|
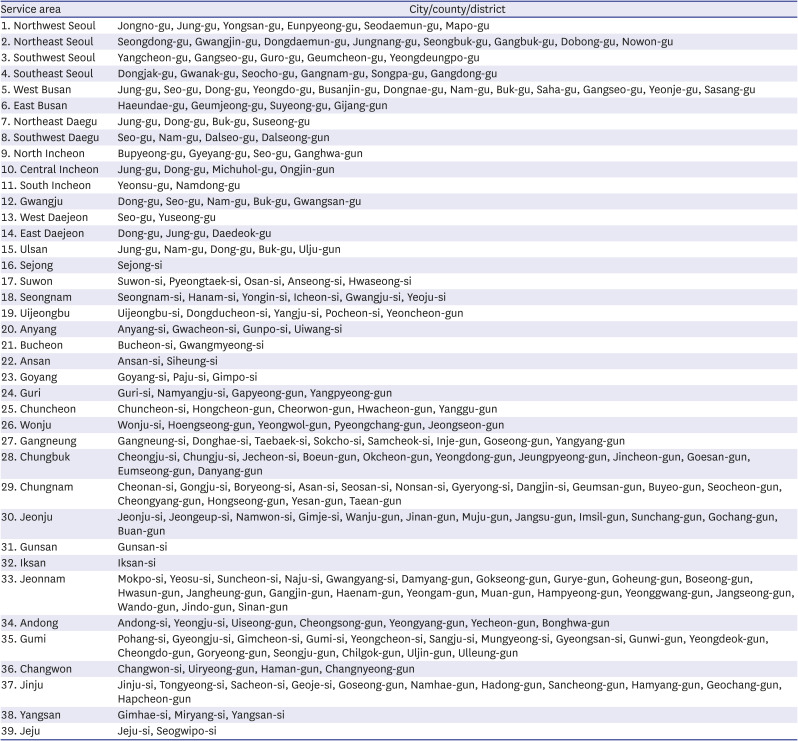
1. Northwest Seoul |
Jongno-gu, Jung-gu, Yongsan-gu, Eunpyeong-gu, Seodaemun-gu, Mapo-gu |
|
2. Northeast Seoul |
Seongdong-gu, Gwangjin-gu, Dongdaemun-gu, Jungnang-gu, Seongbuk-gu, Gangbuk-gu, Dobong-gu, Nowon-gu |
|
3. Southwest Seoul |
Yangcheon-gu, Gangseo-gu, Guro-gu, Geumcheon-gu, Yeongdeungpo-gu |
|
4. Southeast Seoul |
Dongjak-gu, Gwanak-gu, Seocho-gu, Gangnam-gu, Songpa-gu, Gangdong-gu |
|
5. West Busan |
Jung-gu, Seo-gu, Dong-gu, Yeongdo-gu, Busanjin-gu, Dongnae-gu, Nam-gu, Buk-gu, Saha-gu, Gangseo-gu, Yeonje-gu, Sasang-gu |
|
6. East Busan |
Haeundae-gu, Geumjeong-gu, Suyeong-gu, Gijang-gun |
|
7. Northeast Daegu |
Jung-gu, Dong-gu, Buk-gu, Suseong-gu |
|
8. Southwest Daegu |
Seo-gu, Nam-gu, Dalseo-gu, Dalseong-gun |
|
9. North Incheon |
Bupyeong-gu, Gyeyang-gu, Seo-gu, Ganghwa-gun |
|
10. Central Incheon |
Jung-gu, Dong-gu, Michuhol-gu, Ongjin-gun |
|
11. South Incheon |
Yeonsu-gu, Namdong-gu |
|
12. Gwangju |
Dong-gu, Seo-gu, Nam-gu, Buk-gu, Gwangsan-gu |
|
13. West Daejeon |
Seo-gu, Yuseong-gu |
|
14. East Daejeon |
Dong-gu, Jung-gu, Daedeok-gu |
|
15. Ulsan |
Jung-gu, Nam-gu, Dong-gu, Buk-gu, Ulju-gun |
|
16. Sejong |
Sejong-si |
|
17. Suwon |
Suwon-si, Pyeongtaek-si, Osan-si, Anseong-si, Hwaseong-si |
|
18. Seongnam |
Seongnam-si, Hanam-si, Yongin-si, Icheon-si, Gwangju-si, Yeoju-si |
|
19. Uijeongbu |
Uijeongbu-si, Dongducheon-si, Yangju-si, Pocheon-si, Yeoncheon-gun |
|
20. Anyang |
Anyang-si, Gwacheon-si, Gunpo-si, Uiwang-si |
|
21. Bucheon |
Bucheon-si, Gwangmyeong-si |
|
22. Ansan |
Ansan-si, Siheung-si |
|
23. Goyang |
Goyang-si, Paju-si, Gimpo-si |
|
24. Guri |
Guri-si, Namyangju-si, Gapyeong-gun, Yangpyeong-gun |
|
25. Chuncheon |
Chuncheon-si, Hongcheon-gun, Cheorwon-gun, Hwacheon-gun, Yanggu-gun |
|
26. Wonju |
Wonju-si, Hoengseong-gun, Yeongwol-gun, Pyeongchang-gun, Jeongseon-gun |
|
27. Gangneung |
Gangneung-si, Donghae-si, Taebaek-si, Sokcho-si, Samcheok-si, Inje-gun, Goseong-gun, Yangyang-gun |
|
28. Chungbuk |
Cheongju-si, Chungju-si, Jecheon-si, Boeun-gun, Okcheon-gun, Yeongdong-gun, Jeungpyeong-gun, Jincheon-gun, Goesan-gun, Eumseong-gun, Danyang-gun |
|
29. Chungnam |
Cheonan-si, Gongju-si, Boryeong-si, Asan-si, Seosan-si, Nonsan-si, Gyeryong-si, Dangjin-si, Geumsan-gun, Buyeo-gun, Seocheon-gun, Cheongyang-gun, Hongseong-gun, Yesan-gun, Taean-gun |
|
30. Jeonju |
Jeonju-si, Jeongeup-si, Namwon-si, Gimje-si, Wanju-gun, Jinan-gun, Muju-gun, Jangsu-gun, Imsil-gun, Sunchang-gun, Gochang-gun, Buan-gun |
|
31. Gunsan |
Gunsan-si |
|
32. Iksan |
Iksan-si |
|
33. Jeonnam |
Mokpo-si, Yeosu-si, Suncheon-si, Naju-si, Gwangyang-si, Damyang-gun, Gokseong-gun, Gurye-gun, Goheung-gun, Boseong-gun, Hwasun-gun, Jangheung-gun, Gangjin-gun, Haenam-gun, Yeongam-gun, Muan-gun, Hampyeong-gun, Yeonggwang-gun, Jangseong-gun, Wando-gun, Jindo-gun, Sinan-gun |
|
34. Andong |
Andong-si, Yeongju-si, Uiseong-gun, Cheongsong-gun, Yeongyang-gun, Yecheon-gun, Bonghwa-gun |
|
35. Gumi |
Pohang-si, Gyeongju-si, Gimcheon-si, Gumi-si, Yeongcheon-si, Sangju-si, Mungyeong-si, Gyeongsan-si, Gunwi-gun, Yeongdeok-gun, Cheongdo-gun, Goryeong-gun, Seongju-gun, Chilgok-gun, Uljin-gun, Ulleung-gun |
|
36. Changwon |
Changwon-si, Uiryeong-gun, Haman-gun, Changnyeong-gun |
|
37. Jinju |
Jinju-si, Tongyeong-si, Sacheon-si, Geoje-si, Goseong-gun, Namhae-gun, Hadong-gun, Sancheong-gun, Hamyang-gun, Geochang-gun, Hapcheon-gun |
|
38. Yangsan |
Gimhae-si, Miryang-si, Yangsan-si |
|
39. Jeju |
Jeju-si, Seogwipo-si |




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download