METHODS
Study population
Newly diagnosed IPAH data from KNHIS records from 2006 through 2017 were collected (N = 9,017). Associated pulmonary hypertension data were excluded, and only IPAH patients were included per the Updated Clinical Classification of Pulmonary Hypertension.
1 The data contain primary diagnoses related to IPAH according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10 code I27.0).
KNHIS database
The KNHIS database for health insurance subscribers and Medicare recipients consists of the following four databases: 1) qualification database, 2) medical check-up database, 3) medical institution database, and 4) treatment database. The treatment database has four subcategories of medicine, dentistry, oriental medicine, and pharmacy of which we only used records from the medicine subcategory. Additionally, we used variables from the qualification database in conjunction with the treatment database.
23
Definition of variables
Age groups were defined as 0–9 years, 10–19 years, 20–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, and 80 years or older. Socioeconomic factors included percentile group of income level using the National Health Insurance Premium database divided into 20 quartiles. Income level was categorized as upper, medium, and lower.
Comorbidities
We defined comorbidities from diagnoses in patients with IPAH: essential hypertension (hypertension, ICD-10 codes I10, I11, I12, I13, and I15); diabetes mellitus (ICD-10 codes E10, E11 E12, E13, and E14); myocardial infarction (ICD-10 codes I21, I22, and I25.2); atrial fibrillation (ICD-10 code I48); ischemic stroke (ICD-10 codes I63 and I64); hemorrhagic stroke (ICD-10 codes I60, I61, and I62); transient ischemic attack (ICD-10 code G45); and malignant neoplasm (ICD-10 codes C00 to C97).
Death data
We employed the death data of Korean people from 2006 through 2018 in this study. We received only information on the cause of death and the date of death from the Korea Statistics Promotion Institute in accordance with official protocols.
3
Cause of death
IPAH is a rare disease, and there are limitations on the use and disclosure of health data due to concerns about the exposure of personal information. Thus, we categorized reported the causes of death into groups of ICD-10 codes, evaluating the primary cause of death as one of the following: certain infections and parasitic diseases (ICD-10 codes A00–B99); malignant neoplasms (ICD-10 codes C00–C97); benign neoplasm (ICD-10 codes D00–D48) & diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (ICD-10 codes D50–D89); endocrine, nutritional, and metabolic diseases (ICD-10 codes E00–E90); mental and behavioral disorders (ICD-10 codes F01–F99); diseases of the nervous system (ICD-10 codes G00–G98); diseases of the circulatory system (ICD-10 codes I00–I99); diseases of the respiratory system (ICD-10 codes J00–J98); diseases of the digestive system (ICD-10 codes K00–K92); diseases of the skin and subcutaneous tissue (ICD-10 codes L00–L99); diseases of the musculoskeletal system and connective tissue (ICD-10 codes M00–M99); diseases of the genitourinary system (ICD-10 codes N00–N99); pregnancy, childbirth and the puerperium (ICD-10 codes O00–O99); certain conditions originating in the perinatal period (ICD-10 codes P00–P96); congenital malformations, deformations and chromosomal abnormalities (ICD-10 codes Q00–Q99); symptoms, signs, and abnormal clinical and laboratory findings, that are not elsewhere classified elsewhere (ICD-10 codes R00–R99); injury, poisoning, and certain other consequences of external causes (ICD-10 codes S00–T98); and not provided.
Statistical analysis
Differences in age, comorbidities, and cause of death by sex were analyzed using the Student’s t-test for continuous variables and the χ2-test for categorical variables. The Kaplan–Meier method was also used to compare SRs among patients with IPAH, by sex, and by age group using the log-rank test or Wilcoxon test. Simple and multiple Cox proportional-hazards analyses were carried out using the variables of age, sex, income level, and comorbidities (hypertension, diabetes mellitus, myocardial infarction, atrial fibrillation, ischemic stroke, hemorrhagic stroke, transient ischemic attack, and malignant neoplasm).
Ethics statement
Evaluation of the study protocol was approved and patient consent was exempted by the Institutional Review Board (IRB) of Samsung Medical Center (IRB file no. 2017-02-032). We used secondary processed national big data. The exemption of consent does not adversely affect the rights or well-being of the study subjects.
RESULTS
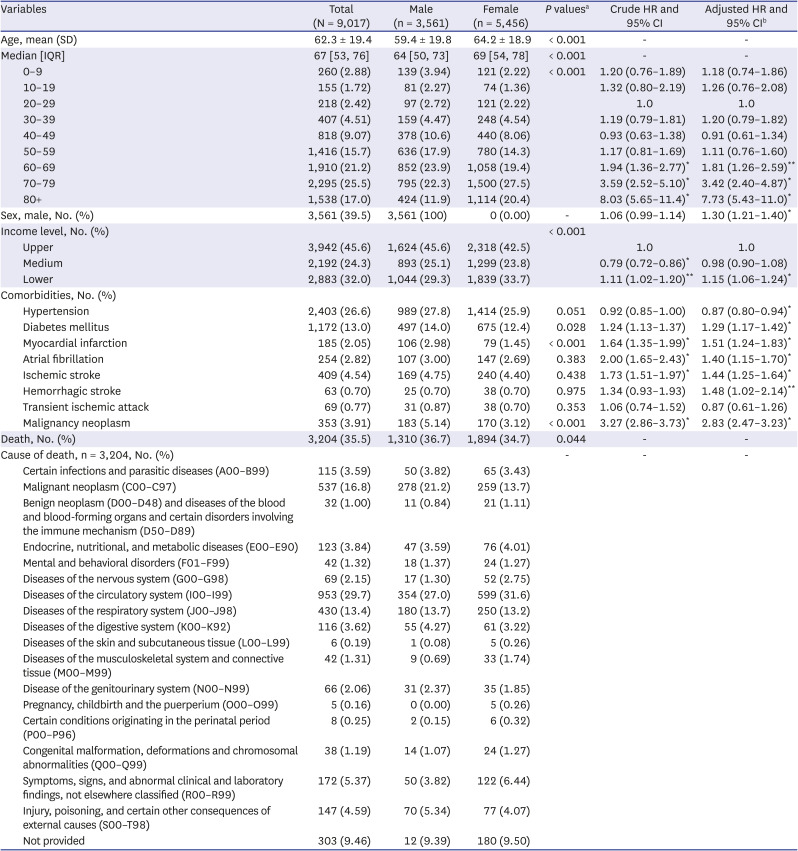
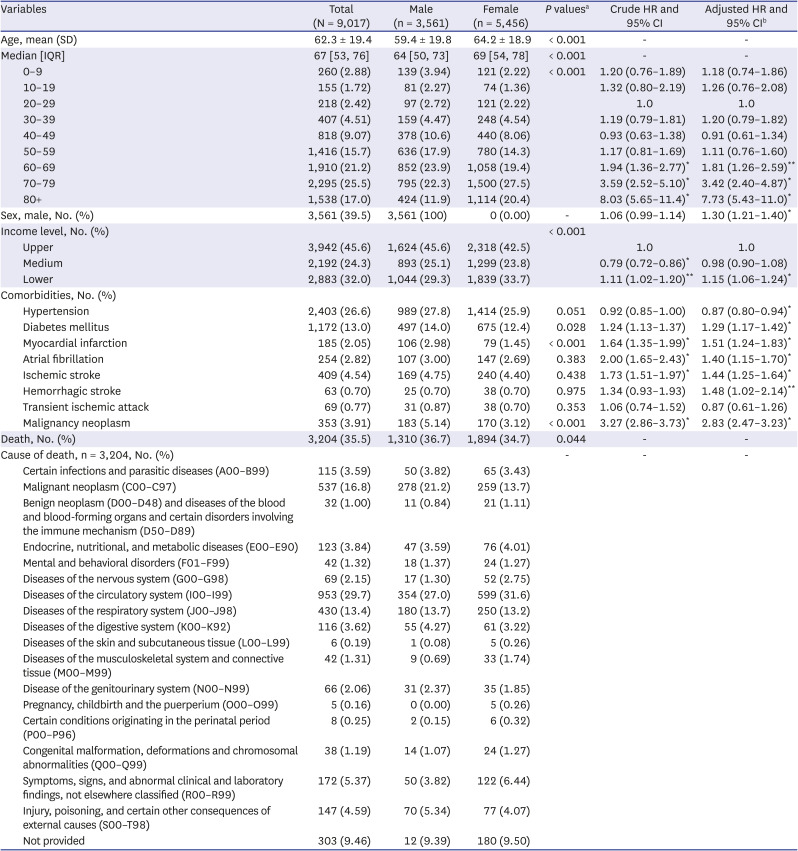
The mean (± standard deviation) age of the whole study population was 62.3 (± 19.4) years and was 64.2 (± 18.9) years and 59.4 (± 19.8) years among females and males (
P < 0.001), respectively. The female-to-male ratio of the study population was 6:4. The distribution of newly diagnosed IPAH patients by age group was as follows: 2.88% in the group 0–9 years, 1.72% in 10–19, 2.42% in 20–29, 4.51% in 30–39, 9.07% in 40–49, 15.7% in 50–59, 21.2% in 60–69, 25.5% in 70–79, and 17.0% in 80 or older (
P < 0.001). The overall proportion of death among participants with IPAH was 35.5%. The three most common causes of death in patients with IPAH were diseases of the circulatory system (29.7%), malignant neoplasm (16.8%), and diseases of the respiratory system (13.4%). Adjusted hazard ratios (HRs) of IPAH was were 1.81 (95% confidence interval [CI], 1.26–2.59) in the 60–69, 3.42 (95% CI, 2.40–4.87) in 70–79, 7.73 (95% CI, 5.43–11.0) in 80 or older, 1.30 (95% CI, 1.21–1.40) among male patients, 1.15 (95% CI, 1.06–1.24) in the low socioeconomic group, 0.87 (95% CI, 0.80–0.94) in the hypertensive group, 1.29 (95% CI, 1.17–1.42) in the diabetes mellitus group, 1.51 (95% CI, 1.24–1.83) in the prior myocardial infarction group, 1.40 (95% CI, 1.15–1.70) in the atrial fibrillation group, 1.44 (95% CI, 1.25–1.64) in the prior ischemic stroke group, 1.48 (95% CI, 1.02–2.14) in the prior hemorrhagic stroke group, and 2.83 (95% CI, 2.47–3.23) in the malignant neoplasm group (
Table 1).
Table 1
The distribution of general characteristics, comorbidities, and causes of death in IPAH by sex and death risk for IPAH
|
Variables |
Total (N = 9,017) |
Male (n = 3,561) |
Female (n = 5,456) |
P valuesa
|
Crude HR and 95% CI |
Adjusted HR and 95% CIb
|
|
Age, mean (SD) |
62.3 ± 19.4 |
59.4 ± 19.8 |
64.2 ± 18.9 |
< 0.001 |
- |
- |
|
Median [IQR] |
67 [53, 76] |
64 [50, 73] |
69 [54, 78] |
< 0.001 |
- |
- |
|
0–9 |
260 (2.88) |
139 (3.94) |
121 (2.22) |
< 0.001 |
1.20 (0.76–1.89) |
1.18 (0.74–1.86) |
|
10–19 |
155 (1.72) |
81 (2.27) |
74 (1.36) |
1.32 (0.80–2.19) |
1.26 (0.76–2.08) |
|
20–29 |
218 (2.42) |
97 (2.72) |
121 (2.22) |
1.0 |
1.0 |
|
30–39 |
407 (4.51) |
159 (4.47) |
248 (4.54) |
1.19 (0.79–1.81) |
1.20 (0.79–1.82) |
|
40–49 |
818 (9.07) |
378 (10.6) |
440 (8.06) |
0.93 (0.63–1.38) |
0.91 (0.61–1.34) |
|
50–59 |
1,416 (15.7) |
636 (17.9) |
780 (14.3) |
1.17 (0.81–1.69) |
1.11 (0.76–1.60) |
|
60–69 |
1,910 (21.2) |
852 (23.9) |
1,058 (19.4) |
1.94 (1.36–2.77)*
|
1.81 (1.26–2.59)**
|
|
70–79 |
2,295 (25.5) |
795 (22.3) |
1,500 (27.5) |
3.59 (2.52–5.10)*
|
3.42 (2.40–4.87)*
|
|
80+ |
1,538 (17.0) |
424 (11.9) |
1,114 (20.4) |
8.03 (5.65–11.4)*
|
7.73 (5.43–11.0)*
|
|
Sex, male, No. (%) |
3,561 (39.5) |
3,561 (100) |
0 (0.00) |
- |
1.06 (0.99–1.14) |
1.30 (1.21–1.40)*
|
|
Income level, No. (%) |
|
|
|
< 0.001 |
|
|
|
Upper |
3,942 (45.6) |
1,624 (45.6) |
2,318 (42.5) |
1.0 |
1.0 |
|
Medium |
2,192 (24.3) |
893 (25.1) |
1,299 (23.8) |
0.79 (0.72–0.86)*
|
0.98 (0.90–1.08) |
|
Lower |
2,883 (32.0) |
1,044 (29.3) |
1,839 (33.7) |
1.11 (1.02–1.20)**
|
1.15 (1.06–1.24)*
|
|
Comorbidities, No. (%) |
|
|
|
|
|
|
|
Hypertension |
2,403 (26.6) |
989 (27.8) |
1,414 (25.9) |
0.051 |
0.92 (0.85–1.00) |
0.87 (0.80–0.94)*
|
|
Diabetes mellitus |
1,172 (13.0) |
497 (14.0) |
675 (12.4) |
0.028 |
1.24 (1.13–1.37) |
1.29 (1.17–1.42)*
|
|
Myocardial infarction |
185 (2.05) |
106 (2.98) |
79 (1.45) |
< 0.001 |
1.64 (1.35–1.99)*
|
1.51 (1.24–1.83)*
|
|
Atrial fibrillation |
254 (2.82) |
107 (3.00) |
147 (2.69) |
0.383 |
2.00 (1.65–2.43)*
|
1.40 (1.15–1.70)*
|
|
Ischemic stroke |
409 (4.54) |
169 (4.75) |
240 (4.40) |
0.438 |
1.73 (1.51–1.97)*
|
1.44 (1.25–1.64)*
|
|
Hemorrhagic stroke |
63 (0.70) |
25 (0.70) |
38 (0.70) |
0.975 |
1.34 (0.93–1.93) |
1.48 (1.02–2.14)**
|
|
Transient ischemic attack |
69 (0.77) |
31 (0.87) |
38 (0.70) |
0.353 |
1.06 (0.74–1.52) |
0.87 (0.61–1.26) |
|
Malignancy neoplasm |
353 (3.91) |
183 (5.14) |
170 (3.12) |
< 0.001 |
3.27 (2.86–3.73)*
|
2.83 (2.47–3.23)*
|
|
Death, No. (%) |
3,204 (35.5) |
1,310 (36.7) |
1,894 (34.7) |
0.044 |
- |
- |
|
Cause of death, n = 3,204, No. (%) |
|
|
|
- |
- |
- |
|
Certain infections and parasitic diseases (A00–B99) |
115 (3.59) |
50 (3.82) |
65 (3.43) |
|
Malignant neoplasm (C00–C97) |
537 (16.8) |
278 (21.2) |
259 (13.7) |
|
Benign neoplasm (D00–D48) and diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50–D89) |
32 (1.00) |
11 (0.84) |
21 (1.11) |
|
Endocrine, nutritional, and metabolic diseases (E00–E90) |
123 (3.84) |
47 (3.59) |
76 (4.01) |
|
Mental and behavioral disorders (F01–F99) |
42 (1.32) |
18 (1.37) |
24 (1.27) |
|
Diseases of the nervous system (G00–G98) |
69 (2.15) |
17 (1.30) |
52 (2.75) |
|
Diseases of the circulatory system (I00–I99) |
953 (29.7) |
354 (27.0) |
599 (31.6) |
|
Diseases of the respiratory system (J00–J98) |
430 (13.4) |
180 (13.7) |
250 (13.2) |
|
Diseases of the digestive system (K00–K92) |
116 (3.62) |
55 (4.27) |
61 (3.22) |
|
Diseases of the skin and subcutaneous tissue (L00–L99) |
6 (0.19) |
1 (0.08) |
5 (0.26) |
|
Diseases of the musculoskeletal system and connective tissue (M00–M99) |
42 (1.31) |
9 (0.69) |
33 (1.74) |
|
Disease of the genitourinary system (N00–N99) |
66 (2.06) |
31 (2.37) |
35 (1.85) |
|
Pregnancy, childbirth and the puerperium (O00–O99) |
5 (0.16) |
0 (0.00) |
5 (0.26) |
|
Certain conditions originating in the perinatal period (P00–P96) |
8 (0.25) |
2 (0.15) |
6 (0.32) |
|
Congenital malformation, deformations and chromosomal abnormalities (Q00–Q99) |
38 (1.19) |
14 (1.07) |
24 (1.27) |
|
Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99) |
172 (5.37) |
50 (3.82) |
122 (6.44) |
|
Injury, poisoning, and certain other consequences of external causes (S00–T98) |
147 (4.59) |
70 (5.34) |
77 (4.07) |
|
Not provided |
303 (9.46) |
12 (9.39) |
180 (9.50) |

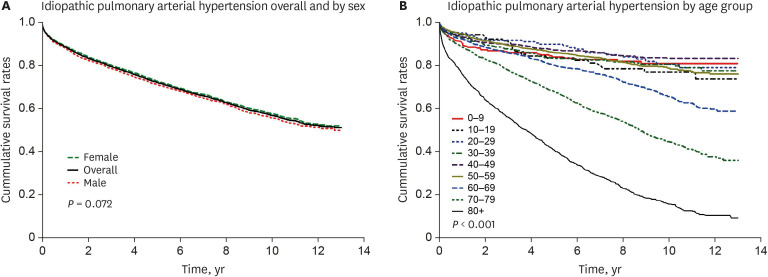
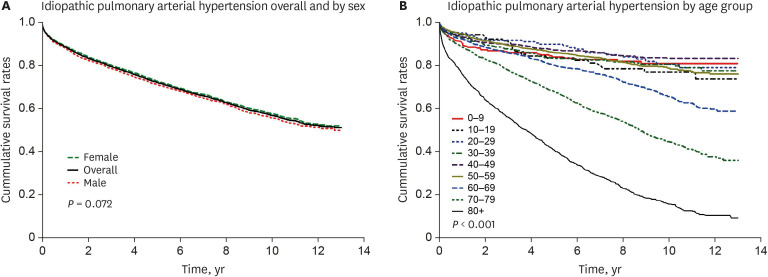
The one-, three-, five-, and 10-year SRs of IPAH were 89.0%, 79.8%, 72.3%, and 57.0%, respectively. The one-, three-, five-, and 10-year SRs by sex were 89.4%, 80.4%, 72.9%, and 57.8%, respectively among women and 88.4%, 78.9%, 71.3%, and 55.9% among men (
P = 0.072). The one-, three-, five-, and 10-year SRs were 92.1%, 85.8%, 80.0%, and 65.3%, respectively in the 60–69 age group; 88.4%, 77.6%, 67.6%, and 44.5%, respectively in the 70-79; and 75.9%, 55.8%, 40.5%, and 15.6%, respectively in 80 years or older (
P < 0.001) (
Fig. 1 and
Supplementary Table 1).
Fig. 1
Survival curve of idiopathic pulmonary arterial hypertension (IPAH) in Koreans. (A)
Survival rates overall and by sex and (B) by age group.

DISCUSSION
The present study showed that the one-, three-, and five-year SRs for IPAH were 89.0%, 79.8%, and 72.3%, while the 10-year SRs was 57.0%. Our one- and three-year SRs correspond well with those of other studies, including 91% and 74% in 1,201 IPAH patients from the REVEAL registry, United States (US), recorded from 2006 to 2009
4; 89% and 76% in German IPAH patients from the Giessen pulmonary hypertension registry recorded from 1993 to 2011
5; 89% and 77% in 314 IPAH patients from the Spanish registry recorded from 2007 to 2008
6; 88% and 73.3% in 174 adults Lavitian PAH patients recorded from 2007 to 2016
7; 95.6% and 87.3% in 220 patients from the Pulmonary Hypertension Society of Australian and New Zealand (PHSANZ) registry recorded from 2011 to 2016
8; and 97.9% and 92.1% in 141 Japanese IPAH patients recorded from 1992 to 2012.
9 However, the five-year SRs in the aforementioned studies, including a Switzerland PAH study performed from 1994 to 2004
10 and excluding the PHSANZ registry
8 and Japanese study,
9 were around 60%.
It’s hard to explain why the aforementioned studies from the 2000s present lower five-year SRs than that of the present study, although we might consider the effects of age and sex. The mean age in this study was 62.3 years, whereas the mean ages of the aforementioned studies were between 50 and 59 years. Also, the present study stratified SRs by age group. Although the five-year SR was 80% in the 60–69 group, 67.6% in the 70-79 group, and 40.5% in the group of 80 or older, and those 60 years of age or older comprised two-thirds of the population, aforementioned SRs for IPAH studies performed in the 2000s showed that they were greater than those recorded from studies in the 1980s and 1990s conducted in the US
11 and Korea.
12 This might be because various clinical trials assessing circulatory system medicines such as vasodilating agents and phosphodiesterase inhibitors have been actively conducted since the 2000s. Most previous studies showed that higher proportion of women was around 60–80% than that of men, and this was similar to the present study. Furthermore, we rarely found 10-year SRs for patients with IPAH in previous studies, so the 10-year SR for IPAH including by sex and by age group in this study could not be compared with that of previous research.
Recently, survival of selected PAH patients treated with targeted therapy in a Korean population was reported using the Korean Health Insurance Review and Assessment Service (HIRA).
13 In that previous study, the population of interest was derived from those who were reimbursed for targeted PAH therapies. Because of delays in the approval of sildenafil and tadalafil (with still no approval for tadalafil from the Korean Food and Drug Administration) and strict indications for reimbursement before 2014 (i.e., all the medications were reimbursed only among symptomatic patients with World Health Organization (WHO) functional class III or IV), the number of participants and data of this prior study vary slightly different from the present data. Also, the prior study included the patients with associated PAH, including connective tissue disease and congenital heart disease; on the contrary, we only included those with idiopathic PAH. Also, in this previous HIRA data investigation, the three- and five-year SRs were around 42% and around 35%, respectively, among 674 Korean IPAH patients treated with approved targeted therapies for PAH, including bosentan, beraprost, sildenafil, ambrisentan, macitentan, and iloprost from 2008 to 2016.
13 Moreover, SRs of IPAH with PAH-related drug therapy were relatively lower than ours because both the KNHIS and HIRA databases only report data on drugs, procedures, and surgery covered by the National Health Insurance. In addition, to be covered by the National Health Insurance, IPAH patients using bosentan, ambrisentan, macitentan, and iloprost must have PAH of be WHO functional class III or IV. Therefore, we may assume that the prior study of IPAH with PAH-related drug therapy included more relatively moderate or severe IPAH patients than did the present study. Hence, there was a difference in the three- to five-year SRs between these investigations. Given the expanded life expectancy thanks to novel treatment medications, we think that more effort should be taken for the continued surveillance with echocardiography in patients who suffer from unexplained dyspnea.
From the results of the adjusted HR calculation for IPAH, significantly higher HRs were apparent for older age
6101415 and male patients.
6814 Because mean age between different sex group showed significant differences, we analyzed HR of sex after age group adjusted. And finally, HR of male gender is significantly higher. Male gender is a well-known risk when compared to women in cardiovascular disease
16 and lower life expectancy compare to women in other diseases.
1718 In REVEAL 2.0 calculator, male age > 60 year is also a risk factor for PAH prognosis which is similar result to our study.
19
Meanwhile, the significantly lower adjusted HRs of essential hypertension for IPAH were shown. Because resting systolic blood pressure (BP) < 110 mmHg is associated with poor outcome in IPAH
20 baseline high blood pressure possibly linked to better outcome in our study population. And the significantly higher adjusted HRs for diabetes mellitus and myocardial infarction for IPAH were shown in this study, and adjusted HRs for essential hypertension, diabetes mellitus and coronary artery disease in the PHSANZ registry
8 were not statistically significant. In the present study, the adjusted HRs of the low socioeconomic group, atrial fibrillation patients, ischemic stroke patients, hemorrhagic stroke patients, and malignancy neoplasm patients were significantly higher than each counterpart. Unfortunately, no comparable previous studies could be found.
The three most common causes of death among patients with IPAH in the order of high to low distribution were diseases of the circulatory system, malignant neoplasms, and diseases of the respiratory system. These results showed similarity with those reported from the Giessen PAH registry, where the three most common causes of death were heart failure (33%), respiratory insufficiency (22%), and malignancy (9%).
5
The present study had several limitations. First, the National Health Insurance benefit records might have missed patients with IPAH who did not use medical services or who paid out of pocket for their medical expenses. Therefore, the SRs and death risk for IPAH in the present study might be under- or overestimated. Second, we did not consider the results of echocardiography, cardiac angiography, use of circulatory system medicines such as vasodilating agents or phosphodiesterase inhibitors, and/or severity risk such as REVEAL risk score when analyzing the HRs due to data limitations. Third, our data contained large number of pediatric patients and old age patients. Diagnosis of pediatrics or old age can be easily misdiagnosed when diagnosis is performed by echocardiography only. For example, transient pulmonary hypertension in children or heart failure with preserved ejection fraction in old age can mimic PAH. Because there is a trend of avoiding cardiac catheterization during diagnostic process in previous practice in Korea, number of IPAH patients can be overestimated.
21
In conclusion, the five-and 10-year SRs were 72% and 57%, respectively. The HRs for IPAH were significantly high in correlation with older age, male sex, low socioeconomic status, diabetes mellitus, myocardial infarction, atrial fibrillation, ischemic or hemorrhagic stroke, and malignant neoplasm. The most common cause of death in patients with IPAH was diseases of the circulatory system. Our reported patterns of SR and death risk for IPAH should be considered in future research designs and policies for cardiovascular healthcare services, with particular attention paid to gender. Furthermore, the results of the current study can provide new information on the contemporary prevalence of IPAH, and will be helpful for establishing healthcare policy regarding this rare intractable, but clinically important disease.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download