3. Clark JH, Pang S, Naclerio RM, Kashima M. Complications of nasal SARS-CoV-2 testing: a review. J Investig Med. 2021; 69(8):1399–1403.
4. Liu R, Han H, Liu F, Lv Z, Wu K, Liu Y, et al. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin Chim Acta. 2020; 505:172–175. PMID:
32156607.
5. Okoye GA, Kamara HI, Strobeck M, Mellman TA, Kwagyan J, Sullivan A, et al. Diagnostic accuracy of a rapid diagnostic test for the early detection of COVID-19. J Clin Virol. 2022; 147:105023. PMID:
35121489.
6. Wölfl-Duchek M, Bergmann F, Jorda A, Weber M, Müller M, Seitz T, et al. Sensitivity and specificity of SARS-CoV-2 rapid antigen detection tests using oral, anterior nasal, and nasopharyngeal swabs: a diagnostic accuracy study. Microbiol Spectr. 2022; 10(1):e0202921. PMID:
35107327.
7. Barton RT. Q-tip otalgia. JAMA. 1972; 220(12):1619.
8. Smith M, Darrat I, Seidman M. Otologic complications of cotton swab use: one institution’s experience. Laryngoscope. 2012; 122(2):409–411. PMID:
22241624.
9. Bwire GM, Majigo MV, Njiro BJ, Mawazo A. Detection profile of SARS-CoV-2 using RT-PCR in different types of clinical specimens: a systematic review and meta-analysis. J Med Virol. 2021; 93(2):719–725. PMID:
32706393.
10. Lee RA, Herigon JC, Benedetti A, Pollock NR, Denkinger CM. Performance of saliva, oropharyngeal swabs, and nasal swabs for SARS-CoV-2 molecular detection: a systematic review and meta-analysis. J Clin Microbiol. 2021; 59(5):e02881-20. PMID:
33504593.
11. Agamawi YM, Namin A, Ducic Y. Cerebrospinal fluid leak from COVID-19 swab. OTO Open. 2021; 5(4):2473974X211059104.
12. Hakimi AA, Goshtasbi K, Kuan EC. Complications associated with nasopharyngeal COVID-19 testing: an analysis of the MAUDE database and literature review. Am J Rhinol Allergy. 2022; 36(2):281–284. PMID:
34547903.
15. Alberola-Amores FJ, Valdeolivas-Urbelz E, Torregrosa-Ortiz M, Álvarez-Sauco M, Alom-Poveda J. Meningitis due to cerebrospinal fluid leak after nasal swab testing for COVID-19. Eur J Neurol. 2021; 28(11):e91–e92. PMID:
33480112.
16. De Luca L, Maltoni S. Is naso-pharyngeal swab always safe for SARS-CoV-2 testing? An unusual, accidental foreign body swallowing. Clin J Gastroenterol. 2021; 14(1):44–47. PMID:
32951147.
17. Fabbris C, Cestaro W, Menegaldo A, Spinato G, Frezza D, Vijendren A, et al. Is oro/nasopharyngeal swab for SARS-CoV-2 detection a safe procedure? Complications observed among a case series of 4876 consecutive swabs. Am J Otolaryngol. 2021; 42(1):102758. PMID:
33125901.
18. Farina DA, Nelson KK. How deep is too deep? Gastrointestinal complication of COVID-19 deep nasal swab testing. Endosc Int Open. 2021; 9(11):E1841–E1842. PMID:
34790553.
19. Fazekas B, Fazekas B, Darraj E, Jayakumar D. Preseptal cellulitis and infraorbital abscess as a complication of a routine COVID-19 swab. BMJ Case Rep. 2021; 14(5):e241963.
20. Föh B, Borsche M, Balck A, Taube S, Rupp J, Klein C, et al. Complications of nasal and pharyngeal swabs: a relevant challenge of the COVID-19 pandemic? Eur Respir J. 2021; 57(4):2004004. PMID:
33303542.
21. Gaffuri M, Capaccio P, Torretta S, Daga M, Zuccotti GV, Pignataro L. An unusual retained choanal foreign body: a possible complication of COVID-19 testing with nasopharyngeal swab. Ear Nose Throat J. Forthcoming. 2021; DOI:
10.1177/0145561321993933.
22. Holmes A, Allen B. Case report: an intracranial complication of COVID-19 nasopharyngeal swab. Clin Pract Cases Emerg Med. 2021; 5(3):341–344. PMID:
34437043.
23. Knížek Z, Michálek R, Vodicka J, Zdobinská P. Cribriform plate injury after nasal swab testing for COVID-19. JAMA Otolaryngol Head Neck Surg. 2021; 147(10):915–917. PMID:
34499106.
24. Koskinen A, Tolvi M, Jauhiainen M, Kekäläinen E, Laulajainen-Hongisto A, Lamminmäki S. Complications of COVID-19 nasopharyngeal swab test. JAMA Otolaryngol Head Neck Surg. 2021; 147(7):672–674. PMID:
33914064.
25. Lapeyre M, Coupez E, Ghelis N, Dupuis C. Pharyngeal abscess: a rare complication of repeated nasopharyngeal swabs. Intensive Care Med. 2021; 47(5):612–613. PMID:
33547902.
26. Molnár D, Zsigmond F, Helfferich F. Safety precautions for self-performed severe acute respiratory syndrome coronavirus 2 tests: a case of a swallowed swab. Cureus. 2021; 13(5):e15297. PMID:
34221756.
27. Mughal Z, Luff E, Okonkwo O, Hall CE. Test, test, test - a complication of testing for coronavirus disease 2019 with nasal swabs. J Laryngol Otol. 2020; 134(7):646–649. PMID:
32641170.
28. Ovenden C, Bulshara V, Patel S, Vsykocil E, Valentine R, Psaltis A, et al. COVID-19 nasopharyngeal swab causing a traumatic cerebrospinal fluid leak. ANZ J Surg. 2021; 91(5):1021–1022. PMID:
33890357.
29. Paquin R, Ryan L, Vale FL, Rutkowski M, Byrd JK. CSF leak after COVID-19 nasopharyngeal swab: a case report. Laryngoscope. 2021; 131(9):1927–1929. PMID:
33577104.
30. Rajah J, Lee J. CSF rhinorrhoea post COVID-19 swab: a case report and review of literature. J Clin Neurosci. 2021; 86:6–9. PMID:
33775348.
31. Ribeiro SP, Loureiro RM, Gil JM, Dutra DL, Gomes RL, Daniel MM. Ethmoidal silent sinus syndrome after nasal swab test. Neuroradiology. 2022; 64(1):205–207. PMID:
34773478.
32. Rigante M, Picciotti PM, Parrilla C. A nasal complication of nasopharyngeal swab for reverse transcription polymerase chain reaction (RT-PCR) detection of SARS-CoV-2 mRNA. Cureus. 2021; 13(7):e16183. PMID:
34367790.
33. Samadian M, Maroufi SF, Taheri MS, Jafari A. CSF rhinorrhea after nasopharyngeal swab testing for COVID-19: a case report and review of literature. Otolaryngol Case Rep. 2021; 21:100370. PMID:
34957364.
34. Sullivan CB, Schwalje AT, Jensen M, Li L, Dlouhy BJ, Greenlee JD, et al. Cerebrospinal fluid leak after nasal swab testing for coronavirus disease 2019. JAMA Otolaryngol Head Neck Surg. 2020; 146(12):1179–1181. PMID:
33022069.
35. Tümer M, Ardıçlı B. A fractured nasopharyngeal swab in the duodenum of a toddler: an unusual complication of preoperative COVID-19 testing. Can J Anaesth. 2021; 68(9):1450–1451. PMID:
33880727.
36. Yılmaz M, Bahadır Z, Madendere B, Yüksel RT, Gökay H, Yiğitbaşı AA. A brief report: cerebrospinal fluid rhinorrhea after repetitive nasal swab testing for coronavirus disease 2019(COVID-19). Otolaryngol Case Rep. 2021; 20:100313. PMID:
34957362.
37. Cheong HS, Kwon KT, Hwang S, Kim SW, Chang HH, Park SY, et al. Workload of healthcare workers during the COVID-19 outbreak in Korea: a nationwide survey. J Korean Med Sci. 2022; 37(6):e49. PMID:
35166085.
38. Lee HA, Ahn MH, Byun S, Lee HK, Kweon YS, Chung S, et al. How COVID-19 affected healthcare workers in the hospital locked down due to early COVID-19 cases in Korea. J Korean Med Sci. 2021; 36(47):e325. PMID:
34873888.
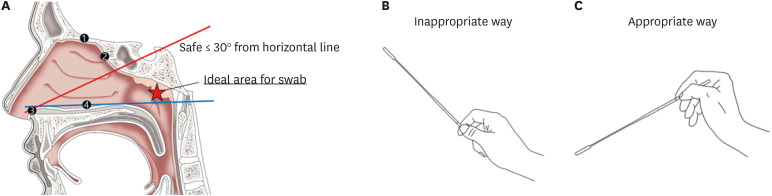
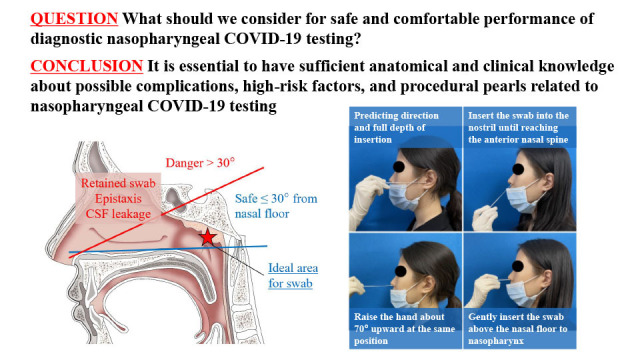
39. Li L, Shim T, Zapanta PE. Optimization of COVID-19 testing accuracy with nasal anatomy education. Am J Otolaryngol. 2021; 42(1):102777. PMID:
33125907.
40. May J, Mason K, Patel P, Madden B. A challenging case of tracheal foreign body retrieval following COVID-19 swabbing. Monaldi Arch Chest Dis. Forthcoming. 2021; DOI:
10.4081/monaldi.2021.2014.
41. Roque M, Proudfoot K, Mathys V, Yu S, Krieger N, Gernon T, et al. A review of nasopharyngeal swab and saliva tests for SARS-CoV-2 infection: disease timelines, relative sensitivities, and test optimization. J Surg Oncol. 2021; 124(4):465–475. PMID:
34091905.
42. Butler-Laporte G, Lawandi A, Schiller I, Yao M, Dendukuri N, McDonald EG, et al. Comparison of saliva and nasopharyngeal swab nucleic acid amplification testing for detection of SARS-CoV-2: a systematic review and meta-analysis. JAMA Intern Med. 2021; 181(3):353–360. PMID:
33449069.
43. Matti E, Lizzio R, Spinozzi G, Ugolini S, Maiorano E, Benazzo M, et al. An alternative way to perform diagnostic nasopharyngeal swab for SARS-CoV-2 infection. Am J Otolaryngol. 2021; 42(2):102828. PMID:
33234296.
44. Février E, Vandersteen C, Castillo L, Savoldelli C. Silent sinus syndrome: a traumatic case. J Stomatol Oral Maxillofac Surg. 2017; 118(3):187–190. PMID:
28411135.
45. Mistry SG, Walker W, Earnshaw J, Cervin A. COVID-19 swab-related skull base injury. Med J Aust. 2021; 214(10):457–459.e1. PMID:
34008200.
46. Marty FM, Chen K, Verrill KA. How to obtain a nasopharyngeal swab specimen. N Engl J Med. 2020; 382(22):e76. PMID:
32302471.
47. Di Maio P, Iocca O, Cavallero A, Giudice M. Performing the nasopharyngeal and oropharyngeal swab for 2019-novel coronavirus (SARS-CoV-2) safely: How to dress, undress, and technical notes. Head Neck. 2020; 42(7):1548–1551. PMID:
32357377.
48. Petruzzi G, De Virgilio A, Pichi B, Mazzola F, Zocchi J, Mercante G, et al. COVID-19: nasal and oropharyngeal swab. Head Neck. 2020; 42(6):1303–1304. PMID:
32352180.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download