This article has been
cited by other articles in ScienceCentral.
Abstract
Background
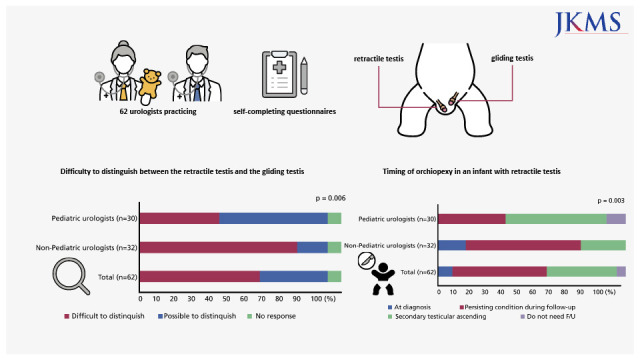
It is quite difficult to distinguish retractile testis from gliding testis, which requires different treatment planning in the clinic setting. We evaluated practice patterns of urologists in Korea regarding the diagnosis and management of retractile and gliding testes.
Methods
We mailed or e-mailed self-completion questionnaires consisting of 20 items to 106 urologists practicing in Korean hospitals concerning the diagnosis and treatment of cryptorchidism. We collected and analyzed the responses statistically.
Results
Responses were received from 62 urologists. The response rate was 58.5%. Thirty-seven urologists (59.7%) actually felt they had difficulty in distinguishing retractile testis from gliding testis in the clinic setting. This rate was higher for non-pediatric urologists (78.1%) than for pediatric urologists (40.0%) (P = 0.006). In cases of infant retractile testis, only five urologists (8.1%) said that they would perform orchiopexy immediately, with 54 (87.1%) urologists saying they would do follow-up. In cases of preschool-age children with retractile testis, 17 urologists (27.4%) said that they would perform orchiopexy immediately with 41 (66.1%) urologists saying they would do follow-up. In cases of infant gliding testis, 37 urologists (59.7%) said that they would perform orchiopexy immediately with 24 (38.7%) urologists saying they would do a follow-up.
Conclusion
More than half (59.7%) of Korean urologists revealed it challenging to distinguish retractile testis and gliding testis in the clinical setting. The more it was difficult to diagnose retractile testis with certainty, the more frequent surgical correction was chosen for treatment. Therefore, it is essential to prevent unnecessary surgical treatment by establishing a practical guideline.
Go to :

Graphical Abstract
Go to :

Keywords: Cryptorchidism, Child, Testis, Practice Patterns, Physicians, Surveys and Questionnaires, Practice Guideline
INTRODUCTION
Recently, parents have been increasingly concerned and anxious about their children’s testicles. Cryptorchidism, or undescended testis, is a common genital anomaly that is extensively studied yet incompletely understood. Orchiopexy, a treatment option for cryptorchidism, is a common operation in pediatric urology.
The normal scrotal position of the testis has been defined as the positioning of the testis at the midpoint, or at or below mid scrotum.
1 Although “high scrotal testis” is not routinely considered undescended by most clinicians, this has been included in the definition of undescended testis in some epidemiologic studies.
2 This is likely a heterogeneous group that includes stable descended “retractile” testis and undescended “gliding” testis.
3 Retractile testis is scrotal testis that retract easily out of the scrotum but can be manually replaced in a stable scrotal position and remain there at least temporarily until there is a recurrent stimulation. On the other hand, gliding testis is not stable and include low undescended testicles.
4
In prepubertal boys, what seems like an undescended testis is often a retractile testis that results from a brisk cremasteric reflex and does not require a surgical intervention. A retractile testis must be differentiated from an ascending testis that may require an orchidopexy. However, the management of retractile testis is still controversial. Recent articles have recommended that only observation in cases of retractile testis is needed.
56 In more than 70% of patients with a retractile testis, the condition evolves favorably without the need for surgery.
7 However, there is a 25% risk of these testis ascending and becoming acquired cryptorchidism in adolescence.
8 In a Korean study, about 16.3% of patients with retractile testis required surgical correction during long-term follow-up.
9
Retractile testis, in some cases, may be difficult to distinguish from the gliding testis that present as high scrotal testes in the clinic setting. In this case, some non-specialists often choose unnecessary surgery for defensive and preventive treatment. Therefore, it will be meaningful to understand the actual practice patterns of all urologists for retractile testis in order to develop proper clinical guidelines. Therefore, we evaluated the actual practice patterns of Korean urologists regarding the diagnosis and management of retractile and gliding testes and the difference between pediatric urologists and general urologists via a questionnaire survey.
Go to :

METHODS
We conducted a questionnaire survey of 106 urologists who worked in a Korean training hospital from March to July 2018. We distributed a self-administered questionnaire consisting of 20 items on the diagnosis and treatment of retractile and gliding testes (
Appendix 1) via email or via mail with letters.
The questionnaires dealt with cases of retractile and gliding testes in infants and cases of retractile testis in childhood. If errors were found in the retrieved questionnaire, they were corrected or supplemented by telephone or face-to-face interviews. Prior to the questionnaires, we checked the period of urologic practice and the rate of pediatric patient treatment at their hospital.
We received responses from 62 urologists. The response rate was 58.5%. We divided the urologists into two groups, according to the number of pediatric patients who had visited each hospital. If the urologist treated pediatric patients accounting for more than 25 percent of total patients, or if the individual was a member of the Korean Society of Pediatric Urology, this urologist was regarded as a pediatric urologist. Non-pediatric urologist was defined as treating pediatric patients less than 25 percent of total patients.
Thirty (48.4%) were pediatric urologists, and 32 (51.6%) were non-pediatric urologists. We compared and statistically analyzed the two groups’ distribution of responses.
Statistical analysis
We performed statistical analysis by using the IBM SPSS statistics software, version 22.0 (IBM Co., Armonk, NY, USA), and the two groups were compared using the Fisher's exact test and the chi-squared test. A P value < 0.05 was considered to be statistically significant.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Pusan National University Yangsan Hospital (approval No. 05-2018-073). Informed consent was submitted by all subjects when they were enrolled.
Go to :

RESULTS
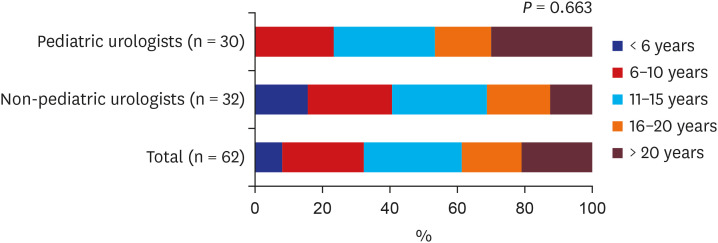
Fig. 1 shows the distribution of practice duration according to the duration of the urologists’ qualifications.
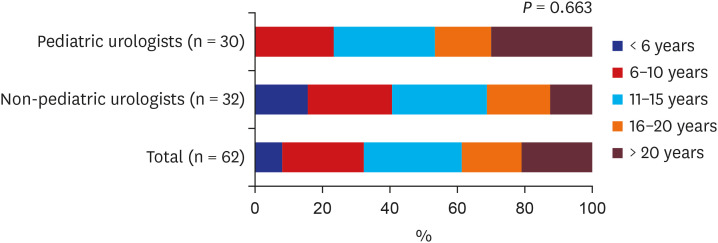 | Fig. 1 Duration of urologist qualification.
|
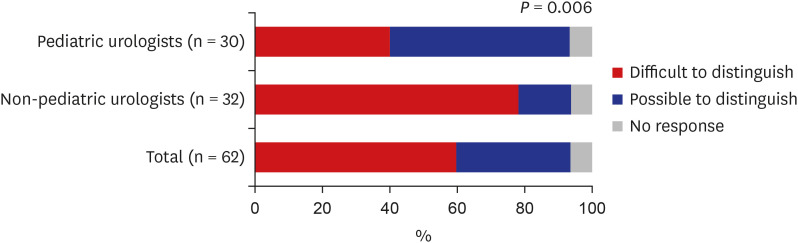
Thirty-seven urologists (59.7%) had difficulty distinguishing retractile testis from gliding testis in the clinic setting. This rate was higher in non-pediatric urologists (78.1%) than in pediatric urologists (40.0%) (
P = 0.006) (
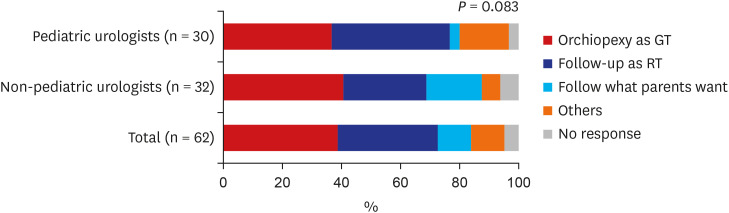
Fig. 2). The treatment planning varied among the respondents when they had difficulty distinguishing between retractile and gliding testes in the clinic setting. Each one-third of urologists preferred surgical correction (38.7%) or follow-up (33.9%) for when it was difficult to distinguish either a retractile or a gliding testis. The treatment planning showed various but statistically insignificant differences between pediatric and non-pediatric urologists (
P = 0.083) (
Fig. 3).
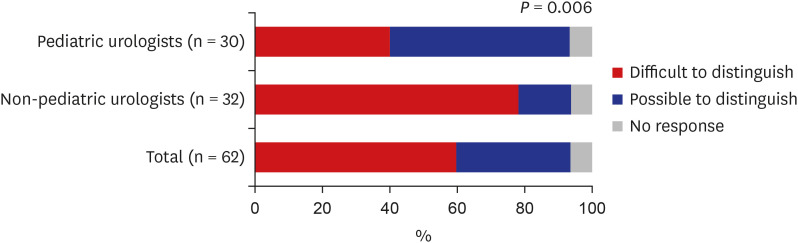 | Fig. 2 Difficulty to distinguish between the retractile testis and the gliding testis in their clinic.
|
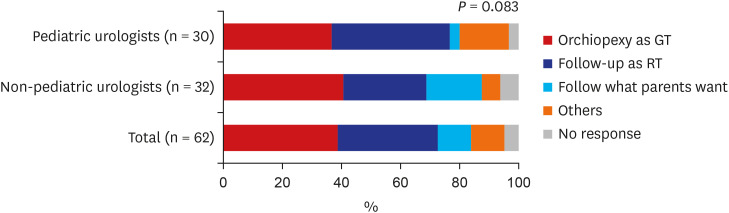 | Fig. 3
Treatment plan when it was difficult.
GT = gliding testis, RT = retractile testis.

|
Most of the urologists (98.4%) agreed that cryptorchidism could cause infertility and testicular dysfunction in the future. Although 50 of these urologists (80.6%) agreed on the adverse effects of gliding testis, 13 of them (21.0%) agreed this was the case with retractile testis. The rate difference was especially notable among the urologists, with 31.2% of non-pediatric urologists (10 of 32) compared to 10.0% of pediatric urologists (3 of 30) (P > 0.05).
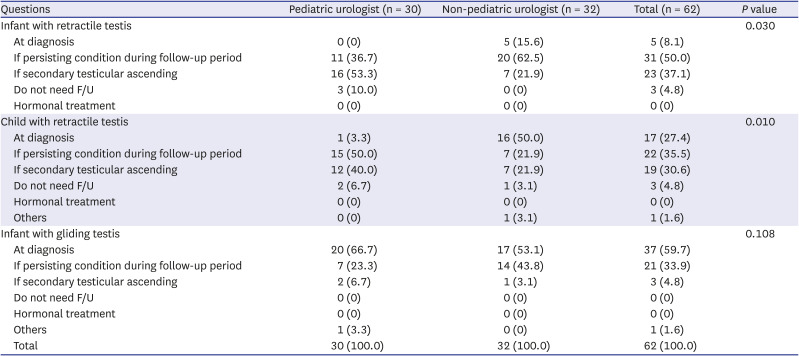
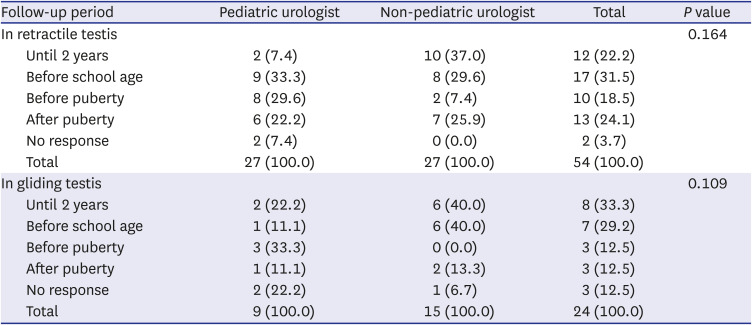
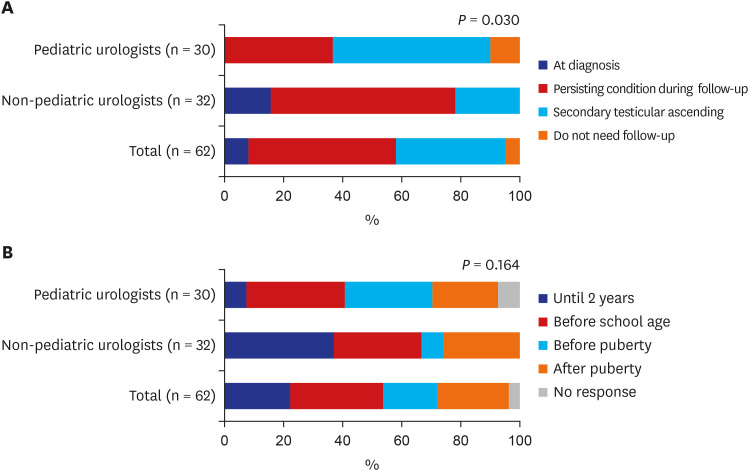
Case scenario of an infant with retractile testis
Of the 62 respondents, 54 urologists (87.1%) agreed with the diagnosis of retractile testis in this case scenario, and 22 urologists (35.5%) wanted to check an ultrasound study for further evaluation.
Only five urologists (8.1%) said that they would have performed orchiopexy immediately, but 54 (87.1%) urologists responded that they would do follow-up. None wanted to use hormone therapy. Three (4.8%) urologists said that they would no longer need to follow-up. This distribution of treatment decisions showed a statistically significant difference between the pediatric and non-pediatric urologists (
P = 0.030) (
Table 1 and
Fig. 4A).
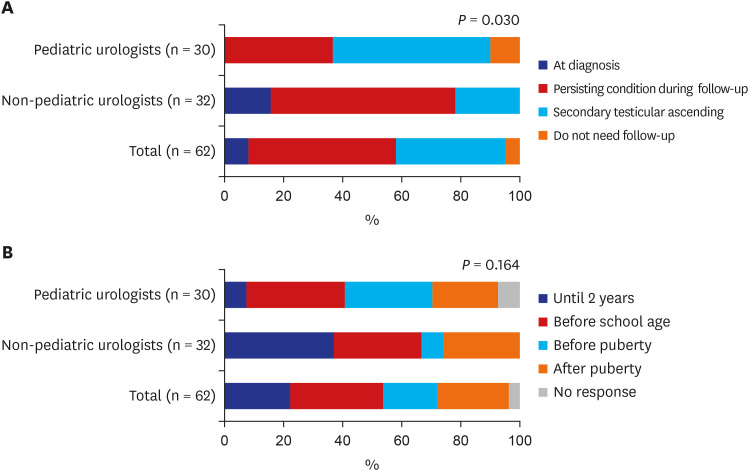 | Fig. 4Practice pattern in an infant with retractile testis. (A) Timing of orchiopexy and (B) follow-up period if orchiopexy was not performed at diagnosis.
|
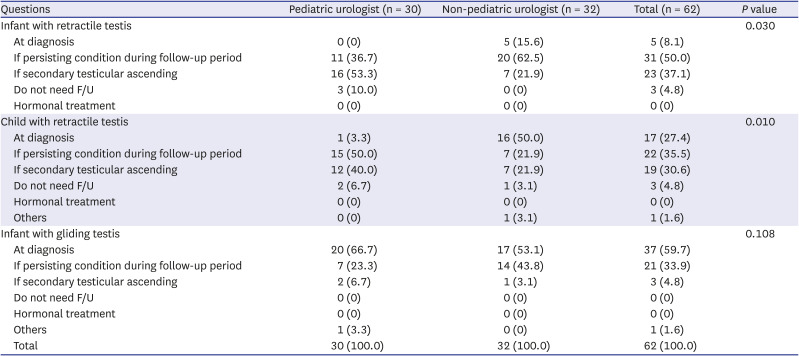
Table 1
Timing of orchiopexy
|
Questions |
Pediatric urologist (n = 30) |
Non-pediatric urologist (n = 32) |
Total (n = 62) |
P value |
|
Infant with retractile testis |
|
|
|
0.030 |
|
At diagnosis |
0 (0) |
5 (15.6) |
5 (8.1) |
|
If persisting condition during follow-up period |
11 (36.7) |
20 (62.5) |
31 (50.0) |
|
If secondary testicular ascending |
16 (53.3) |
7 (21.9) |
23 (37.1) |
|
Do not need F/U |
3 (10.0) |
0 (0) |
3 (4.8) |
|
Hormonal treatment |
0 (0) |
0 (0) |
0 (0) |
|
Child with retractile testis |
|
|
|
0.010 |
|
At diagnosis |
1 (3.3) |
16 (50.0) |
17 (27.4) |
|
If persisting condition during follow-up period |
15 (50.0) |
7 (21.9) |
22 (35.5) |
|
If secondary testicular ascending |
12 (40.0) |
7 (21.9) |
19 (30.6) |
|
Do not need F/U |
2 (6.7) |
1 (3.1) |
3 (4.8) |
|
Hormonal treatment |
0 (0) |
0 (0) |
0 (0) |
|
Others |
0 (0) |
1 (3.1) |
1 (1.6) |
|
Infant with gliding testis |
|
|
|
0.108 |
|
At diagnosis |
20 (66.7) |
17 (53.1) |
37 (59.7) |
|
If persisting condition during follow-up period |
7 (23.3) |
14 (43.8) |
21 (33.9) |
|
If secondary testicular ascending |
2 (6.7) |
1 (3.1) |
3 (4.8) |
|
Do not need F/U |
0 (0) |
0 (0) |
0 (0) |
|
Hormonal treatment |
0 (0) |
0 (0) |
0 (0) |
|
Others |
1 (3.3) |
0 (0) |
1 (1.6) |
|
Total |
30 (100.0) |
32 (100.0) |
62 (100.0) |

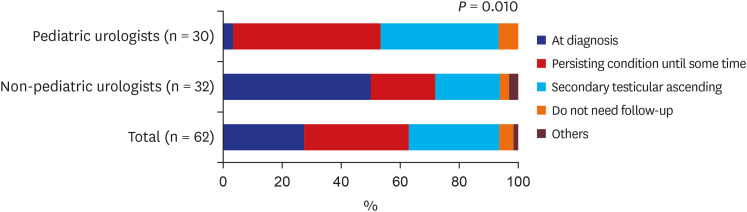
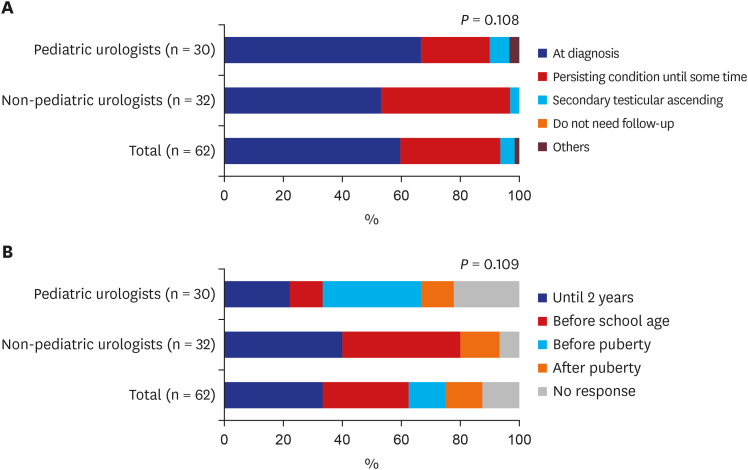
Respondents had various opinions on the follow-up period. However, there was no statistical significance between pediatric and non-pediatric urologists (
P = 0.164) (
Table 2 and
Fig. 4B).
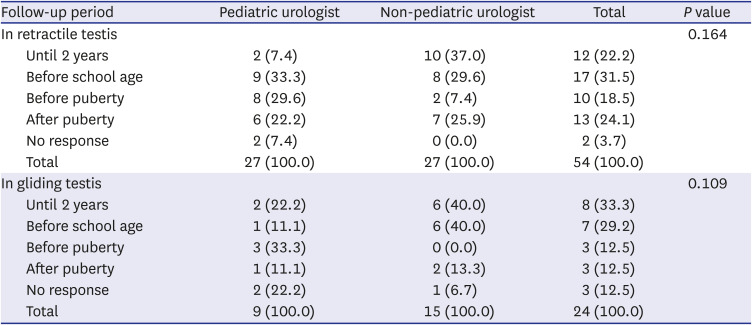
Table 2
Follow-up period if you do not perform at diagnosis
|
Follow-up period |
Pediatric urologist |
Non-pediatric urologist |
Total |
P value |
|
In retractile testis |
|
|
|
0.164 |
|
Until 2 years |
2 (7.4) |
10 (37.0) |
12 (22.2) |
|
Before school age |
9 (33.3) |
8 (29.6) |
17 (31.5) |
|
Before puberty |
8 (29.6) |
2 (7.4) |
10 (18.5) |
|
After puberty |
6 (22.2) |
7 (25.9) |
13 (24.1) |
|
No response |
2 (7.4) |
0 (0.0) |
2 (3.7) |
|
Total |
27 (100.0) |
27 (100.0) |
54 (100.0) |
|
In gliding testis |
|
|
|
0.109 |
|
Until 2 years |
2 (22.2) |
6 (40.0) |
8 (33.3) |
|
Before school age |
1 (11.1) |
6 (40.0) |
7 (29.2) |
|
Before puberty |
3 (33.3) |
0 (0.0) |
3 (12.5) |
|
After puberty |
1 (11.1) |
2 (13.3) |
3 (12.5) |
|
No response |
2 (22.2) |
1 (6.7) |
3 (12.5) |
|
Total |
9 (100.0) |
15 (100.0) |
24 (100.0) |

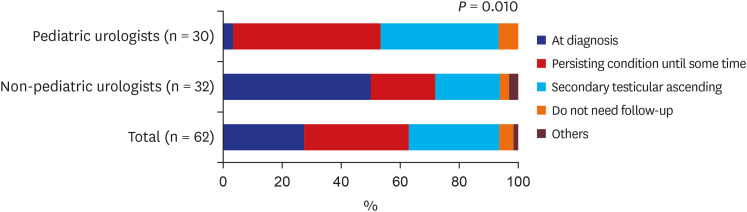
Case scenario of a 6-year-old child with retractile testis
Of the total 62 respondents, 53 urologists (85.5%) agreed with the diagnosis of retractile testis in this case scenario, and 29 urologists (46.8%) wanted an ultrasound study for further evaluation.
Seventeen urologists (27.4%) said that they would have performed orchiopexy immediately, and 41 (66.1%) urologists said that they would do a follow-up. None wanted to use hormone therapy, and three (4.8%) urologists said follow-up was no longer needed. This distribution of treatment decisions showed a statistically significant difference between pediatric and non-pediatric urologists (
P = 0.010) (
Table 1 and
Fig. 5).
 | Fig. 5Timing of orchiopexy in a child with retractile testis.
|
Case scenario of an infant with a gliding testis
Of the 62 respondents, 49 (79.0%) agreed with the diagnosis of gliding testis in this case scenario, and 36 urologists (58.1%) wanted to do an ultrasound study for further evaluation.
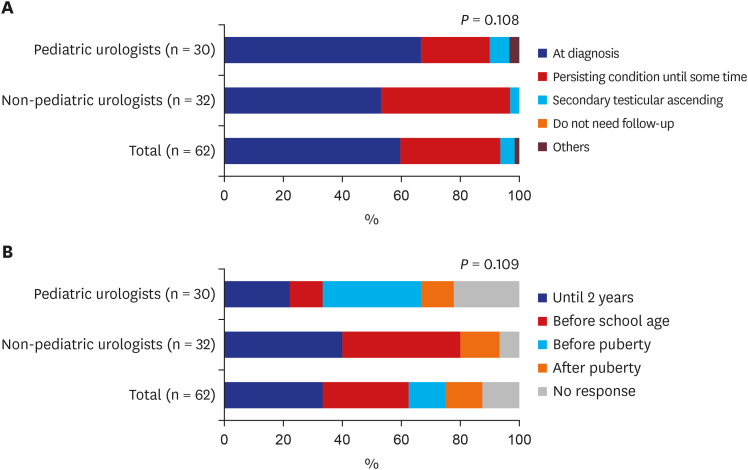
Thirty-seven urologists (59.7%) responded that they would have performed orchiopexy immediately. Twenty-four urologists (38.7%) said they would do a follow-up. None wanted to use hormone therapy or to stop following up. This distribution of treatment decisions showed no statistically significant differences between pediatric and non-pediatric urologists (
P = 0.108) (
Table 1 and
Fig. 6A).
 | Fig. 6Practice pattern in an infant with gliding testis. (A) Timing of orchiopexy and (B) follow-up period if orchiopexy was not performed at diagnosis.
|
Responses about the follow-up period showed various but statistically insignificant differences between pediatric and non-pediatric urologists (
P = 0.109) (
Table 2 and
Fig. 6B).
Summary
Scrotal ultrasound was chosen by 35.5% to 58.1% of respondents to establish a treatment plan. Immediate orchiopexy was selected by 8.1% to 59.7% of respondents. This imaging modality was frequently utilized in the order of infants with gliding testis, children with retractile testis, and infants with retractile testis. Immediate orchiopexy was frequently selected in the order of infants with gliding testis, children with retractile testis, and infants with retractile testis. Especially half of the non-pediatric urologists responded that they would have performed orchiopexy immediately even in the case of a child with retractile testis that generally does not require surgical treatment. In the case of an infant with retractile testis, 15.6% of non-pediatric urologists responded that they would have performed orchiopexy immediately.
None chose to use hormone therapy for either retractile or gliding testes. Opinions on the follow-up period for both retractile and gliding testes were inconsistent, and their responses varied.
Go to :

DISCUSSION
Although cryptorchidism is one of the most common diseases in pediatric urology, there have been no systematic investigations into the recognition and treatment of unstable high scrotal testis, such retractile or gliding testes.
Gliding testis should be clearly distinguished from retractile testis. There are many tips on how to distinguish gliding from retractile testis. Van Essen
10 described that having a patient take a squatting position on physical examination is essential in distinguishing gliding from retractile testis. Wyllie
11 stated that retractile testis could be brought into a low, stable scrotal position and that traction on the cord structures is not painful. In contrast, gliding testis can only be brought into a high unstable scrotal position, and further traction on cord structures is painful.
11 Ferro et al.
12 defines retractile testis as a phenomenon in which a testis can manipulated into the scrotum and remain in position without tension. A gliding testis is defined as when it can be manipulated into the upper scrotum, but then it retracts when released.
12 However, both are two different and distinct non-scrotal entities, and each definition is so clear, but there are many cases where it is often difficult to apply it in practice.
In the beginning, both conditions were thought to be identical, and a gliding testis was therefore also called a “pathological retractile testis”.
1314 Many studies about retractile testis could have some bias because they include some cases of gliding testis in their studies. Often it was concluded that the course of retracted testis was similar to that of cryptorchidism. It should be realized that this can create vague fears about retractile testis. However, most urologists believe that a retractile testis is a physiological variant of a fully descended testis, and therefore active treatment and long-term follow-up are usually not indicated. In contrast to a retractile testis, a gliding testis belongs to the spectrum of undescended testis. Therefore, it should be noted that retractile testis do not need surgery but indicates careful physical examinations and periodic follow-ups. However, in this study, 59.7% of urologists felt they had difficulty distinguishing retractile testis from gliding testis in the clinic setting. This rate was higher for non-pediatric urologists (78.1%) than pediatric urologists (40.0%).
The treatment for retractile testis remains controversial, whereas treatment methods for undescended testis have been well established through many studies.
151617 The most typical indication for orchidopexy is when a retractile testis has any decrease in testicular volume and when it ascends because of increased spermatic cord tension. This makes it impossible to reposition the testis into its correct anatomic location. In this study, treatment planning varied among the respondents when they had difficulty distinguishing between retractile and gliding testes in the clinic setting. They recommended follow-up or orchiopexy at a similar rate.
A retractile testis is attributed to an overactive cremasteric reflex or to alterations within the contractile properties of the cremasteric muscle.
18 It is especially common in boys around the school starting age (5–6 years).
19 Some authors have suggested that retractile testis may not be as innocuous as has been widely believed.
20 In addition, recent evidence suggests that a retractile testis may evolve into an acquired-undescended testis.
8
It has been reported that retractile testis is accompanied by histological changes. Abnormalities on semen analysis have been found during follow-up when patients with retractile testis had become adults.
2122
In this study, most of the urologists (98.4%) agreed that cryptorchidism could affect infertility and testicular function in the future. Fifty urologists (80.6%) agreed that these adverse effects were also true with gliding testis, and selected surgical treatment. The distribution of treatment decisions shows no statistically significant differences between pediatric and non-pediatric urologists (P = 0.108). Meanwhile, 13 urologists (21.0%) agreed that retractile testis lead to adverse effects, including 31.2% of non-pediatric urologists and 10% of pediatric urologists. Regarding infant with retractile testis, treatment distribution varied among groups (P = 0.030). These differences show the result of a more conservative treatment trend among pediatric urologists than in non-pediatric urologists. To overcome such discrepancies in clinical practice, it is necessary to establish an appropriate guideline for the proper management of retractile testis.
La Scala and Ein
7 reported that 150 boys with retractile testis needed periodic follow-up. In their series, only 22.7% of the patients required orchidopexy. They recommend that patients with retractile testis be attentively followed annually. They suggested that most patients with retractile testis can expect a spontaneously favorable resolution without surgical treatment, even after 14 years of age. In this study, the follow-up period in retractile and gliding testes is not clear. Half of the urologists wanted to follow-up before school age or until 2 years of age. Some urologists (12.5–24.1%) wanted to follow-up after puberty. Therefore, we need further evaluation about what is the proper follow-up period for retractile and gliding testes.
In this study, there are some limitations. This is a survey study of urologists. As a result of raising questions about the treatment trends of these urologists, we do not know if this occurs in the real clinical setting. However, we tried to elicit answers that are as realistic as possible, with scenarios for patients seen in the actual clinical field. Second, the number of respondents is small. We think it is likely that the urologists who seldom treat pediatric patients did not respond. However, we tried to include all pediatric urologists in the Korean Society of Pediatric Urology, and most members of our society participated in this survey study.
Moreover, we found some differences in practice patterns between pediatric urologists and non-pediatric urologists. Overall, non-pediatric urologists found it challenging to distinguish retractile testis from gliding testis. Compared to pediatric urologists, they had a higher tendency to agree with the statement that retractile testis could cause infertility and testicular dysfunction in the future and chose to perform orchiopexy as early as the time of the first detection. To overcome these differences, adequate education about retractile and gliding testes is essential. The results of this study are expected to be utilized as basic data for establishing a practical guideline for the diagnosis and treatment of retractile testis in Korea.
In conclusion, more than half (59.7%) of Korean urologists revealed it challenging to distinguish retractile testis and gliding testis in the clinical setting. Among urologists, non-pediatric urologists had more difficulty than pediatric urologists, and this disparity was more pronounced in children compared to infants. The more it was difficult to diagnose retractile testis with certainty, the more frequent surgical correction was chosen for treatment. Therefore, it is essential to prevent unnecessary surgical treatment by establishing consistent management plans. The results of this study are expected to be used as basic data for making a practical guideline for the diagnosis and treatment of retractile testis in Korea.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download