INTRODUCTION
Burnout is defined as “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed” by the 11th Revision of the International Classification of Disease.
1 It is well-known that burnout is rampant in stressful professions requesting long working hours and heavy workloads, which is common in medical professions.
2 The previous study reported that the burnout rate of physicians had reached global epidemic levels; 78% of physicians out of 8,774 in the American Physicians Survey in 2018
3 and 80% of 3,500 licensed British doctors in the British Medical Association 2019 Survey have experienced burnout.
4
Physician burnout is associated with suboptimal patient care and professional inefficiencies.
567 At an individual level, burnout increases stress, depression, and the risk of suicide among physicians. At an organizational level, burnout decreases quality of care and patient satisfaction but increases clinical errors and high turnover rates. These adverse outcomes lead to substantial economic loss and high costs associated with replacing, recruiting, and retraining doctors. Gabbay et al.
5 raised concerns about higher burnout among U.S. endocrinologists and the personal and organizational consequences from the burnout. A recent meta-analysis provided evidence that physician burnout may jeopardize patient care. This meta-analysis of 47 studies on 42,473 physicians found that burnout is associated with two-fold increased odds for unsafe care, unprofessional behaviors, and low patient satisfaction.
6 The authors of this study argued that reversal of this risk has to pursue as a fundamental healthcare policy goal across the globe.
6
Compared to large-scale surveys abroad to identify physician burnout status, studies on physician burnout are lacking in Korea. Although a previous study warned of a high rate (37.1%) of burnout in Korean medical school faculty members, it was only confined to the south-eastern parts of Korea (186 faculty members, 49% out of the total faculty members from the participating four universities).
7 To the best our knowledge, there has been no Korean study to report physician burnout statistics nationwide or reveal related factors and consequences of burnout.
It defines that ordinary professors’ roles in the university are teaching, research, and contribution to social value. In addition to these roles, faculty members at clinical departments in medical schools are mandatory to do the clinical practice. Faculty members of university-affiliated hospitals in Korea are more prone to being over-burdened in medical practice. A Korean survey of 456 medical college professors in 2004 showed that 49.8% of working hours were devoted to clinical practice compared to research activities (18.0%) and educational activities (15.6%).
8 Besides teaching medical students, faculty members of clinical departments should train residents, communicate with diverse healthcare personnel, and manage healthcare teams effectively. Although professors in basic medical science or humanities are free from clinical work, they still struggle to deal with the heavy workload in undergraduate and postgraduate education and ever-increasing research requirements. Therefore, we presume that faculty members in Korean medical schools are vulnerable to a higher degree of burnout.
In 2020, the upheaval of the coronavirus disease 2019 (COVID-19) pandemic drastically changed the medical school environment
910 and intensified faculty members’ burdens in patient care and the adaptations for new teaching platforms and technology.
1112 Moreover, from September 2020 to October 2020, unprecedented strikes of all residents and the allied school leave by medical students in Korea provoked by a new healthcare policy, which the government proposed, increased the workload and challenges of medical faculty members in Korea.
13
There have been no national statistics on the burnout of Korea’s medical school faculty members. This study is the first nationwide survey to explore the burnout rate and factors related to burnout. The authors of this study aimed to: 1) investigate the burnout levels perceived by medical school faculty members; 2) explore possible factors related to burnout, including demographic characteristics, working conditions, and source of stress; and 3) identify adverse effects of burnout.
Go to :

METHODS
Survey participants and data collection
There are various types of faculty members in Korean medical schools depending on the contract with an institution, including funding sources for salaries and employment stability. This study included tenure tract professors registered by the Ministry of Education, clinical professors hired by university-affiliated hospitals only, and professors hired by a university only.
This study was conducted by a grant from “Faculty Welfare Committee” at the Korea Association of Medical Colleges (KAMC). To promote active participation from all 40 medical colleges, KAMC sent an official letter of cooperation and a letter of information about the study to all 40 deans. As per approval by all deans, a survey link with a letter of information was sent to each university administration office by email. The responsible administrative staff in each university emailed their faculty members the survey information for voluntary participation. The authors of this study could not identify the exact number of distributed emails to the faculty members at each university. Furthermore, we could not trace who actually participated in the survey in accordance of our IRB protocol assuring an anonymous, voluntary participation. Consequently, the ratio of participants to the total study population could not be attained. An anonymous online survey was conducted using SurveyMonkey® (San Mateo, CA, USA) for two months, from October 25, 2020 to December 24, 2020. The participants started the questionnaire by signing up and completing the informed consent proving their volunteer participation.
Burnout measurement
Burnout was measured by 21 items out of the previous validated Korean version of Maslach Burnout Inventory-Human Service Survey (MBI-HSS)
14: seven items for each sub-dimension, emotional exhaustion, depersonalization, and sense of reduced personal accomplishment. Each item was scored on a 7-point Likert scale from zero (not experiencing at all) to six points (experience certain feelings, emotions, thoughts at least six times a week). We conducted the Rasch rating scale model analysis to test the validity of a modified version of 21 items (Linacre JM).
15 In the Rasch analysis, if all values of the Infit Mean Square are more than 0.5 and all Outfit Mean Square values are less than 2.0, all items are interpreted as good fits.
15 Our results showed the goodness-of-fit acceptable with the Infit Mean Square (0.8197–1.6534) and outfit Mean Square (0.6819–1.7904). We estimated two indices of reliability. Person reliability indicates the consistency with which the items calculate the latent score for persons (i.e., the frequency with which they experienced symptoms of burnout), and item reliability indicates the consistency with which persons calculate item and response option difficulties (i.e., the rank order and relative spacing between items). The acceptable levels of reliability of the two indices range from 0.70 to 0.95.
1617 The person reliability and item reliability of our data showed both ideal ranges of 0.97–0.99, 0.90–0.92, respectively. The Cronbach alpha showed high internal consistency of 0.963.
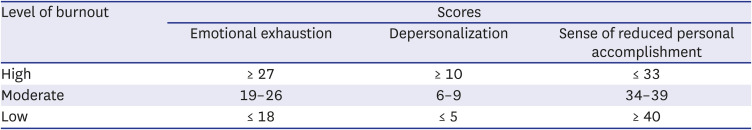
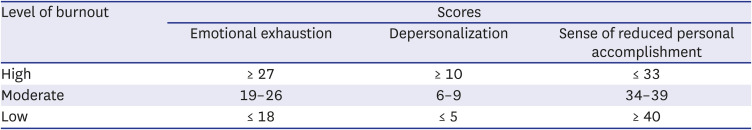
The MBI-HSS burnout scale is categorized into high, medium, and low-level burnout, and
Table 1 shows a cut score for high, moderate, and low levels of burnout.
18 In the emotional exhaustion and depersonalization dimensions, higher scores mean higher levels of burnout while lower scores mean a higher level of burnout in the reduced personal accomplishment dimension.
Table 1
Burnout level of each dimension of the Maslach Burnout Inventory-Human Service Survey
|
Level of burnout |
Scores |
|
Emotional exhaustion |
Depersonalization |
Sense of reduced personal accomplishment |
|
High |
≥ 27 |
≥ 10 |
≤ 33 |
|
Moderate |
19–26 |
6–9 |
34–39 |
|
Low |
≤ 18 |
≤ 5 |
≥ 40 |

Possible factors related to burnout
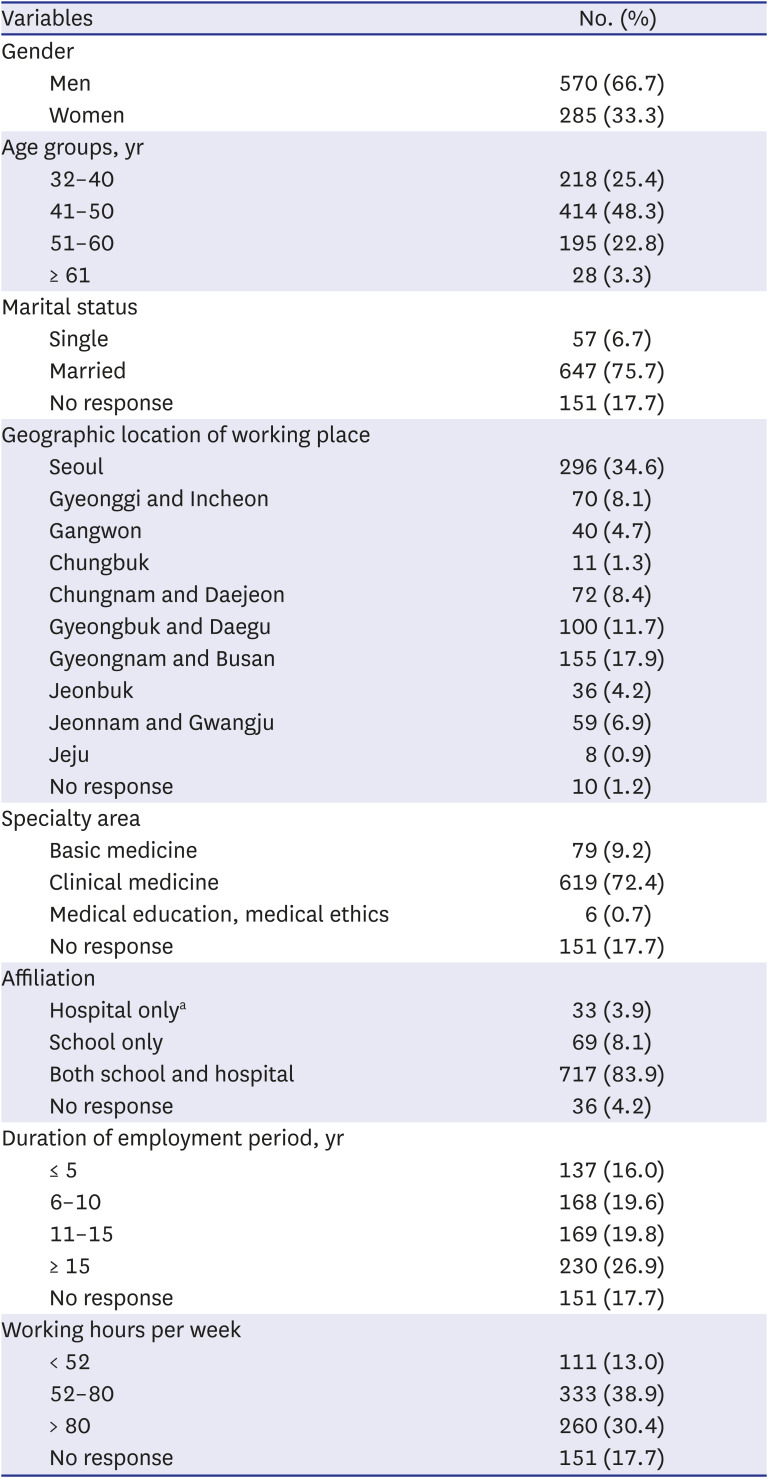
The questionnaire was composed of three parts to identify possible factors related to burnout. Part I consisted of items asking demographic characteristics, including age, gender, marital status, and working conditions. The items for working conditions included department (basic/clinical medicine), affiliation (hospital/school), position (assistant/associated/professor), employment period, and working hours per week. We did not include the items that might reveal the information of participants, such as university or hospital names, except the geographic location of the medical school.
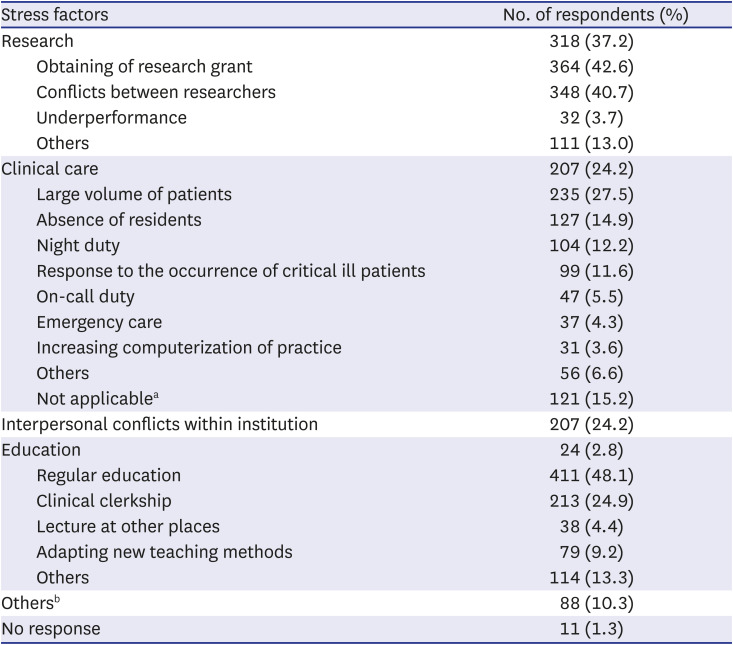
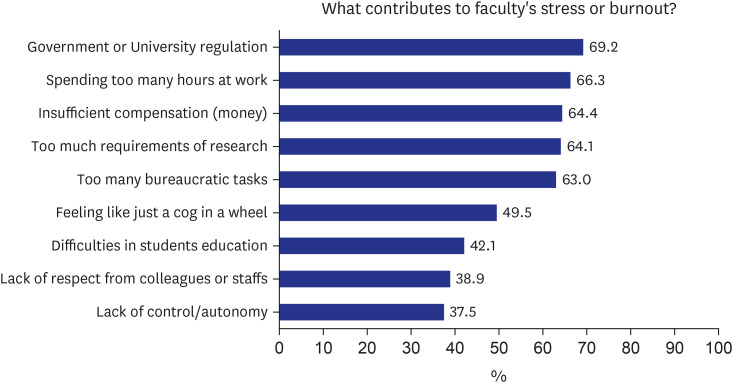
Part II asked the most significant stressor or burnout source from routine work. The questions of perceived levels of stress consisted of ten items: government or university regulation, working hours, insufficient compensation (money), requirements of research, bureaucratic tasks, feeling like just a cog in a wheel, difficulties in students education, lack of respect from colleagues or staffs, lack of control/autonomy and others (5-point Likert scale from 0: strongly disagree to 4: strongly agree). The participants were also asked to choose the one most stressful factor in research, clinical practice, and education, respectively. Options in research included obtaining research grants, conflicts between researchers, underperformance, and others. In clinical practice, the options included a large volume of patients, absence of residents, night duty, response to the occurrence of critically ill patients, on-call duty, emergency care, and increasing computerization of practice. Regular teaching, clinical clerkship, outside lecture, adapting new teaching methods, and others were included as options in education.
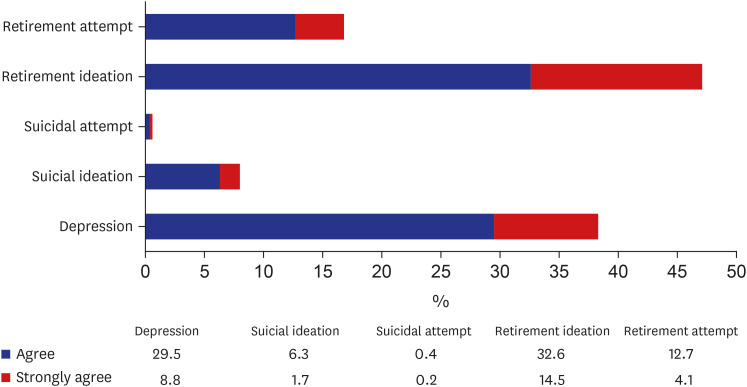
In Part III, the adverse effects of burnout included five items of depressive feelings, suicidal ideation, suicidal attempt, retirement intention, and retirement attempt (5-point Likert scale from 0: strongly disagree to 4: strongly agree).
Statistical analyses
Univariate analyses were done to obtain frequencies and percentages for the categorical variables and mean and standard deviation (SD) for continuous variables. Bivariate analyses examined the association between variables, using χ2 test, Students t-test, one-way ANOVA with posthoc analysis (Scheffe’s method), and Spearman's correlation. A reliability level of .05 was set up to be a statistical significance. The data were analyzed using IBM SPSS Statistics 25 (SPSS for Window version; SPSS, Inc., Chicago, IL, USA).
Ethics statement
The Institutional Bioethics Committee of Gyeongsang National University (GIRB-A20-Y-0014) permitted our study. This study conformed to the ethical guidelines of the World Medical Association Declaration of Helsinki. Informed consent was submitted by all subjects when they were enrolled.
Go to :

DISCUSSION
Although the burnout of medical doctors is problematic at the workplace and physician burnout reached the global crisis,
3181920 there has been no national study on burnout of medical doctors or medical faculty members in Korea. The present study shows Korean medical faculty members having a substantial level of burnout and alarms the increased awareness of physician burnout and reversal of this risk has to pursue as a fundamental healthcare policy.
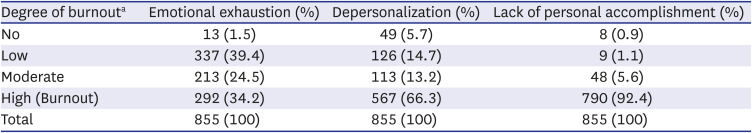
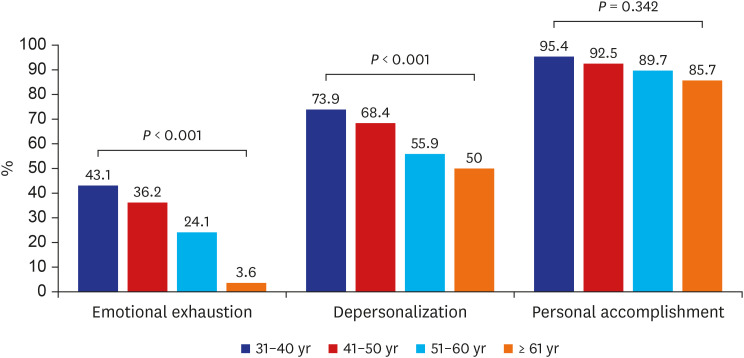
In this study, 34.2% of respondents showed emotional exhaustion, 66.3% with depersonalization, and 92.4% with a sense of reduced personal accomplishment. Up to 63.6% of medical faculty members responded that they have experienced burnout in two or more sub-dimensions, and 30.1% (257/855) of faculty members had high burnout in all three sub-dimensions. This degree of burnout in all three sub-dimensions is substantially higher than 10% of points in the 2019 U.S. Medical School Professors’ Burnout Survey.
20 Particularly, the degree of reduced personal accomplishment burnout was nine times higher than American medical school professors.
20 Compared to 11.8% for emotional exhaustion, 25.3% for depersonalization, and 14.5% for reduced personal accomplishment among professors at three universities in Busan and Gyeongnam area in 2014.
7 This study show a relatively higher degree in all three sub-dimensions of burnout. This increased frequency in burnout in our study may be interpreted partly by the difference of the participants distrubution of the current study, including sampling from all over the country. Alternatively, it may be assumed that the prevalence of burnout in medical school teachers has actually increased for the past several years. If it is true, it should be seriously taken into consideration. Therefore, it needs further investigation to identify what working conditions and school environments affected burnout of medical school faculty members in 2020 compared to that of 2014.
7
The present study found that young women faculty members who work in the clinical department were most vulnerable to burnout. In the previous analysis of the U.S., 35% of women professors and 26% of men professors experienced burnout,
20 and women professors had higher emotional exhaustion and depersonalization burnout than men professors. It may be explained that high burnout among women physicians has to do with dual roles of child care and house chores at the same time,
20 often being victims of bias and discrimination such as disparaging or disrespectful treatment or comments, lack of career promotion, and insufficient rewards and reimbursement.
2122 Balancing between professional work as a medical faculty member and personal work at home seems to increase the degree of burnout. Eliminating biases and gender discrimination which are a substantial source of stress for women faculty members can reduce burnout, especially emotional exhaustion.
21
This study found that the highest burnout in all three sub-dimensions of emotional exhaustion, depersonalization, and reduced personal accomplishment occurred in the 31–40 years old age group. It is explainable that this age group feels significant pressure related to clinical care, research for promotion, and education all at once as newly being appointed as a medical faculty member. In the 2019 burnout survey of doctors in the U.S., which divided age groups into millennials (ages 25–39), generation X (ages 40–54), and baby boomers (ages 55–73), the burnout level of generation X was the highest at 48%, followed by babyboomers at 39%, and millennials at 38%.
23 It explained that 40–54 years old is a critical period paying tuition and balancing family and work, thus increasing the degree of burnout in the U.S.
23
Burnout level of faculty members at hospitals and schools was higher than faculty members at only schools or hospitals, similar to that of the U.S. (11%).
22 The research was the most stressful factor for burnout, and many Korean medical faculty members (37%), were stressed out with research, which is similar to the U.S. Research.
20 This is a main exasperating task not only for medical faculties but also for other professors at universities for performance and promotion. The second contributing factor to stress or burnout was intra-organizational conflict, which is higher than clinical care or education.
In our study, Korean medical faculty members indicated “excessive government or institutional regulation” as the most contributing factor for stress and burnout at 69.2%. They responded that “excessive working hours,” “requirement of research results,” and “relatively low wage level” as the other stress factors at around 50%. The big strikes of residents and allied leave of students under upheaval of COVID-19 pandemic might affect the high burnout of Korean medical school faculty members in 2020.
12 In the U.S. study, American doctors indicated the most contributing factor for burnout is “too much bureaucratic work” at 58%, followed by “excessive working hours” (37%) and “lack of respect from administrators/employers, colleagues, or staff (37%).”
23
Most professors appeal to the difficulties of caring for too many patients and on-call or critically ill cases.
18 However, excessive working hours and demand for research are the same stressors for U.S. physicians and Korean medical faculty members. In our study, the average working hours of faculty members cannot be calculated, but working 52–80 hours per week is comparatively more prolonged than that of U.S. physicians, suggesting that the more time there is to see patients results in more burnout. The U.S. physicians complain that there is not enough time to change personal protective equipment due to excessive working hours with too many patients.
23 In the U.S., 44.7% of physicians care for cancer patients, and 33.8% of these physiciansare professors, experience burnout, and report their working hours as 58.6 hours for university hospitals and 62.9 hours for practitioners.
24
In our study, Korean faculties similarly chose drinking alcohol (27.8%) and eating food (23.9%) to cope with stress and burnout. Among the eight ways to cope with stress and burnout, exercise was the most common coping way (51.9%), slightly higher than the 48% of U.S. physicians.
25 Next, the U.S. physicians chose drinking alcohol (26%) and eating junk food (35%).
25
In our study, 47.5% of faculty members responded retirement ideation and retirement attempt (16.8%), which is significantly related to burnout. In the U.S. study, physicians did nothing (35%), reducing working hours (28%) and changing workplace (21%) to alleviate burnout.
25 Study results worldwide suggest that healthcare professionals, especially resident doctors and faculty members, are prone to developing mental health problems such as depression and anxiety.
26 In 2020, doctors in the U.S. reported that 69% of physicians felt depressed, and 20% were practically depressed, which is related to burnout.
25 Our results show that 30.1% of faculty members experienced burnout in all three dimensions, and 38.0% felt depressed. The 13.0% of professors responded suicidal ideation and 1.0% practically attempted suicide in the U.S. study,
23 whereas 8% of Korean faculty members responded suicidal ideation and 0.8% of suicidal attempts, which seems similar in adverse situations.
There are several limitations in this study. First, the number of participants in the survey may not represent all the medical faculty members of 40 Korean medical schools. Our results may not extend generalizability to those who did not participate in the survey since our data cannot free from selection bias or active participant bias. Since we could not find any credible source to confirm the exact number of faculty members in 40 medical schools in Korea in the survey year (2020), we could not tell what percentage of our respondents stands from the real target population. The best statistics we identified was 10,103 medical school faculty members by the latest statistics from the 2014 White Paper on Current Medical Education in Korea by the Research Institute for Healthcare Policy
27 If we use this number, our participants (n = 996) stands for 9.8% of faculty members of 2014. Secondly, we could not calculate the respondent rate out of the total distriubuted survey information because we did not collect the baseline data which tell us how many emails was distributed to faculty members by each university. However, we have found great value in this research as it is the first nationwide survey revealing the burnout status of medical school faculty members in Korea. Further studies are necessary to examine what factors affect burnout and how the medical school faculties manage burnout. In addition, we would like to suggest periodical investigation to identify the degree of burnout of medical school professors and developing a strategic policy to minimize burnout and depression and improve their quality of life.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download