Abstract
Purpose
There are few reports on outcomes following surgical repair of recurrent rectal prolapse. The purpose of this study was to examine surgical outcomes for recurrent rectal prolapse.
Methods
We conducted a multicenter retrospective study of patients who underwent surgery for recurrent rectal prolapse. This study used data collected by the Korean Anorectal Physiology and Pelvic Floor Disorder Study Group.
Results
A total of 166 patients who underwent surgery for recurrent rectal prolapse were registered retrospectively between 2011 and 2016 in 8 referral hospitals. Among them, 153 patients were finally enrolled, excluding 13 patients who were not followed up postoperatively. Median follow-up duration was 40 months (range, 0.2–129.3 months). Methods of surgical repair for recurrent rectal prolapse included perineal approach (n = 96) and abdominal approach (n = 57). Postoperative complications occurred in 16 patients (10.5%). There was no significant difference in complication rate between perineal and abdominal approach groups. While patients who underwent the perineal approach were older and more fragile, patients who underwent the abdominal approach had longer operation time and admission days (P < 0.05). Overall, 29 patients (19.0%) showed re-recurrence after surgery. Among variables, none affected the re-recurrence.
Conclusion
For the recurrent rectal prolapse, the perineal approach is used for the old and fragile patients. The postoperative complications and re-recurrence rate between perineal and abdominal approach were not different significantly. No factor including surgical method affected re-recurrence for recurrent rectal prolapse.
Rectal prolapse occurs when a mucosal or full-thickness layer of rectal tissue protrudes through the anal orifice. Problems with this condition include constipation, fecal incontinence, mucous discharge, and rectal bleeding [1]. Most rectal prolapse can be treated successfully with surgical procedures. While much data have been obtained on the treatment strategy for primary rectal prolapse, little is known about clinical outcomes of recurrent disease. Only 6 case series solely dealing with recurrent rectal prolapse have been published [234567]. All these studies were performed before 2006.
Surgical approaches for rectal prolapse can be divided into perineal and abdominal approaches. Traditionally, a perineal procedure such as Delorme or Altemeir operation was commonly used in elderly or frail patients while an abdominal procedure such as rectopexy with or without resection was reserved for younger and fitter patients [89]. The frequency of laparoscopic abdominal repair of rectal prolapse has increased in recent years, with ventral mesh rectopexy being the most popular procedure [1011]. Two recent randomized clinical trials did not show any difference in morbidity, recurrence rate, or quality of life score between the abdominal procedure and the perineal procedure [1213]. Based on these data, this study investigated recent clinical outcomes of surgical management comparing perineal and abdominal approaches for recurrent rectal prolapse.
The study was performed under the Korean Anorectal Physiology and Pelvic Floor Disorder Study Group. Data of individual patients from 8 institutes of Korea from 2011 to 2016 were collected. This study was approved by the Institutional Review Board (IRB) of Korea University Ansan Hospital (No. AS17181-001). The IRB granted a waiver of informed consent. It was further endorsed by each participating institute. Inclusion criteria for data were: (1) patients with age of ≥18 years; and (2) those with evidence of recurrent rectal prolapse (defined as reappearance of external full-thickness prolapse after previous surgery for rectal prolapse) at baseline assessment. Patients who had their previous rectal prolapse surgery performed inside or outside each institution were included. Patients who were lost without follow-up after surgery were excluded from this study.
External full-thickness prolapse was diagnosed by concentric folds of prolapsed tissues. In each center, initial evaluation of a patient with a rectal prolapse included a complete history and physical examination with a focus on the prolapse. Additional testing such as defecography, anal manometry, colonoscopy, and endoanal sonography might be used selectively to refine the diagnosis and identify other coexisting pathologies. Three experts (Hong KD, Lee D, and Joh YG) in this study group determined whether enrolled patients had definite recurrent rectal prolapse based on clinical manifestations at each center.
Variables including age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status (PS) classification, number and type of previous operation for rectal prolapse, and methods of surgical repair for recurrent rectal prolapse were analyzed. Operative methods were divided into abdominal and perineal approaches. The abdominal approach included posterior suture rectopexy, posterior mesh rectopexy, posterolateral mesh rectopexy, ventral mesh rectopexy, and resection rectopexy [1014151617]. For rectal mobilization, a posterior suture rectopexy and a posterior mesh rectopexy were performed using a circular mesorectal dissection down to pelvic diaphragm. However, a posterolateral mesh rectopexy involved dissection in the posterior and only right lateral mesorectum of the rectum to lessen autonomic nerve injury [16]. In ventral mesh rectopexy, no rectal mobilization or lateral dissection was performed. Mesh was sutured to the ventral aspect of the distal rectum [10]. Posterior suture rectopexy was similar to posterior mesh rectopexy except that it did not use mesh to pull the rectum in a cranial direction [17]. All meshes used were made of polypropylene materials. Perineal approach included Delorme procedure, Thiersch procedure, Delorme with Thiersch procedure, and Altemeir procedure [1819202122]. With a Thiersch procedure, a non-absorbable suture material was placed circumferentially around the anus, allowing an index finger to pass through [22]. The Delorme with Thiersch procedure was mainly performed in Song Do Hospital (Seoul, Korea) [20]. After the Delorme procedure, a polyester tape (Cervix set, B Braun, S.A., Rubí, Spain) was brought through the tunnel around the external anal sphincter to encircle the anal canal. All procedures were chosen according to the preference of each institution or the surgeon. Outcome data included operation time, length of postoperative hospital stay, 30-day postoperative complications, 30-day mortality, and re-recurrence. Complications were limited to cases having grade II or higher according to the Clavien-Dindo classification [23]. Re-recurrence was defined as reappearance of external full-thickness prolapse after surgery. Follow-up was conducted by office visit or phone survey.
Patients were divided into 2 groups according to the method of surgical repair for recurrent rectal prolapse. Clinicopathologic outcomes were compared between the 2 groups. Wilcoxon and Mann-Whitney U-tests were used for comparison of quantitative variables. Fisher exact test was used for categorical variables. To find the impact of an independent variable on re-recurrence, logistic regression analysis was performed. Time to re-recurrence was analyzed using the Kaplan-Meier estimator and groups were compared by Cox proportional hazards to competing events [24]. All statistical analyses were performed with IBM SPSS Statistics ver. 20.0 (IBM Corp., Armonk, NY, USA). A P-value of <0.05 was considered statistically significant.
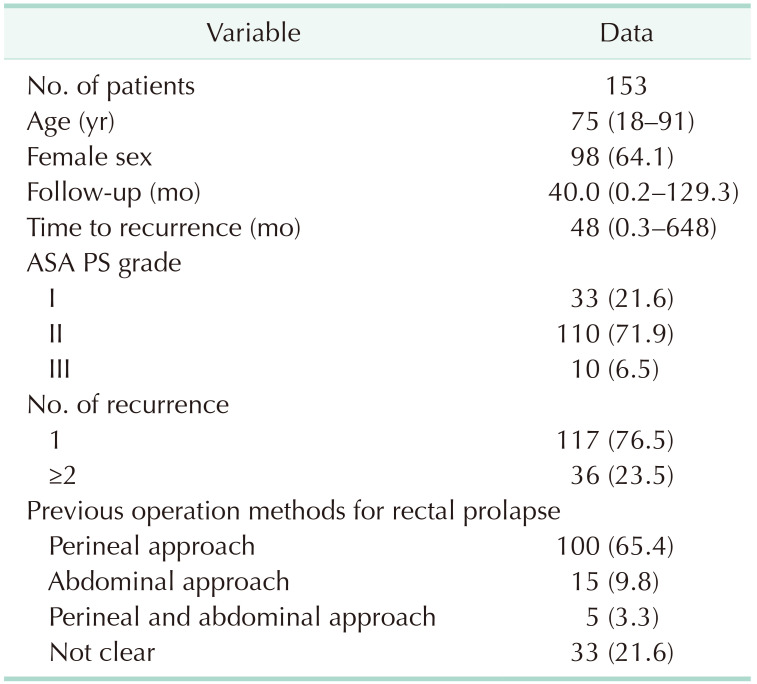
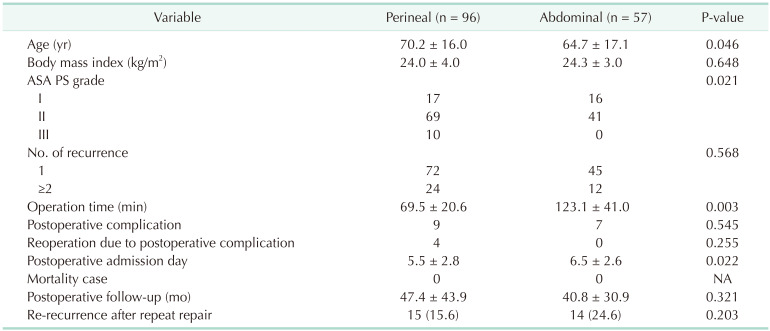
From 2011 to 2016, 166 surgically treated patients were identified in 8 institutes in Korea. These institutes were tertiary university hospitals or specialized colorectal centers. The number of cases at each institute was as follows: Song Do Hospital, 90; Daehang Hospital, 40; Hansol Hospital, 20; Korea University Anam Hospital, 5; Seoul National University Hospital, 4; Korea University Guro Hospital, 3; Korea University Ansan Hospital, 3; and Seoul National University Bundang Hospital, 1. Among them, 13 patients were not followed up after operation. Thus, 153 patients were finally enrolled. Of these patients, 98 (64.1%) were female. Median follow-up duration was 40.0 months (range, 0.2–129.3 months). Median age was 75 years (range, 18–91 years). One hundred and seventeen patients (76.5%) experienced the first recurrence. Twenty-six patients (17.0%) experienced second recurrence and 10 patients (6.5%) had more than 3 recurrence events. Median time to recurrence was 48 months (range, 0.3–648 months) (Table 1).
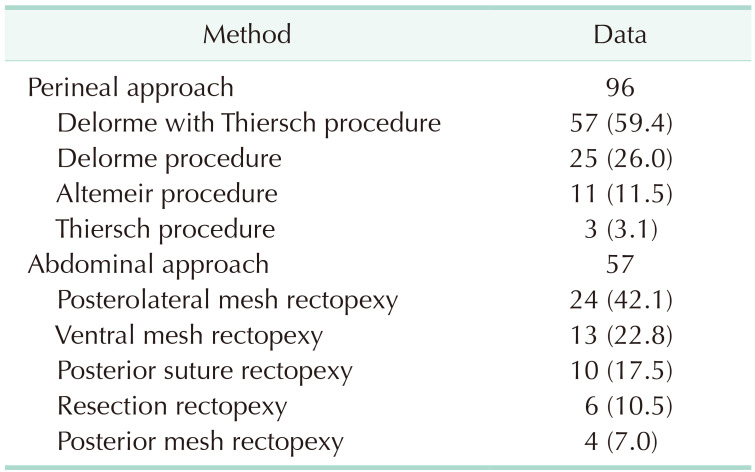
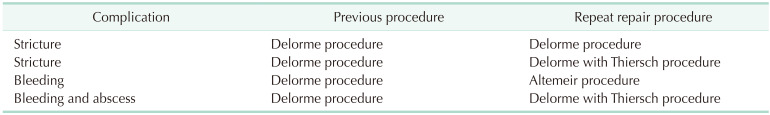
A total of 153 patients underwent surgery for recurrent rectal prolapse. The method of surgical repair for recurrent rectal prolapse included the perineal approach (96 patients, 62.7%) and the abdominal approach (57 patients, 37.3%). Among the 96 patients who underwent the perineal approach for recurrent rectal prolapse, Delorme with the Thiersch procedure (57 patients, 59.4%) was the most common procedure. Among the 57 patients who underwent the abdominal approach for recurrent rectal prolapse, posterolateral mesh rectopexy (24 patients, 42.1%) was the most common procedure (Table 2). The abdominal approach was mostly performed laparoscopically (55 patients, 96.5%). Patients who underwent the perineal approach were statistically older with higher ASA PS grade than patients who underwent the abdominal approach for recurrent rectal prolapse. Although postoperative complications showed no significant difference, operation time and postoperative hospital stay were statistically longer for patients who underwent the abdominal approach (Table 3). Overall, 16 patients (10.5%) had 30-day postoperative complications. The most common complication was wound infection (5 patients), followed by urinary retention (4 patients), operation site bleeding (2 patients), anal stricture (2 patients), incisional hernia (2 patients), and ileus (1 patient). There were 4 reoperation cases due to postoperative complications such as stricture, infection by suture material, and bleeding. These cases occurred only in patients who received the perineal approach for both previous and recurrent rectal prolapse. There was no mortality case (Table 4). There were 17 patients who underwent rectal resection procedures through perineal or abdominal approach for recurrent rectal prolapse. Among the 11 patients who underwent the Altemeir procedure for recurrent rectal prolapse, no patient had received resection rectopexy for a previous rectal prolapse. In contrast, among the 6 patients who underwent resection rectopexy for recurrent rectal prolapse, 1 patient had received the Altemeir procedure for a previous rectal prolapse. That patient had no postoperative complication.
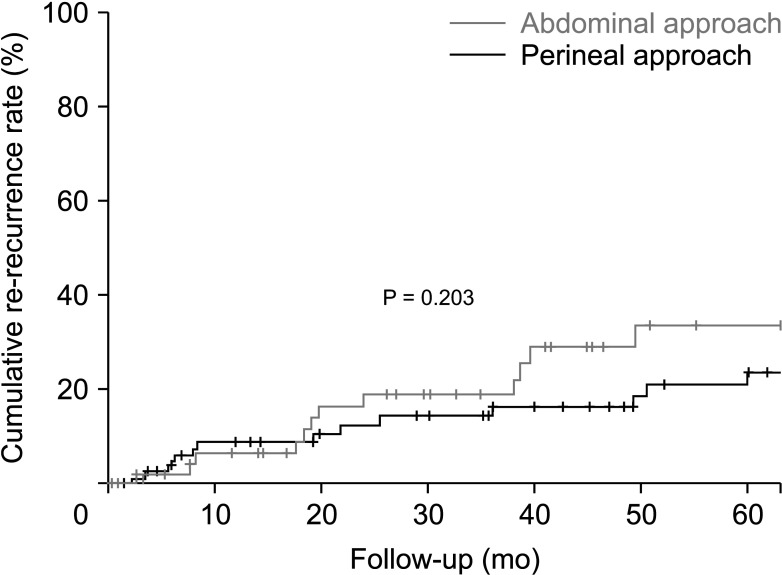
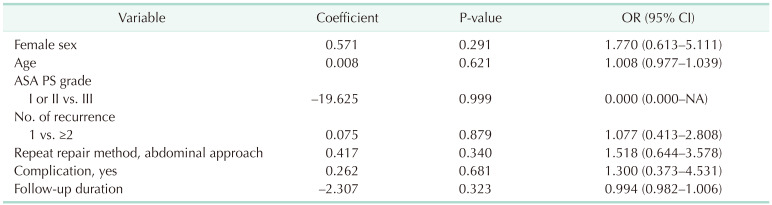
Re-recurrence of rectal prolapse after surgery occurred in 29 patients (19.0%). Median time to re-recurrence after surgery was 21.9 months (range, 2.4–97.3 months). Nine cases of re-recurrence (31.0%) occurred within 1 year of recurrent repair operation. Logistic regression analysis was performed to determine the impact of independent variables on re-recurrence. Among variables, none was related to re-recurrence (Table 5). The relationship between surgery and previous surgical methods was also investigated. It was found that the repair method was not related to the re-recurrence rate (P = 0.839) (Fig. 1). The Kaplan-Meier curve did not show any significant difference in re-recurrence rate between the 2 approaches for recurrent rectal prolapse (P = 0.203) (Fig. 2).
Unlike with primary rectal prolapse, there is no appropriate surgical guideline for recurrent rectal prolapse. There might be several reasons for the lack of surgical guidelines. First, few studies have investigated recurrent rectal prolapse. Second, various surgical methods have been performed for recurrent rectal prolapse. Third, only single-center studies with a limited number of patients have been conducted. The current study represents the largest one to date on surgical outcomes for recurrent rectal prolapse through multicenter research based on recent data.
When we divided the surgical approach into perineal and abdominal approaches, the perineal approach was found to be 1.68 times more frequently performed in patients with recurrent rectal prolapse. Although most abdominal approach surgeries were performed with laparoscopic surgery (96.5%), elderly and fragile patients were still receiving the perineal approach more often than the abdominal approach. This finding is in line with a systematic review by Hotouras et al. [9] showing that the traditional idea that older or high-risk patients should be offered the perineal approach cannot currently be challenged in the laparoscopic era. Among perineal approaches, Delorme with and without Thiersch procedures were the most commonly performed ones (82 patients, 85.4%). Among abdominal approaches, rectopexy was the most often performed one laparoscopically without bowel resection (51 patients, 89.5%). The Delorme procedure is simpler with less surgical risk than the Altemeir procedure because it only uses mucosal striping without rectal resection [1925]. Furthermore, to treat the associated lax anal sphincter, a Thiersch suture can be placed concomitantly with the Delorme procedure. Warwick et al. [26] reported that complications were not increased after placement of a Thiersch suture with the Delorme procedure and that recurrence rate could be potentially decreased with this combined technique. Likewise, laparoscopic rectopexy without bowel resection is simpler without having the risk of anastomotic leak compared with resection rectopexy. Considering these findings, in the clinic, less invasive surgical methods were applied to patients with recurrent rectal prolapse.
We found that the re-recurrence rate after surgery for recurrent rectal prolapse was 19.0% with a median follow-up duration of 40.0 months (range, 0.2–129.3 months). This finding was similar to other studies showing re-recurrence rate of 0% to 39.1% during a follow-up period of 9 to 60 months [2345152527]. However, because these studies had small sample sizes, different surgical procedures, and various follow-up periods, care should be taken when comparing these rates. No study has investigated factors influencing re-recurrence after surgery for recurrent rectal prolapse yet. We analyzed causal factors that might influence re-recurrence after surgery for recurrent rectal prolapse. When confounding factors were controlled by logistic regression analysis, no factor was related to re-recurrence. Twenty-nine patients developed re-recurrence, with Kaplan-Meier curve estimates of 5.9%, 11.8%, and 16.3% after 1, 3, and 5 years, respectively. Because a short length of follow-up can lead to underestimation of the actual re-recurrence rate, further study with a longer term follow-up needs to be performed. Interestingly, the type of surgery (perineal or abdominal approach) for recurrent rectal prolapse did not affect the re-recurrence rate or the complication rate in this study. Until now, only 1 study has compared outcomes of perineal and abdominal approaches for recurrent rectal prolapse [4]. Although there was no significant difference in postoperative complications between the 2 approaches in a previous report, there were significantly more re-recurrences after surgery using a perineal approach (37.3%) compared with an abdominal approach (14.8%) for recurrent rectal prolapse [4]. However, the perineal approach was more frequently performed in older patients, which was not controlled with other confounding factors influencing the re-recurrence rate with a statistical method. Although no further study had compared perineal and abdominal approaches, some studies suggested that the type of surgery should be chosen according to the previous surgery for rectal prolapse. Fengler et al. [2] have suggested that repeat resectional procedures such as resection rectopexy following the Altemeir procedure or vice versa might result in complications attributable to ischemia in intervening segments between anastomoses. Hence, the authors recommended that a nonresectional surgery such as the Delorme procedure should be considered in recurrent rectal prolapse if a resectional procedure was previously performed. To avoid this problem, Pikarsky et al. [5] and Ding et al. [27] have recommended the Altemeir procedure for recurrent rectal prolapse because it can be successfully performed in patients who have previously received the Altemier procedure for rectal prolapse. The reason might be that the previous anastomotic line can be easily identified in the anal canal. Additionally, it is difficult to perform an abdominal approach because tissue planes are lost with little tissue to perform the rectopexy. Among 9 patients who underwent Altemeir as a previous surgery for rectal prolapse in this study, 1 patient following resection rectopexy and 2 patients following the Altemeir procedure for recurrent rectal prolapse had no postoperative complications or re-recurrence. Among the 5 patients who underwent resection rectopexy as a previous surgery for rectal prolapse in this study, only 1 patient received the abdominal approach (rectopexy without resection) and showed no complication or re-recurrence. With respect to other authors’ concerns, these findings indicated good results, although the number of cases was small. In this study, there was no significant difference in complication rate between the perineal and abdominal approaches. However, 4 reoperation cases due to complications occurred only when the perineal approach was used for recurrence after the Delorme procedure. Although Javed et al. [25] have suggested that repeated peritoneal approaches can be safe after failed Delorme procedures, their study only included 8 cases (Delorme, 3 cases and Altemeir, 5 cases). Our results indicate that repeated handling of the rectum through the anal canal, albeit via a nonresectional procedure, can jeopardize the viability of rectal tissue.
This study had some limitations. First, it was retrospective in nature. Second, the 2 patient groups, perineal and abdominal approach groups for recurrent rectal prolapse, were not completely comparable. Thus, further studies are required to validate our conclusions. Third, the operative approach was at the discretion of each institution or individual surgeon. Although a multicenter research was performed to produce universal results, selection bias might have affected our results. Such bias may explain why patients who underwent a perineal approach were older with higher ASA PS grades than those who underwent the abdominal approach for recurrent rectal prolapse. Lastly, we did not present changes in functional outcome after surgery for recurrent rectal prolapse. Because most institutes did not use a validated questionnaire for constipation or fecal incontinence, it was impossible to summarize those results.
For the recurrent rectal prolapse, the perineal approach is used for the old and fragile patients. The postoperative complications and re-recurrence rate between perineal and abdominal approach were not different significantly. No factor including surgical method affected re-recurrence for recurrent rectal prolapse.
Notes
This study was previously presented as an oral presentation at the meeting of The 27th Seoul Coloproctology Course, Seoul, Korea on November 7, 2021.
References
1. Bordeianou L, Hicks CW, Kaiser AM, Alavi K, Sudan R, Wise PE. Rectal prolapse: an overview of clinical features, diagnosis, and patient-specific management strategies. J Gastrointest Surg. 2014; 18:1059–1069. PMID: 24352613.

2. Fengler SA, Pearl RK, Prasad ML, Orsay CP, Cintron JR, Hambrick E, et al. Management of recurrent rectal prolapse. Dis Colon Rectum. 1997; 40:832–834. PMID: 9221862.

3. Hool GR, Hull TL, Fazio VW. Surgical treatment of recurrent complete rectal prolapse: a thirty-year experience. Dis Colon Rectum. 1997; 40:270–272. PMID: 9118739.
4. Steele SR, Goetz LH, Minami S, Madoff RD, Mellgren AF, Parker SC. Management of recurrent rectal prolapse: surgical approach influences outcome. Dis Colon Rectum. 2006; 49:440–445. PMID: 16465585.

5. Pikarsky AJ, Joo JS, Wexner SD, Weiss EG, Nogueras JJ, Agachan F, et al. Recurrent rectal prolapse: what is the next good option? Dis Colon Rectum. 2000; 43:1273–1276. PMID: 11005496.
6. Tsugawa K, Sue K, Koyanagi N, Hashizume M, Wada H, Tomikawa M, et al. Laparoscopic rectopexy for recurrent rectal prolapse: a safe and simple procedure without a mesh prosthesis. Hepatogastroenterology. 2002; 49:1549–1551. PMID: 12397732.
7. Araki Y, Isomoto H, Tsuzi Y, Matsumoto A, Yasunaga M, Yamauchi K, et al. Transsacral rectopexy for recurrent complete rectal prolapse. Surg Today. 1999; 29:970–972. PMID: 10489150.

8. Tou S, Brown SR, Malik AI, Nelson RL. Surgery for complete rectal prolapse in adults. Cochrane Database Syst Rev. 2008; (4):CD001758. PMID: 18843623.

9. Hotouras A, Ribas Y, Zakeri S, Bhan C, Wexner SD, Chan CL, et al. A systematic review of the literature on the surgical management of recurrent rectal prolapse. Colorectal Dis. 2015; 17:657–664. PMID: 25772797.

10. D’Hoore A, Cadoni R, Penninckx F. Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg. 2004; 91:1500–1505. PMID: 15499644.

11. de Bruijn H, Maeda Y, Tan KN, Jenkins JT, Kennedy RH. Long-term outcome of laparoscopic rectopexy for full-thickness rectal prolapse. Tech Coloproctol. 2019; 23:25–31. PMID: 30604250.

12. Senapati A, Gray RG, Middleton LJ, Harding J, Hills RK, Armitage NC, et al. PROSPER: a randomised comparison of surgical treatments for rectal prolapse. Colorectal Dis. 2013; 15:858–868. PMID: 23461778.

13. Emile SH, Elbanna H, Youssef M, Thabet W, Omar W, Elshobaky A, et al. Laparoscopic ventral mesh rectopexy vs Delorme’s operation in management of complete rectal prolapse: a prospective randomized study. Colorectal Dis. 2017; 19:50–57. PMID: 27225971.

14. Joubert K, Laryea JA. Abdominal approaches to rectal prolapse. Clin Colon Rectal Surg. 2017; 30:57–62. PMID: 28144213.

15. Gurland B, E Carvalho ME, Ridgeway B, Paraiso MF, Hull T, Zutshi M. Should we offer ventral rectopexy to patients with recurrent external rectal prolapse? Int J Colorectal Dis. 2017; 32:1561–1567. PMID: 28785819.

16. Hyun K, Yang SJ, Lim KY, Lee JK, Yoon SG. Laparoscopic posterolateral rectopexy for the treatment of patients with a full thickness rectal prolapse: experience with 63 patients and short-term outcomes. Ann Coloproctol. 2018; 34:119–124. PMID: 29991200.

17. Lundby L, Iversen LH, Buntzen S, Wara P, Høyer K, Laurberg S. Bowel function after laparoscopic posterior sutured rectopexy versus ventral mesh rectopexy for rectal prolapse: a double-blind, randomised single-centre study. Lancet Gastroenterol Hepatol. 2016; 1:291–297. PMID: 28404199.

18. Barfield LR. Perineal approaches to rectal prolapse. Clin Colon Rectal Surg. 2017; 30:12–15. PMID: 28144207.

19. Elagili F, Gurland B, Liu X, Church J, Ozuner G. Comparing perineal repairs for rectal prolapse: Delorme versus Altemeier. Tech Coloproctol. 2015; 19:521–525. PMID: 26341686.

20. Hyun K, Yoon SG. Comparison of Delorme-Thiersch operation outcomes in men and women with rectal prolapse. Ann Coloproctol. 2019; 35:262–267. PMID: 31726002.

21. Festen S, van Geloven AA, Gerhards MF. Redo procedure for prolapse and haemorrhoids (PPH) for persistent and recurrent prolapse after PPH. Dig Surg. 2009; 26:418–421. PMID: 19923831.

22. Thorlakson RH. A modification of the Thiersch procedure for rectal prolapse using polyester tape. Dis Colon Rectum. 1982; 25:57–58. PMID: 7056143.

23. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
24. Ludbrook J, Royse AG. Analysing clinical studies: principles, practice and pitfalls of Kaplan-Meier plots. ANZ J Surg. 2008; 78:204–210. PMID: 18269491.

25. Javed MA, Afridi FG, Artioukh DY. What operation for recurrent rectal prolapse after previous Delorme’s procedure?: a practical reality. World J Gastrointest Surg. 2016; 8:508–512. PMID: 27462393.

26. Warwick AM, Zimmermann E, Boorman PA, Smart NJ, Gee AS. Recurrence rate after Delorme’s procedure with simultaneous placement of a Thiersch suture. Ann R Coll Surg Engl. 2016; 98:419–421. PMID: 27092405.

27. Ding JH, Canedo J, Lee SH, Kalaskar SN, Rosen L, Wexner SD. Perineal rectosigmoidectomy for primary and recurrent rectal prolapse: are the results comparable the second time? Dis Colon Rectum. 2012; 55:666–670. PMID: 22595846.
Fig. 1
Re-recurrence rate according to the relationship between previous and repeat repair methods. The relationship between previous and repeat repair methods did not affect the re-recurrence rate for patients with recurrent rectal prolapse.
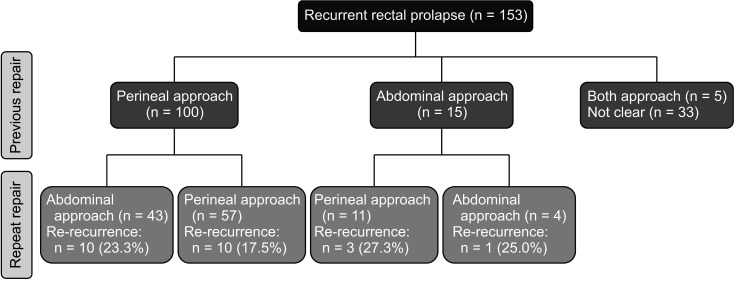
Fig. 2
Kaplan-Meier curves of re-recurrence rate between perineal and abdominal approaches for recurrent rectal prolapse.The curve did not show any difference in re-recurrence rate between the 2 approaches for recurrent rectal prolapse.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download