1. Laveneziana P, Di Paolo M, Palange P. The clinical value of cardiopulmonary exercise testing in the modern era. Eur Respir Rev. 2021; 30(159):200187. PMID:
33408087.

2. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002; 346(11):793–801. PMID:
11893790.

3. Palange P, Ward SA, Carlsen KH, Casaburi R, Gallagher CG, Gosselink R, et al. Recommendations on the use of exercise testing in clinical practice. Eur Respir J. 2007; 29(1):185–209. PMID:
17197484.

4. Kim HJ, Park SW, Cho BR, Hong SH, Park PW, Hong KP. The role of cardiopulmonary exercise test in mitral and aortic regurgitation: it can predict post-operative results. Korean J Intern Med. 2003; 18(1):35–39. PMID:
12760266.

5. Hwang TW, Kim SO, Kim MS, Jang SI, Kim SH, Lee SY, et al. Short-term change of exercise capacity in patients with pulmonary valve replacement after tetralogy of fallot repair. Korean Circ J. 2017; 47(2):254–262. PMID:
28382082.

6. Kim GB, Kwon BS, Choi EY, Bae EJ, Noh CI, Yun YS, et al. Usefulness of the cardiopulmonary exercise test in congenital heart disease. Korean Circ J. 2007; 37(10):489–496.

7. Kim JY, Yun BS, Lee S, Jung SY, Choi JY, Kim NK. Changes in strain pattern and exercise capacity after transcatheter closure of atrial septal defects. Korean Circ J. 2017; 47(2):245–253. PMID:
28382081.

8. American Thoracic Society. American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003; 167(2):211–277. PMID:
12524257.
9. Paap D, Takken T. Reference values for cardiopulmonary exercise testing in healthy adults: a systematic review. Expert Rev Cardiovasc Ther. 2014; 12(12):1439–1453. PMID:
25418758.

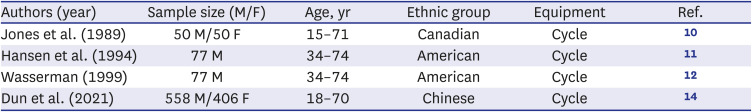
10. Jones NL, Makrides L, Hitchcock C, Chypchar T, McCartney N. Normal standards for an incremental progressive cycle ergometer test. Am Rev Respir Dis. 1985; 131(5):700–708. PMID:
3923878.
11. Hansen JE, Sue DY, Wasserman K. Predicted values for clinical exercise testing. Am Rev Respir Dis. 1984; 129(2 Pt 2):S49–S55. PMID:
6421218.
12. Wasserman K. Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications. 5th ed. Philadelphia, PA, USA: Wolters Kluwer Health/Lippincott Williams & Wilkins;2012. p. 572.
13. Koch B, Schäper C, Ittermann T, Spielhagen T, Dörr M, Völzke H, et al. Reference values for cardiopulmonary exercise testing in healthy volunteers: the SHIP study. Eur Respir J. 2009; 33(2):389–397. PMID:
18768575.

14. Dun Y, Olson TP, Li C, Qiu L, Fu S, Cao Z, et al. Characteristics and reference values for cardiopulmonary exercise testing in the adult Chinese population - The Xiangya hospital exercise testing project (the X-ET project). Int J Cardiol. 2021; 332:15–21. PMID:
33716041.

15. Mohammad MM, Dadashpour S, Adimi P. Predicted values of cardiopulmonary exercise testing in healthy individuals (a pilot study). Tanaffos. 2012; 11(1):18–25.
16. Ong KC, Loo CM, Ong YY, Chan SP, Earnest A, Saw SM. Predictive values for cardiopulmonary exercise testing in sedentary Chinese adults. Respirology. 2002; 7(3):225–231. PMID:
12153688.

17. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35(8):1381–1395. PMID:
12900694.

18. Ahmadian HR, Sclafani JJ, Emmons EE, Morris MJ, Leclerc KM, Slim AM. Comparison of predicted exercise capacity equations and the effect of actual versus ideal body weight among subjects undergoing cardiopulmonary exercise testing. Cardiol Res Pract. 2013; 2013:940170. PMID:
23653881.

19. Itoh H, Ajisaka R, Koike A, Makita S, Omiya K, Kato Y, et al. Heart rate and blood pressure response to ramp exercise and exercise capacity in relation to age, gender, and mode of exercise in a healthy population. J Cardiol. 2013; 61(1):71–78. PMID:
23182944.

20. Yu R, Yau F, Ho S, Woo J. Cardiorespiratory fitness and its association with body composition and physical activity in Hong Kong Chinese women aged from 55 to 94 years. Maturitas. 2011; 69(4):348–353. PMID:
21683535.

21. Jee Y, Kim Y, Jee SH, Ryu M. Exercise and cancer mortality in Korean men and women: a prospective cohort study. BMC Public Health. 2018; 18(1):761. PMID:
29914427.

22. Kim BJ, Kim Y, Oh J, Jang J, Kang SM. Characteristics and safety of cardiopulmonary exercise testing in elderly patients with cardiovascular diseases in Korea. Yonsei Med J. 2019; 60(6):547–553. PMID:
31124338.

23. Kim YH, Shim WJ, Kim MA, Hong KS, Shin MS, Park SM, et al. Utility of pretest probability and exercise treadmill test in Korean women with suspected coronary artery disease. J Womens Health (Larchmt). 2016; 25(6):617–622. PMID:
26562494.

24. Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing: data from the fitness registry and the importance of exercise national database. Mayo Clin Proc. 2015; 90(11):1515–1523. PMID:
26455884.

25. John N, Thangakunam B, Devasahayam AJ, Peravali V, Christopher DJ. Maximal oxygen uptake is lower for a healthy Indian population compared to white populations. J Cardiopulm Rehabil Prev. 2011; 31(5):322–327. PMID:
21734591.

26. Singh R, Singh HJ, Sirisinghe RG. Spirometric studies in Malaysians between 13 and 69 years of age. Med J Malaysia. 1993; 48(2):175–184. PMID:
8350793.
27. Vijayan VK, Kuppurao KV, Venkatesan P, Sankaran K, Prabhakar R. Pulmonary function in healthy young adult Indians in Madras. Thorax. 1990; 45(8):611–615. PMID:
2402724.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download