Abstract
Background
The aim of this study was to investigate the relationship between pain catastrophizing, acceptance, and quality of life in relation to chronic low back pain in Jakarta, the capital city of Indonesia. We also analyze the effect of personality in catastrophizing and acceptance.
Methods
A total of 52 chronic low back pain patients were enrolled as participants from 2 hospitals in Jakarta (43 females, 9 males, mean age 54.38 years). Participants completed a set of self-reported questionnaires: the NEO Five Factor Inventory (NEO-FFI), Chronic Pain Acceptance Questionnaire-Revised (CPAQ-R), Pain Catastrophizing Scale (PCS), and Pain Discomfort Module (PDM).
Results
This study showed that acceptance increased the patient's quality of life by giving physical relief from pain. In contrast, pain catastrophizing decreased the quality of life, and increased the patients' tendency to get frustrated, irritated, and anxious about the pain. From a personality perspective, the trait neuroticism may lead to a higher level of pain catastrophizing.
Go to : 
Chronic pain is defined as pain or discomfort that persists continually or episodically for more than 3 months [1]. Low back pain (LBP) refers to pain that occurs in the lower portion of back. This pain can occur due to accident, heavy lifting, or changes in the structure of the spine related to aging. Despite the many causes, low back pain can be categorized as being either organic or mechanical. Organic pain can be caused by disease, such as spinal cancer, tumors, or aortic aneurisms. Mechanical low back pain means the source of the pain is in the spine and/or its supporting structure, it may be in the spinal joints, discs, vertebrae, or soft tissues [2]. The low back pain discussed in this study is mechanical low back pain. Chronic low back pain (CLBP) is pain in the lower back that occurs for more than 3 months, even though the causes have been treated [2].
A hospital-based survey conducted in 13 big cities in Indonesia revealed that low back pain is the most common condition of those with chronic pain (28.6%) [3]. The subjects were predominantly forty to sixty years old (57.9%), followed by less than 40 years old (24.85%) and more than 60 years old (17.26%).
Chronic pain, in this case low back pain, is complex because it is not only disturbing physically, but also has psychological, social, and economic impact because of its prolonged nature. Most chronic pain patients experience varying physical difficulties, ranging from difficulties with walking, doing household activities, and some even experiencing difficulty in performing simple activities such as sitting or standing [456]. In addition, chronic pain also affects social interaction, as it limits the activity and social contact of the patients. The complexities caused by chronic pain ultimately lead to the patients' lower quality of life [7].
According to World Health Organization (WHO), quality of life is “the individuals' perception of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns” [1]. However, for chronic pain patients, quality of life can be understood specifically with some particular and relevant details. These are related to the nature of the pain which is chronic and uncontrollable. The aspects of the quality of life in chronic pain are pain relief; anger and frustration; vulnerability, fear, and worry, as well as uncertainty [1].
Chronic pain not only affects physical but also psychological functioning. A number of studies suggest that the psychological aspects which play an important part in chronic pain are acceptance and catastrophizing [8910111213]. Acceptance is shifting focus from something that cannot be controlled (pain and the negative emotion) to more controllable ones (changing how the body moves in doing daily activities) [10]. McCracken and Eccleston [14] stated that rather than trying to control uncontrollable experiences like pain, people who responded with acceptance reported better results, with less pain intensity and fewer physical disabilities, less depression and pain-related anxiety, and also a better work status. Acceptance consists of two factors which are (1) activity engagement, pursuit of life activities regardless of pain, and (2) pain willingness, the willingness to experience pain without trying to avoid or reduce it [15].
On the other hand, individuals who repeatedly attempt to control uncontrollable pain show lower quality of life and higher catastrophizing [1116]. Catastrophizing refers to an exaggerated negative interpretation to an expected or actual experience of pain, and is characterized by magnification of the potential negative aspects of pain, a feeling of helplessness in coping with pain, and an inability to disengage from thoughts about pain in anticipating, during, or after experiencing pain [17]. Catastrophizing is an important factor in determining how cognition, belief, coping strategy, and functioning relate to the pain experience [12], and correlates with pain intensity, disability, lowered pain threshold, a worse prognosis, and poorer responses to pain intervention [18192021]. Catastrophizing consists of 3 factors, which are (1) rumination, which refers to ruminative thoughts, worry, and an inability to inhibit pain-related thoughts; rumination reflects an inability to suppress or divert attention away from pain-related thoughts; (2) magnification, refers to a tendency to exaggerate the unpleasantness of pain and expectancies for negative outcomes; and (3) helplessness, reflecting the inability to deal with painful situations [22].
Study shows that to improve the quality of life, it is not enough to just focus on increasing acceptance, but also by reducing catastrophizing [23]. Both acceptance and catastrophizing are also influenced by the patient's personality [112324]. Based on researches conducted using factor analysis, the various basic personality traits can be classified into five main factors which are found consistently throughout the world. These five factors are known as five factor model (FFM) which categorized human personality into five dimension: neuroticism, extraversion, openness, agreeableness, and conscientiousness [25].
This study aims to investigate the relations among catastrophizing, acceptance, and quality of life in patients with chronic low back pain. In general, the treatment of chronic pain in the hospital is more focused on the physical aspect, using pharmacological therapy [26]. Therefore, this study is expected to encourage the development of a more comprehensive treatment for chronic pain, which involves various aspects including the psychological aspect, to complement therapy with drugs, especially in Indonesia. In addition, this study is expected to enrich the understanding about chronic pain in Indonesia, considering there have not been many studies on this matter in the country.
Go to : 
The study was conducted with approval from the Ethics Committee from Unika Atma Jaya; the Institutional Review Board from Atma Jaya Hospital, Jakarta; and the Institutional Review Board from Royal Taruma Hospital, Jakarta. All participants provided written informed consent which was also previously approved by the ethics committee.
Participants were recruited from 2 hospitals in Jakarta with inclusion criteria: (1) having chronic mechanical low back pain diagnosed by a neurologist; (2) having suffered chronic low back pain for more than 3 months [2]; (3) having their pain was caused by mechanical disturbance in the musculoskeletal system; (4) being from 40 to 60 years of age; (5) a minimum educational level of elementary school (being able to read and write); (6) not being blind, deaf, or mute, which could hinder the data collection process; (7) live in Jakarta. Individuals who claimed to have low back pain but were not diagnosed by a specialist were excluded, as well as patients who suffered chronic low back pain due to cancer, being post-operation, or experiencing pregnancy. A total of 52 participants referred by neurologists were included in this study (43 women and 9 men, mean age 54.38 years old).
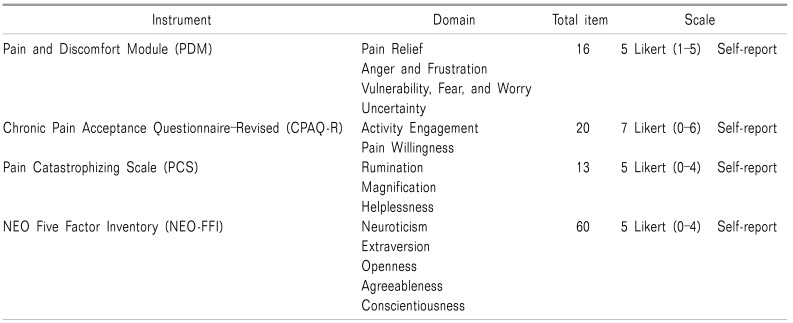
Several instruments used for collecting data in this study are the Pain and Discomfort Module (PDM), Chronic Pain Acceptance Questionnaire-Revised (CPAQ-R), Pain Catastrophizing Scale (PCS), and NEO Five Factor Model (NEO-FFI), which were translated into Bahasa. The PDM is a self-report questionnaire used to assess quality of life, specifically in chronic pain patients. This instrument was developed by Mason, et al. [27] with inter-item correlation for each domain ranging from −0.05 to −0.77 and Cronbach's alpha = 0.78.
The PDM consists of 16 items in Likert scale ranging from 1 to 5, which represent 4 domains. In interpreting the score for each domain, three out of four domains have to interpret negatively, which are anger and frustration; vulnerability, fear and worry; and uncertainty (Table 1). The higher the scores obtained in these three domains, the lower the quality of life. For the pain relief aspect, the score is interpreted positively. The higher the pain relief score is, the higher the quality of life is [27].
The CPAQ-R is a self-report questionnaire developed by McCracken et al. [15] to assess acceptance of pain. This instrument consists of 20 items in the Likert scale from 0 to 6 (Table 1). A higher score indicates higher acceptance in patients. The CPAQ-R Indonesian version has been demonstrated to have good internal consistency reliability (Cronbach's alpha = 0.79, inter-item correlation from 0.25 to 0.58). The PCS was developed by Sullivan et al. [22] to assess pain catastrophizing. The PCS consists of 13 items in the Likert scale from 0 to 4 (Table 1). A higher score indicates higher catastrophizing. Internal consistency for the Indonesian version is 0.93 and inter-item correlation ranges from 0.50 to 0.80.
The NEO-FFI was developed by Costa and McCrae [28] to assess personality traits in term of the five factor model. The NEO-FFI consists of 60 items with the Likert scale on 0–4. These items representing 5 domains: neuroticism, extraversion, openness, agreeableness, and conscientiousness (Table 1).
The total score for each of the domains is calculated by summing the item scores on each domain. A domain with higher score indicates that those domain characteristics are more dominant in the particular person. The validated Indonesian version was used and the measurements in this study were shown good internal consistencies in each domains (Cronbach's alphas: neuroticism = 0.78, extraversion = 0.68, openness = 0.42, agreeableness = 0.67, and conscientiousness = 0.73).
All instruments in this study are Likert scale, therefore the statistical non-parametric Spearman-Rho was used to assess correlation among variables. Furthermore, regression analysis was added if there were any variables that significantly correlated with each other. This regression analysis was performed using multiple linear regression. All analyses were conducted using IBM SPSS for Windows Version 22.
Go to : 
The study participants were 52 patients with chronic low back pain, 43 women (82.7%) and 9 men (17.3%), with mean age 54.38 years old. A majority of participants were married (82.7%) and worked as housewives (59.6%). Pain was measured with the Numerical Pain Rating Scale (NPRS), the result ranging from 1 (low pain intensity) to 8 (high pain intensity) with a mean NPRS result of 4.7 (SD = 1.8). The duration of the pain reported by participants ranged from 4 months to 20 years but for the majority it was 5 months–5 years (48.1%).
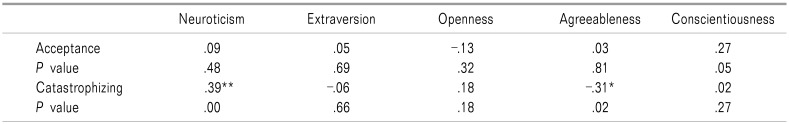
There were two personality dimensions, neuroticism and agreeableness, that significantly correlated with catastrophizing (Table 2). Neuroticism was positively correlated with catastrophizing. In other words, the higher the neuroticism trait in a person, the higher the tendency for the catastrophizing level to increase (rs = 0.398, P < 0.01). The more worried the people are, the more likely it is for them to interpret their pain negatively, and vice versa. In contrast, agreeableness was negatively correlated with catastrophizing (rs = −0.314, P < 0.05). An agreeable person tends not to overly think about their pain, hence decreasing their catastrophizing.
Multiple regression analysis between neuroticism and agreeableness was performed to investigate whether the two personality dimensions can predict catastrophizing. From Table 3, we can conclude that neuroticism is a significant predictor of catastrophizing which contributes 13.7% of the variances in chronic low back pain patients.
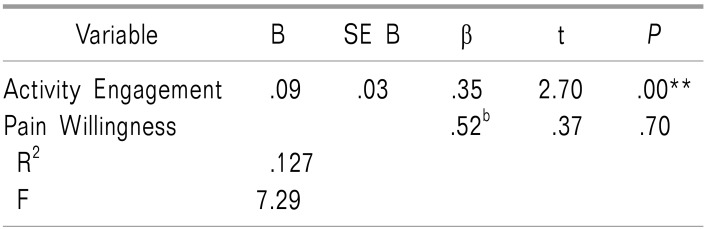
Acceptance has a significant positive correlation with pain relief, one of the many aspects in quality of life related to chronic pain (rs = 0.335, P < 0.05), and has no correlation with the other three aspects (Table 4). Acceptance consists of 2 factors, which are pain willingness and activity engagement. Based on Table 5, activity engagement is correlated significantly with pain relief (rs = 0.359, P < 0.05) and predicted a 12.7% proportion of the variances.
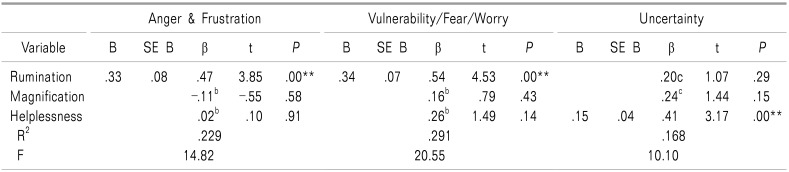
On the other side, catastrophizing was positively correlated with three out of the four aspects in quality of life related to chronic pain; anger & frustration (rs = 0.436, P < 0.05), vulnerability/fear/worry (rs = 0.564, P < 0.05), and uncertainty (rs = 0.410, P < 0.05) (Table 4). Specifically, one factor in catastrophizing, rumination, was responsible for anger and frustration (22.9%) as well as anxiety and fear experienced by the patients (29.1%). The other factor in catastrophizing which affected quality of life was helplessness. It was responsible for the feeling of uncertainty experiences by the patients (16.8%) (Table 6).
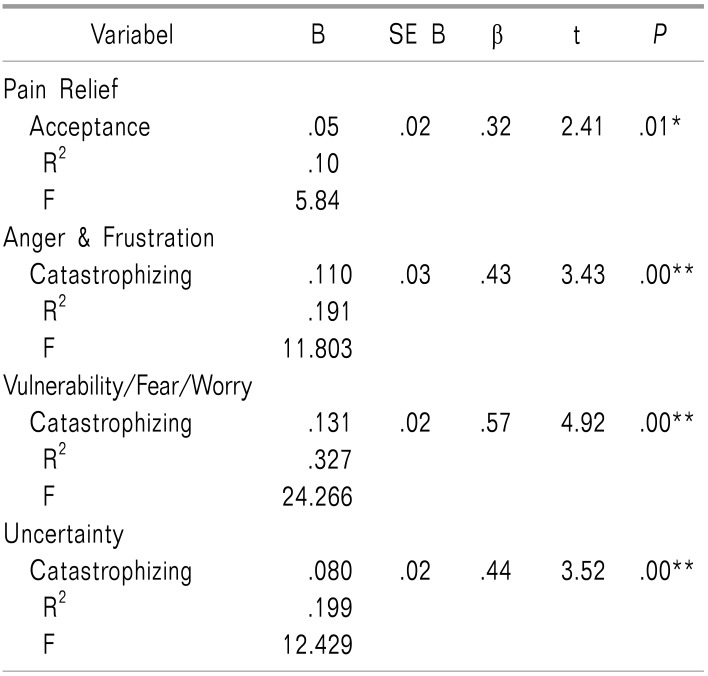
Multiple regression analysis was performed with acceptance and catastrophizing as predictors, and quality of life as the dependent variable. As shown in Table 6, both acceptance and catastrophizing are significant predictors of quality of life in chronic low back pain patients. Acceptance predicts a 10.5% proportion of pain relief, and catastrophizing is a predictor of anger & frustration (19.1%), vulnerability/fear/worry (32.7%), and uncertainty (19.9%) (Table 7).
Go to : 
The results showed that quality of life was determined by acceptance and catastrophizing. Acceptance has a positive impact on quality of life, whereas catastrophizing has a negative impact. Thus, to improve quality of life, the catastrophizing level should be lowered and acceptance should be raised. However, independently speaking, quality of life with chronic pain in this study was more affected by catastrophizing than acceptance.
Acceptance can improve the quality of life by affecting one of its aspects, which is pain relief. Chronic low back pain patients who are able to accept their condition tend to feel more relief, physically, as if the pain is reduced. This finding is in line with previous studies which stated that greater acceptance is associated with better emotional, physical, and social function [91014151629]. In this study, the factor in acceptance that can predict pain relief is activity engagement. This means that the patients who are still doing daily activities tend to have better quality of life in term of physical relief. A possible explanation is that patients who remain active are consistently, yet unintentionally, training their muscles, which improves muscle strength and mobility, thus reducing the pain, as in physiotherapy [30].
On the contrary, catastrophizing decreased the quality of life and affected three of its aspects, which are anger and frustration, vulnerability/fear/worry, and uncertainty. Patients who perceive their pain negatively tend to be more frustrated, angry, anxious, afraid, and tend to worry about the pain. They also have difficulties in planning their future due to the uncertainty of whether the pain will get better or worse. Moreover, constantly thinking in a negative way about the pain and the helplessness can cause the patients to feel frustration, anger, anxiety, and fear about the pain. These things particularly affect the patients' psychological and social function, as well as their autonomy. These align with Severeijns et al. [31], who mentioned that catastrophizing is significantly associated with the psychological and social aspects of quality of life in chronic pain patients. This study also supports several other studies which reported that catastrophizing has negative impacts for patients with chronic pain [121719202132].
Regression analysis among the factors of catastrophizing showed that rumination and helplessness are factors that can decrease patients' quality of life. Patients who ruminate and are constantly thinking about their pain feel more anxious, afraid, frustrated, and angry, which in the end, lowers their quality of life. Feeling helpless due to chronic low back pain causing the patients to be more uncertain about their future. This leads to difficulties in planning their future, impacts the social function and autonomy, and therefore lower their quality of life. This finding is consistent with Severeijns et al. [31] which stated that catastrophizing has been greatly associated with the psychological and social aspects of quality of life in chronic pain.
We also assessed the effect of personality on catastrophizing and acceptance. According to the result in this study, personality, the trait neuroticism particularly, has a significant association with catastrophizing and actually contributes to it. Neuroticism is a tendency to feel negative emotion and have a low tolerance to pressure [33]. Its sensitivity to negative emotion relates to magnifying the negatives, as it does in catastrophizing. This result suggested that neuroticism has a substantial role in a person's mental condition, contributing to higher catastrophizing and lowering their quality of life. The more the patients feel worried, anxious, and vulnerable to negative emotions, the higher their tendency to build negative feeling towards their chronic pain. This finding is consistent with previous studies which showed that neuroticism is a personality dimension with a negative contribution in health issues [3435], and therefore needs to be controlled.
The majority of the participants in this study are female (82.7%) who work as housewives (59.6%). Consistently, other studies reported that women have a higher prevalence of chronic low back pain [3637]. Middle-aged women have a greater risk in developing musculoskeletal disturbance due to biological issues [3839]. Besides, activities performed by housewives such as heavy lifting, bending, standing or sitting for long period of time, and repetitive movement may also contribute to musculoskeletal issues such as low back pain [40].
This study has several limitations. First, due to the small number of participants recruited, the results cannot be generalized to another population. Second, demographic data in this study is not proportional so we cannot analyze its effect on research variables. Also, we did not control participants' previous treatments; some patients only used pharmacological treatment, while others used pharmacological and physiotherapy. It is recommended that future research use more participants, with diverse and proportionate demographic data. Besides, controlling for previous treatment and considering the pain duration, pain threshold, and underlying psychiatric conditions such as depression and mood changes disorder in the study may help to get a more comprehensive result.
In conclusion, quality of life in chronic low back pain patients in Jakarta was more affected by catastrophizing, resulting in a lower quality of life, which needs to be improved. It is not enough to improve quality of life only by dealing with physical pain; we must also consider patients' psychological condition, including catastrophizing. Having said so, one suggestion that can be recommended for patients with chronic low back pain is to join a pain management program with a multidisciplinary basis. In Indonesia, one of the multidisciplinary pain management programs is Jakarta's Program Tatalaksana Nyeri Kronis Multidisiplin (POTENSI) [41]. POTENSI has shown to improve the quality of life in chronic low back pain patients in Jakarta [41].
Go to : 
ACKNOWLEDGEMENTS
The authors want to thank Dr. Jimmy Barus, Dr. Linda Suryakusuma, Dr. Andre, Dr. Octavianus Darmawan, and Dr. Jane from Atma Jaya Hospital, also Dr. Imelda and Dr. Handoyo from Royal Taruma Hospital for contributing to data collection.
Go to : 
References
1. Mason VL, Mathias B, Skevington SM. Accepting low back pain: is it related to a good quality of life? Clin J Pain. 2008; 24:22–29. PMID: 18180632.

2. National Institute of Neurological Disorders and Stroke (NINDS). Chronic pain information page [Internet]. Rockville (MD): NINDS;2016. cited 2017 Sep 20. Available at https://www.ninds.nih.gov/Disorders/All-Disorders/Chronic-Pain-Information-Page.
3. Purwata TE, Sadeli HA, Yudiyanta Y, Anwar Y, Amir D, Asnawi C, et al. Characteristics of neuropathic pain in Indonesia: a hospital based national clinical survey. Neurol Asia. 2015; 20:389–394.
4. Amris K, Wæhrens EE, Jespersen A, Bliddal H, Danneskiold-Samsøe B. Observation-based assessment of functional ability in patients with chronic widespread pain: a cross-sectional study. Pain. 2011; 152:2470–2476. PMID: 21715094.

5. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006; 10:287–333. PMID: 16095934.

6. McBeth J, Nicholl BI, Cordingley L, Davies KA, Macfarlane GJ. Chronic widespread pain predicts physical inactivity: results from the prospective EPIFUND study. Eur J Pain. 2010; 14:972–979. PMID: 20400346.

7. Bentsen SB, Hanestad BR, Rustøen T, Wahl AK. Quality of life in chronic low back pain patients treated with instrumented fusion. J Clin Nurs. 2008; 17:2061–2069. PMID: 18705783.

8. Doran NJ. Experiencing wellness within illness: exploring a mindfulness-based approach to chronic back pain. Qual Health Res. 2014; 24:749–760. PMID: 24728110.
9. Evers AW, Kraaimaat FW, van Lankveld W, Jongen PJ, Jacobs JW, Bijlsma JW. Beyond unfavorable thinking: the illness cognition questionnaire for chronic diseases. J Consult Clin Psychol. 2001; 69:1026–1036. PMID: 11777106.

10. McCracken LM, Eccleston C. A prospective study of acceptance of pain and patient functioning with chronic pain. Pain. 2005; 118:164–169. PMID: 16203093.

11. Poppe C, Crombez G, Devulder J, Hanoulle I, Vogelaers D, Petrovic M. Personality traits in chronic pain patients are associated with low acceptance and catastrophizing about pain. Acta Clin Belg. 2011; 66:209–215. PMID: 21837930.
12. Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009; 9:745–758. PMID: 19402782.

13. Vowles KE, McCracken LM, Eccleston C. Processes of change in treatment for chronic pain: the contributions of pain, acceptance, and catastrophizing. Eur J Pain. 2007; 11:779–787. PMID: 17303452.

14. McCracken LM, Eccleston C. Coping or acceptance: what to do about chronic pain? Pain. 2003; 105:197–204. PMID: 14499436.

15. McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004; 107:159–166. PMID: 14715402.

16. Viane I, Crombez G, Eccleston C, Poppe C, Devulder J, Van Houdenhove B, et al. Acceptance of pain is an independent predictor of mental well-being in patients with chronic pain: empirical evidence and reappraisal. Pain. 2003; 106:65–72. PMID: 14581112.

17. Sturgeon JA, Zautra AJ. Psychological resilience, pain catastrophizing, and positive emotions: perspectives on comprehensive modeling of individual pain adaptation. Curr Pain Headache Rep. 2013; 17:317. PMID: 23338769.

18. Cecchi F, Molino-Lova R, Paperini A, Boni R, Castagnoli C, Gentile J, et al. Predictors of short- and long-term outcome in patients with chronic non-specific neck pain undergoing an exercise-based rehabilitation program: a prospective cohort study with 1-year follow-up. Intern Emerg Med. 2011; 6:413–421. PMID: 21153893.

19. Rosenberg JC, Schultz DM, Duarte LE, Rosen SM, Raza A. Increased pain catastrophizing associated with lower pain relief during spinal cord stimulation: results from a large post-market study. Neuromodulation. 2015; 18:277–284. PMID: 25817755.

20. Smith AD, Jull GA, Schneider GM, Frizzell B, Hooper RA, Sterling MM. Low pain catastrophization and disability predict successful outcome to radiofrequency neurotomy in individuals with chronic whiplash. Pain Pract. 2016; 16:311–319. PMID: 25594839.

21. Walton DM, Macdermid JC, Giorgianni AA, Mascarenhas JC, West SC, Zammit CA. Risk factors for persistent problems following acute whiplash injury: update of a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2013; 43:31–43. PMID: 23322093.

22. Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995; 7:524–532.

23. Elander J, Robinson G, Mitchell K, Morris J. An assessment of the relative influence of pain coping, negative thoughts about pain, and pain acceptance on health-related quality of life among people with hemophilia. Pain. 2009; 145:169–175. PMID: 19573989.

24. Poppe C, Crombez G, Hanoulle I, Vogelaers D, Petrovic M. Improving quality of life in patients with chronic kidney disease: influence of acceptance and personality. Nephrol Dial Transplant. 2013; 28:116–121. PMID: 22822093.

25. McCrae RR, Costa PT. Personality in adulthood: a five-factor theory perspective. 2nd ed. New York: Guilford Press;2003.
26. American Chronic Pain Association. Resource guide to chronic pain management [Internet]. Rocklin (CA): American Chronic Pain Association, inc.;2018. cited 2018 Dec 31. Available at https://www.theacpa.org/wp-content/uploads/2018/05/ACPA_Resource_Guide_2018-update.pdf.
27. Mason VL, Skevington SM, Osborn M. The quality of life of people in chronic pain: developing a pain and discomfort module for use with the WHOQOL. Psychol Health. 2008; 23:135–154. PMID: 25160047.

28. Costa PT, McCraes RR. Revised NEO personality inventory (NEO PI-R) and NEP five-factor inventory (NEO-FFI): professional manual. Odessa: Psychological Assessment Resources;1992.
29. McCracken LM, Eccleston C, Bell L. Clinical assessment of behavioral coping responses: preliminary results from a brief inventory. Eur J Pain. 2005; 9:69–78. PMID: 15629877.

30. Arovah NI. Dasar-dasar fisioterapipada cedera olahraga. Yogyakarta: FIK UNY;2010.
31. Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain. 2001; 17:165–172. PMID: 11444718.

32. Banozic A, Miljkovic A, Bras M, Puljak L, Kolcic I, Hayward C, et al. Neuroticism and pain catastrophizing aggravate response to pain in healthy adults: an experimental study. Korean J Pain. 2018; 31:16–26. PMID: 29372022.

33. Burger JM. Personality. Belmont: Thomson Wadsworth;2004.
34. Hajek A, Bock JO, König HH. The role of personality in health care use: results of a population-based longitudinal study in Germany. PLoS One. 2017; 12:e0181716. PMID: 28746388.

35. Widiger TA, Oltmanns JR. Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiatry. 2017; 16:144–145. PMID: 28498583.

36. Meucci RD, Fassa AG, Faria NM. Prevalence of chronic low back pain: systematic review. Rev Saude Publica. 2015; 49:73.

37. Shmagel A, Foley R, Ibrahim H. Epidemiology of chronic low back pain in US adults: data from the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Care Res (Hoboken). 2016; 68:1688–1694. PMID: 26991822.

38. Barbe MF, Gallagher S, Massicotte VS, Tytell M, Popoff SN, Barr-Gillespie AE. The interaction of force and repetition on musculoskeletal and neural tissue responses and sensorimotor behavior in a rat model of work-related musculoskeletal disorders. BMC Musculoskelet Disord. 2013; 14:303. PMID: 24156755.

39. Wang YXJ. Postmenopausal Chinese women show accelerated lumbar disc degeneration compared with Chinese men. J Orthop Translat. 2015; 3:205–211. PMID: 30035059.

40. Habib RR, El Zein K, Hojeij S. Hard work at home: musculoskeletal pain among female homemakers. Ergonomics. 2012; 55:201–211. PMID: 21846278.

Go to : 




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download