Abstract
Purpose
The incidence of gallstone disease and cholecystectomy is increasing worldwide. The aim of this study was to determine trends in the incidence of cholecystectomy in Korea.
Methods
The National Health Insurance Services database was used to determine patterns in proportion of cholecystectomy and cholecystostomy in the total population of Korea from 2003 to 2017. The age-standardized rate (ASR) was calculated to compare the cholecystectomy and cholecystostomy according to changes in the population structure over time. The ASR was investigated according to patient age, sex, socioeconomic status, use of computed tomography, and type of hospital to identify trends.
Results
The ASR per 100,000 based on the 2010 population of cholecystectomy cases increased markedly from 67.7 to 211.4 between 2003 and 2017. The ASR was consistently higher in female than male (71.9 vs. 63.6 in 2003, 221.8 vs. 201.8 in 2017). Furthermore, the ASR for cholecystectomy increased with age, and surgery for gallstone disease was performed more often at a specialized center than at other medical facilities. The length of hospital stay of cholecystectomy decreased steadily from 10.6 days in 2003 to 6.9 days in 2017.
Conclusion
This study shows that the incidence of cholecystectomy and cholecystostomy has steadily increased over the years in Korea, with a trend toward older age and higher socioeconomic status in patients undergoing cholecystectomy. Increasing use of computed tomography investigations could be a primary cause for this trend. An integrated strategy is needed to manage the increase in older patients undergoing cholecystectomy and shorten their hospital stay with medical safety.
Gallstone disease is a common digestive disease that is expensive to treat and shows geographical and ethnic differences worldwide [1]. Compared with the Western populations, East Asians (e.g., Koreans, Japanese, and Chinese) have a higher prevalence of pigment stones, stones in the common bile duct and intrahepatic duct, and less female predominance [2]. Acute cholecystitis, which occurs at a rate of 1% per year, is one of the most common complications of gallstone disease [3].
The primary treatment for symptomatic gallstone disease is the surgical removal of the gallbladder. By the mid-1990s, laparoscopic management of gallstone disease had replaced open surgery and become a standard procedure with benefits in terms of a shorter hospital stay, less postoperative pain, and a more rapid return to normal activity [4]. According to the National Health Insurance Service (NHIS) yearbook, admissions for gallstones and cholecystitis increased by 135% from 40,592 in 2005 to 95,337 in 2019 [56]. However, there are no reports on the prevalence of cholecystitis based on the number of surgeries performed.
The aim of this study was to determine the current trends in cholecystectomy in Korea based on the number of surgical codes recorded in a nationwide database by year.
The study was approved by the Institutional Review Board of the Gachon University Gil Medical Center, Gachon University College of Medicine (No. GFIRB2020-134) and conducted in accordance with the Declaration of Helsinki. The need for informed consent was waived.
Data on cholecystectomy and cholecystostomy-related medical utilization from 2003 to 2017 were obtained from the NHIS. The NHIS is a mandatory single-payer health care system in Korea; thus, all medical utilization data for the Korean population can be identified. The NHIS claims data contain 4 categories for collection of insurance premiums and reimbursement of insurance claims. Personal demographic data are collected, including patient age and sex, region, and income category. Diagnosis codes are entered using the Korean Standard Classification of Diseases and Causes of Death, 7th edition, a modified version of the International Classification of Disease, 10th revision. Medical procedure codes consisting of procedures, admissions, and operations are included. The gallstone disease and cholecystitis are defined with surgical codes, gallstone (K80), and cholecystitis (K81). During the study period (2003–2017), we collected 2,050,791 diagnoses of patients with gallstone and cholecystitis. Finally, the number of patients with cholecystectomy was 665,428 after excluding no inpatients and surgical operations. Prescriptions are also included in the NHIS data. The Minister of Health and Welfare in Korea classifies hospitals as tertiary referral, general, specialized, and others. According to the medical service act, The Minister of Health and Welfare may designate a general hospital specializing in providing medical services requiring a high level of expertise for treating diseases as a tertiary referral hospital. A general hospital shall be equipped with at least 100 patient beds with medical specialists exclusively dedicated to every specialized department. Specialized hospitals in this study provide medical services requiring a high level of expertise in a surgical department or treating a specific disease related to general surgery. Other hospitals include those with a limited number of beds. In this study, demographic records, diagnosis codes, and procedure codes were used to identify medical utilization related to cholecystectomy and cholecystostomy.
This study was based on descriptive analysis. Patients who underwent cholecystectomy and cholecystostomy were defined as those who met two of the following criteria: (1) acute cholecystitis (K81) or gallstones (K80) as the main diagnosis code and (2) having a procedure or operation code for cholecystectomy (Q7380) or cholecystostomy (Q7390 and M6690) (Supplementary Fig. 1). To analyze the incidence patterns of cholecystectomy and cholecystostomy, we performed subgroup analysis by sex (male and female), age (0–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, and ≥80 years), whether or not CT scans were obtained (NHIS code of HA465), type of surgical facility (tertiary, general, specialized, or others), and patient income group (1st–5th, 6th–10th, 11th–15th, and 16th–20th). The average length of stay (LOS; the number of days from hospitalization to discharge) was also calculated to estimate the performance of the medical provider.
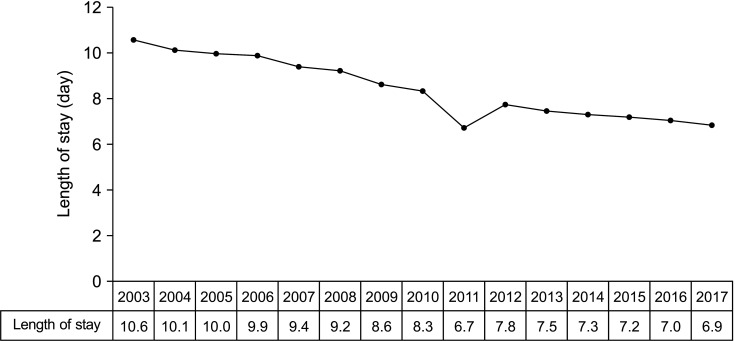
The age-standardized rate (ASR) was used to compare trends in cholecystectomy and cholecystectomy according to changes in the population structure over time. The standard Korean population in 2011 was used to calculate the ASR. The equation used to calculate ASR per 100,000 is as follows:
All statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
The ASR for cholecystectomy cases increased markedly from 67.7 to 211.4 between 2003 and 2017. The total crude number of patients by year also increased with time from 18,081 in 2003 to 56,470 in 2017. A subgroup analysis according to sex showed that the ASR for cholecystectomy increased during the study period from 71.9 (crude number 9,540) to 221.2 (crude number 29,353) in female and from 63.6 (crude number 8,542) to 201.8 (crude number 27,116) in male. Overall, the ASR was consistently high in female; compared with 2003, the ASR in 2017 had increased by 307.7% in female and 317.4% in male, indicating a greater increase in male. However, the trend according to sex showed a similar increasing tendency (data not shown) (Fig. 1).
Subgroup analysis was performed according to age. In all age groups over the 20s, it was confirmed that the ASR continued to increase as time passed. During the study period, the ASR for cholecystectomy was divided into three phases. From 2003 to 2005, the ASR continued to increase in the population aged younger than the 60s and from 2006 to 2010 increased steadily in the 70s. Since 2011, the ASR has continued to increase in the population aged older than 80 years (Fig. 2).
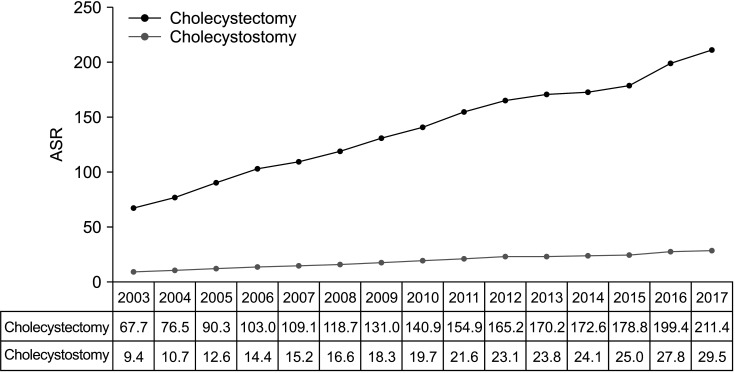
During the study period, there was an increase in the number of CT scans performed to diagnose gallbladder disease and the diagnostic yield using CT from 4.3% in 2003 to 51.0% in 2017. However, the growth rate has remained similar since 2014, with no significant fluctuations (Fig. 3). Moreover, the ASR for cholecystectomy steadily increased during the study period, resulting in a 312% increase in ASR in 2017 compared to 2003. Similarly, the number of cholecystostomy procedures, such as percutaneous transhepatic cholecystostomy, increased by approximately 313%, from 9.4 in 2003 to 29.5 in 2017. The crude number of cholecystectomy and cholecystostomy was found to have discrepancies, but the rate of increase was similar (Fig. 4).
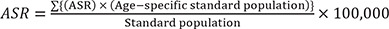
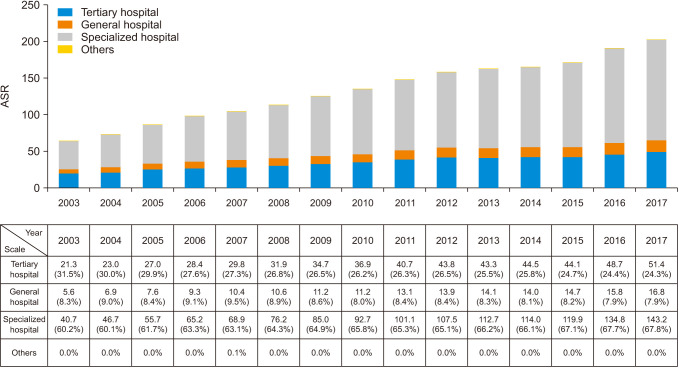
We investigated the cholecystectomy rate according to the type of hospital facility where gallstone disease surgery was performed during the study period. The ASR for surgery performed at specialized hospitals was higher than that for tertiary or general hospitals during the study period. The proportion of surgery in the specialized hospital was maintained at 60% or more during the study period, and the proportion continued to increase over time. On the other hand, the proportion of tertiary hospitals continued to decrease from more than 30% at the beginning of the study to less than the mid-20% at the end of the study, and the proportion of general hospitals was almost the same (Fig. 5). We also analyzed the length of hospital stay of cholecystectomy patients over time during the study period. The average LOS for cholecystectomy decreased steadily and remarkably from 10.6 days in 2003 to 6.9 days in 2017 (Fig. 6). LOS by facility could be confirmed over time through another statistical analysis of the open national big data from the Health Insurance Review and Assessment database. Although the decrease showed some differences depending on the surgical facility, a continuous decrease could be confirmed in common (Supplementary Fig. 2).
We analyzed the socioeconomic status of the patient by dividing income during the study period into 20 quintiles, ranging from the poorest group (group 1) to the most affluent group (group 20) and then merged them into 4 groups (groups 1st–5th, low income; groups 6th–10th, lower–middle income; groups 11th–15th, upper–middle income; and groups 16th–20th, upper income). During the 14 years of observation, the ASR for cholecystectomy was consistently highest in the upper income group (groups 16th–20th) (Supplementary Fig. 3).
This study is the first to analyze trends in cholecystectomy in Korea based on a population-based approach using data from the NHIS without limitations on age or sex. We found a marked increase in the number of cholecystectomies performed in Korea over a 14-year period. According to a Health Insurance Review and Assessment Service, cholecystectomy was the seventh most common type of surgery performed in Korea in 2015 [7]. During the study period, the annual ASR for cholecystectomy increased from 67.7 to 211.4, and the rate for cholecystostomy, such as percutaneous transhepatic gallbladder drainage, also showed a steady increase. The results of this study are consistent with previous reports of an approximately 3-fold increase in the number of patients with a diagnosis of gallstones between 1996 and 2015 [8]. The study mentioned above is quite different from our study in that it was limited to tertiary hospitals in Korea and analyzed the chronological changes of patients by focusing on the classification of gallstone. However, it is meaningful because the study examined the characteristics of patients with gallstone disease based on 20 years of records, and it is considered comparable to our study in that it confirmed the increase in gallstone patients over time. According to a previous study, the prevalence of gallbladder polyp increased linearly from 2.9% in 2002 to 8.5% in 2012 [9]. Additionally, trends of the increasing gallbladder-stone cases and decreasing common bile duct- and intrahepatic duct-stone cases were identified [10]. Such changes in gallbladder disease may have significantly affected the surgical indication for cholecystectomy. Acute cholecystitis (K81) or gallstones (K80) was used as the primary diagnosis in this study, and the relationship between these diagnoses and cholecystectomy was analyzed. Since diagnostic codes such as gallbladder polyp were not included in the cohort of this study, it was not possible to confirm the changing pattern. Nevertheless, since cholecystitis is known to account for more than 80% of cholecystectomy, the analysis of this study is valuable [11]. Also, during the study period, no remarkable change in the national health insurance system that could shift the paradigm of surgical indication for cholecystectomy was confirmed, so the effect of the indication change on the incidence of cholecystectomy can be evaluated as relatively low.
Cholecystectomy is one of the basic procedures in the field of general surgery, and it is performed not only in tertiary hospitals but also in hospitals of various scales, especially specialized hospitals. Therefore, it is judged that a study using NHIS claims data would be more effective than a retrospective study of a single big center to know the trend of cholecystectomy or cholecystostomy in Korea. Another study reported that the number of inpatient discharges related to cholecystitis continued to increase, and the cholecystectomy rates increased and remained stable at a higher level. These studies were also comparable to the increasing trend of our study [1213].
Regarding cholecystitis, either elective or emergency cholecystectomy or delayed cholecystectomy af ter cholecystostomy is performed depending on the degree of inflammation (gallbladder empyema, etc.) or the patient's general condition. Therefore, to investigate all cholecystitis patients, it is appropriate to include cholecystostomy as well. In addition, the reason for comparing the two procedures was to analyze whether the detection by an early diagnostic tool such as CT or medical examination increased and whether severe symptomatic gallbladder disease occurred more frequently. Information on acute vs. chronic disease, elective vs. emergency operations, open vs. minimally invasive surgery, and postoperative complications and mortality can be inferred through information on diagnostic codes and hospitalization routes. Still, these methods are quite inaccurate, and there is a problem in that bias increases because not all chronic cholecystitis is operated on. Therefore, this study using data from the NHIS is considered meaningful and appropriate.
In Korea, confirmed cases of symptomatic gallbladder disease have been covered by NHIS since 1996, and the increase in the number of CT investigations performed likely reflects this change in health care policy. This change in health care policy is reflected in the marked increase in the number of CT scans performed during the study period, which probably explains the increased number of patients undergoing surgery for asymptomatic or mildly symptomatic gallstone disease and the trend of a shorter LOS after surgery. The number of diagnostic tests performed for gallstone disease can be expected to increase in the future, given that NHI cover was extended to include ultrasound treatment in 2018 and CT screening in 2019. The role of ultrasonography in diagnosing gallbladder disease is significant and cannot be overlooked. However, according to the NHIS, health insurance for epigastric ultrasound has been implemented since 2018. Since the timing of such insurance application is somewhat different from the progress of this study, there is a limitation in that it is challenging to evaluate ultrasound diagnosis performed without insurance accurately. Therefore, we used a CT scan (NHIS code HA465) that can be confirmed with the NHIS database in this study. The use of these diagnoses is judged to be appropriate.
Higher body mass index, obesity, abdominal fat, metabolic syndrome, and diabetes mellitus are confirmed risk factors for gallstones and cholecystectomy [7]. A diet high in fat, advanced age, female sex, and a high cholesterol saturation index have also been associated with increased occurrence of gallstones [14]. In Korea, the obesity rate increased by 1.19-fold between 1998 and 2011, and the prevalence of abdominal obesity has also gradually increased over the years [15]. In 1 study, the morbidity of obesity and abdominal obesity increased to 35.7% and 23.8%, respectively, between 2009 and 2018, and an upward trend of obesity and abdominal obesity was observed in both sexes and in nearly all age groups [16]. Moreover, in a study that analyzed data from the Korea National Health and Nutrition Examination Survey, the frequency of metabolic syndrome increased from 24.9% in 1998 to 31.3% in 2007 [17]. Metabolic syndrome has shown a greater trend of increase in Korea than in other countries [18]. In Korea, the number of individuals aged ≥65 years reached 7 million (14.2% of the overall population) in 2018, which officially defines Korea as an ‘aged’ society. Korea is expected to progress to a ‘super-aged society’ within 12 years based on the rapid ongoing trend of aging and is projected to have the world’s highest life expectancy by 2030 [1920]. Our present findings confirm that the ASR for cholecystectomy increases with age, which is consistent with the results of previous studies [21]. These findings indicate that the ASR for cholecystectomy increased during all periods and in age groups and was especially apparent in the elderly. Given the rapid acceleration of population aging in Korea, the proportion of elderly patients with gallbladder-related disease and rates of cholecystectomy are expected to increase in the future.
In this study, the ASR for cholecystectomy increased most in the section of the population with the highest income. Universal NHIS cover became available in Korea in 1989 and was expanded to include the entire population in 2000. Approximately 97% of all Koreans now have NHIS cover. The remaining 3% are covered by the medical aid program for low-income citizens [22]. The high ASR for cholecystectomy in the more affluent section of the population despite the broad coverage afforded by the NHIS is likely explained by the indirect costs of hospitalization, additional CT investigations, and accessibility to health checkups. However, other characteristics in the high-income group, including whether or not they were older, need to be investigated further in the future.
The ASR for cholecystectomy was higher in specialized hospitals than in tertiary referral hospitals or general hospitals, increasing proportions in all three types of centers. Previous studies showed reductions in postoperative morbidity and mortality rates and wound infection and pneumonia rates with the advent of laparoscopic cholecystectomy [23]. High numbers of surgical procedures are now being performed in specialized hospitals that are relatively small, probably because of increased use of minimally invasive surgery and the safety afforded by improved postoperative outcomes. The hazard identification and risk assessment system also classifies various disease groups to allow efficient delivery of health care services and distribution of roles among medical institutions and to ensure the objectivity of the patient classification system. As part of this policy, medical resources are allocated to increase the capacity of tertiary referral hospitals and general hospitals, which has resulted in an increased ASR for smaller specialized surgical facilities.
In this study, the LOS decreased from 10.6 days in 2003 to 6.9 days in 2017. In previous studies, the median LOS reported ranged between 2 days and 2.2 days [1324]. Moreover, a recent meta-analysis that included 10,615 patients found that the mean LOS was 61.2 hours [25]. However, given that the hospitals enrolled in this meta-analysis were diverse and that the LOS can be affected by financial or organizational factors, differences may occur depending on hospital size and insurance coverage between countries. The LOS after cholecystectomy in Korea would be expected to be shorter in the future. The development of minimally invasive surgery, such as single-incision laparoscopic cholecystectomy and robotic cholecystectomy [26], and improvements in medical care, such as enhanced recovery after surgery, is thought to reduce the LOS after cholecystectomy [1127].
This study had several limitations. First, it was based on NHIS data, so it was not possible to obtain detailed information on patient characteristics, symptoms, and compliance or on the preferences of attending physicians. Furthermore, given that NHIS data are collected based on a diagnosis and treatment modality code, the possibility of missing information or information bias cannot be excluded. Second, the up-to-date trend cannot be grasped since the study was conducted on data up to 2017. Further extensive research using more recent data is needed.
In conclusion, this study is the first to investigate the nationwide prevalence of cholecystectomy in Korea and found an increasing trend of older age and a higher socioeconomic level in patients undergoing cholecystectomy. On the other hand, it was confirmed that the LOS for cholecystectomy continued to decrease. A multidisciplinary strategy will be needed to manage the increasing number of older patients who underwent cholecystectomy and keep their hospital stay as short as possible while ensuring medical safety.
Notes
References
1. Shaffer EA. Gallstone disease: epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006; 20:981–996. PMID: 17127183.
2. Park YH, Park SJ, Jang JY, Ahn YJ, Park YC, Yoon YB, et al. Changing patterns of gallstone disease in Korea. World J Surg. 2004; 28:206–210. PMID: 14708060.

3. Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002; 97:249–254. PMID: 11866258.

4. Johnson AG. Reduced postoperative hospitalization after laparoscopic cholecystectomy. Br J Surg. 1991; 78:1019.

5. Health Insurance Review & Assessment Service (HIRA). National Health Insurance Service (NHIS). 2019 National Health Insurance statistical yearbook. Wonju: HIRA, NHIS;2020.
6. Health Insurance Review & Assessment Service (HIRA). National Health Insurance Service (NHIS). 2005 National Health Insurance statistical yearbook. Wonju: HIRA, NHIS;2006.
7. Kim HS, Cho SK, Kim CS, Park JS. Big data and analysis of risk factors for gallbladder disease in the young generation of Korea. PLoS One. 2019; 14:e0211480. PMID: 30794560.

8. Zhao J, Kim H, Han Y, Choi YJ, Byun Y, Kwon W, et al. Chronological changes in epidemiologic features of patients with gallstones over the last 20 years in a single large-volume Korean center. Ann Surg Treat Res. 2019; 97:136–141. PMID: 31508394.

9. Lee YJ, Park KS, Cho KB, Kim ES, Jang BK, Chung WJ, et al. Shifting prevalence of gallbladder polyps in Korea. J Korean Med Sci. 2014; 29:1247–1252. PMID: 25246743.

10. Chang YR, Jang JY, Kwon W, Park JW, Kang MJ, Ryu JK, et al. Changes in demographic features of gallstone disease: 30 years of surgically treated patients. Gut Liver. 2013; 7:719–724. PMID: 24312714.

11. Lee W, Roh YH, Kang SH, Kim CY, Choi Y, Han HS, et al. The chronological change of indications and outcomes for single-incision laparoscopic cholecystectomy: a Korean multicenter study. Surg Endosc. 2021; 35:3025–3032. PMID: 32583067.

12. Wadhwa V, Jobanputra Y, Garg SK, Patwardhan S, Mehta D, Sanaka MR. Nationwide trends of hospital admissions for acute cholecystitis in the United States. Gastroenterol Rep (Oxf). 2017; 5:36–42. PMID: 27174434.

13. Talseth A, Lydersen S, Skjedlestad F, Hveem K, Edna TH. Trends in cholecystectomy rates in a defined population during and after the period of transition from open to laparoscopic surgery. Scand J Gastroenterol. 2014; 49:92–98. PMID: 24354967.

14. Pak M, Lindseth G. Risk factors for cholelithiasis. Gastroenterol Nurs. 2016; 39:297–309. PMID: 27467059.

15. Kim CS, Ko SH, Kwon HS, Kim NH, Kim JH, Lim S, et al. Prevalence, awareness, and management of obesity in Korea: data from the Korea national health and nutrition examination survey (1998-2011). Diabetes Metab J. 2014; 38:35–43. PMID: 24627826.

16. Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee SS, et al. Obesity fact sheet in Korea, 2019: prevalence of obesity and abdominal obesity from 2009 to 2018 and social factors. J Obes Metab Syndr. 2020; 29:124–132. PMID: 32581145.

17. Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011; 34:1323–1328. PMID: 21505206.
18. Lim S, Jang HC, Park KS, Cho SI, Lee MG, Joung H, et al. Changes in metabolic syndrome in American and Korean youth, 1997-2008. Pediatrics. 2013; 131:e214–e222. PMID: 23209102.

19. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017; 389:1323–1335. PMID: 28236464.

20. Hong N, Kim KJ, Lee SJ, Kim CO, Kim HC, Rhee Y, et al. Cohort profile: Korean Urban Rural Elderly (KURE) study, a prospective cohort on ageing and health in Korea. BMJ Open. 2019; 9:e031018.

21. Pisano M, Ceresoli M, Cimbanassi S, Gurusamy K, Coccolini F, Borzellino G, et al. 2017 WSES and SICG guidelines on acute calcolous cholecystitis in elderly population. World J Emerg Surg. 2019; 14:10. PMID: 30867674.

22. Han SR, Kim HJ, Kim NH, Shin S, Yoo RN, Kim G, et al. Inguinal hernia surgery in Korea: nationwide data from 2007-2015. Ann Surg Treat Res. 2019; 97:41–47. PMID: 31297352.

23. Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, et al. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015; 18:196–204. PMID: 25958296.

24. Jensen KK, Roth NO, Krarup PM, Bardram L. Surgical management of acute cholecystitis in a nationwide Danish cohort. Langenbecks Arch Surg. 2019; 404:589–597. PMID: 31297607.

25. Ryan JM, O’Connell E, Rogers AC, Sorensen J, McNamara DA. Systematic review and meta-analysis of factors which reduce the length of stay associated with elective laparoscopic cholecystectomy. HPB (Oxford). 2021; 23:161–172. PMID: 32900611.

26. Lee EK, Park E, Oh WO, Shin NM. Comparison of the outcomes of robotic cholecystectomy and laparoscopic cholecystectomy. Ann Surg Treat Res. 2017; 93:27–34. PMID: 28706888.

27. Udayasankar M, Udupi S, Shenoy A. Comparison of perioperative patient comfort with ‘enhanced recovery after surgery (ERAS) approach’ versus ‘traditional approach’ for elective laparoscopic cholecystectomy. Indian J Anaesth. 2020; 64:316–321. PMID: 32489207.

SUPPLEMENTARY MATERIALS
Supplementary Figs. 1–3 can be found via https://doi.org/10.4174/astr.2022.102.4.205.
Supplementary Fig. 2
Mean length of hospital stay in patients undergoing cholecystectomy according to each surgical facility from the Health Insurance Review and Assessment database.
Supplementary Fig. 3
Proportions of patients according to income. During the study period, the age-standardized rate (ASR) for cholecystectomy was consistently highest in the most affluent group.
Fig. 1
Overall and sex-specific age-standardized rates (ASRs) of cholecystectomy in Korea. During the study period, the ASR increased dramatically from 67.7 to 211.4. A subgroup analysis according to sex showed that the ASR of patients who underwent cholecystectomy increased from 71.9 to 221.2 in female and from 63.6 to 201.8 in male during the study period.
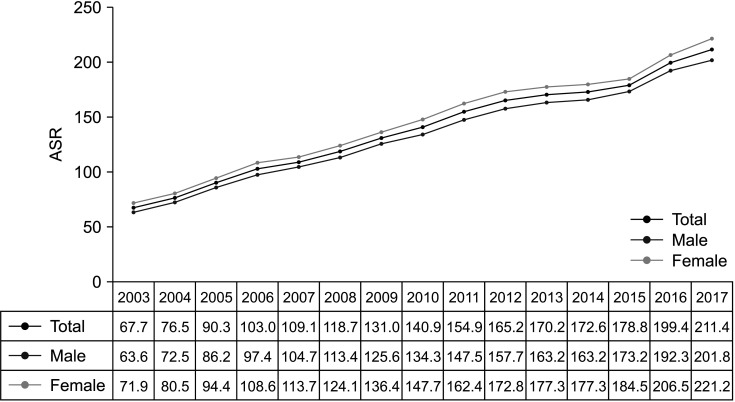
Fig. 2
Change in the age of patients undergoing cholecystectomy during the study period. The age-standardized rate (ASR) continued to increase with age below the 60s from 2003 to 2005 and below the 70s from 2006 to 2010. Since 2011, this increase has continued in patients aged ≥80 years.
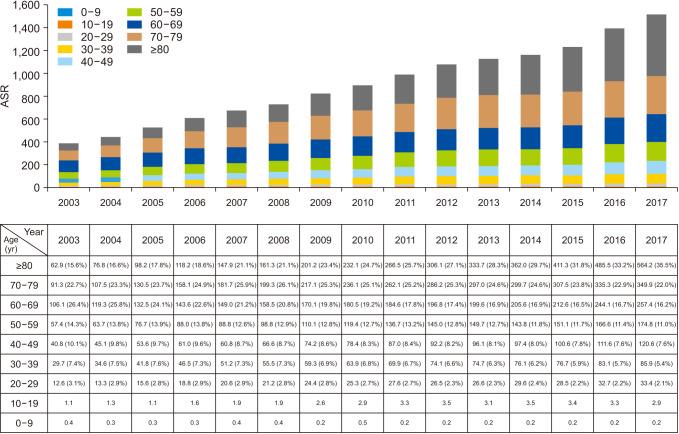
Fig. 3
Use of CT scan for diagnosis of gallbladder disease by year. During the study period, the total number of CT investigations steadily increased, as did the rate of diagnosis of gallbladder disease.
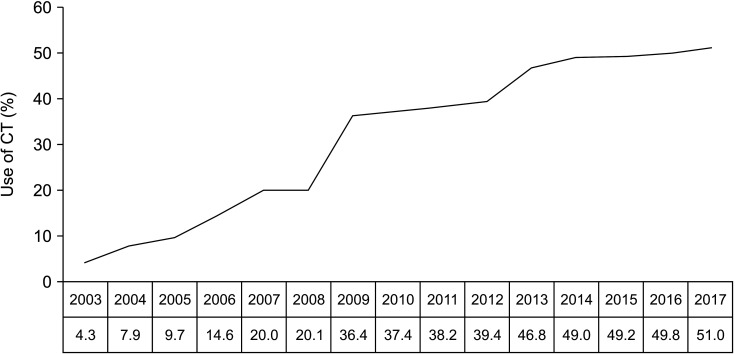
Fig. 4
Changing patterns in the age-standardized rate (ASR) for cholecystectomy and cholecystostomy. The annual incidence of ASR for cholecystectomy steadily increased during the study period, as did cholecystostomy procedures, such as percutaneous transhepatic gallbladder drainage.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download