. 2007; 106:401–406. PMID: 17566211.
12. Hunter JV, Yokoyama C, Moseley IF, Wright JE. Aneurysmal bone cyst of the sphenoid with orbital involvement. Br J Ophthalmol. 1990; 74:505–508. PMID: 2202437.

13. Kransdorf MJ, Sweet DE. Aneurysmal bone cyst : concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995; 164:573–580. PMID: 7863874.

14. Marback EF, Neves M, Marback RL. [Aneurysmal bone cyst of the orbit - a clinicopathological study : case report]. Arq Bras Oftalmol. 2008; 71:868–870. PMID: 19169523.
15. Marcol W, Mandera M, Malinowska I, Pajak J, Właszczuk P, Kluczewska E. Aneurysmal bone cyst of the orbit. Pediatr Neurosurg. 2006; 42:325–327. PMID: 16902348.

16. Nadkarni T, Goel A, Desai K, Aiyer P, Shenoy A. Massive aneurysmal bone cyst of the anterior cranial fossa floor--case report. Neurol Med Chir (Tokyo). 2001; 41:615–619. PMID: 11803589.

17. Peeters SP, Van der Geest IC, de Rooy JW, Veth RP, Schreuder HW. Aneurysmal bone cyst : the role of cryosurgery as local adjuvant treatment. J Surg Oncol. 2009; 100:719–724. PMID: 19821494.

18. Rai AT, Collins JJ. Percutaneous treatment of pediatric aneurysmal bone cyst at C1 : a minimally invasive alternative : a case report. AJNR Am J Neuroradiol. 2005; 26:30–33. PMID: 15661694.
19. Senol U, Karaali K, Akyüz M, Gelen T, Tuncer R, Lüleci E. Aneurysmal bone cyst of the orbit. AJNR Am J Neuroradiol. 2002; 23:319–321. PMID: 11847063.
20. Sun ZJ, Sun HL, Yang RL, Zwahlen RA, Zhao YF. Aneurysmal bone cysts of the jaws. Int J Surg Pathol. 2009; 17:311–322. PMID: 19233862.
21. Sun ZJ, Zhao YF, Yang RL, Zwahlen RA. Aneurysmal bone cysts of the jaws : analysis of 17 cases. J Oral Maxillofac Surg. 2010; 68:2122–2128. PMID: 20110147.
22. Tang IP, Shashinder S, Loganathan A, Anura MM, Zakarya S, Mun KS. Aneurysmal bone cyst of the maxilla. Singapore Med J. 2009; 50:e326–e328. PMID: 19787162.
23. Theron S, Steyn F. Clinical image. An unusual cause of proptosis aneurysmal bone cyst of the anterior skull base. Pediatr Radiol. 2006; 36:997. PMID: 16767401.

Fig. 1
Initial Orbit magnetic resonance images. Inhomogenously-enhancing mass is noted in the right superior orbital area, compressing eyeball. T1-weighted image axial (A) and coronal images (B).
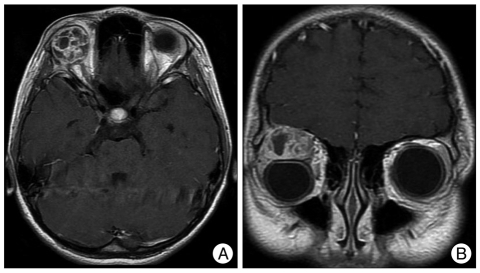
Fig. 3
Marked osteolytic changes are noted in orbital roof on plain film (A), CT (B). Brain MRI (enhanced) shows inferior and superior extension of the large multi-lobulated enhanced mass within homogenous fluid level in right orbit upper portion and intracranial portion compressing the frontal lobe and eyeball (C and D).
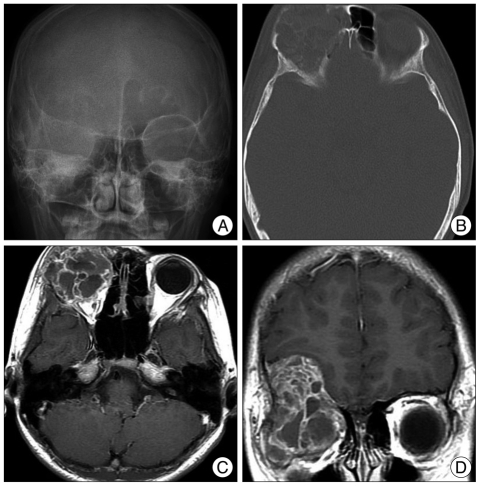
Fig. 4
Histopathological examinatin shows hemorrhagic cystic spaces and connective tissue with fibroblasts, osteoclast-type giant cells and woven bone was seen (H&E, ×100).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download