INTRODUCTION
An epidural steroid injection (ESI) is a commonly administered procedure in pain clinics. The indications include herniated intervertebral disc (HIVD), radiculopathic pain syndrome, spondylolisthesis, herpes zoster, postherpetic neuralgia, and others. ESI using the transforaminal (TF) or interlaminar (IL) approach is a commonly performed procedure [
1]. A larger amount of drug is injected in the IL approach than in the TF approach. Therefore, subdural injection or accidental epidural puncture that leads to a total spinal anesthesia may occur more easily in the IL approach than in the TF approach. The success or failure of the appropriate ESI under C-arm guidance is determined by contrast imaging. Consequently, the interpretation of contrast imaging is very important.
In a previous study, Huang et al. [
2] reported that unintentional lumbar facet joint injection during interlaminar ESI was occurring. The incidence was low, but repositioning of the needle tip into the epidural space was needed [
3]. So far, there has not been much research on the characteristics of patients who have undergone unintentional lumbar facet joint injection. The purpose of this study was to illustrate the contrast patterns of an unintentional lumbar facet joint injection during an interlaminar ESI and to analyze the characteristics of patients who underwent this injection.
Go to :

RESULTS
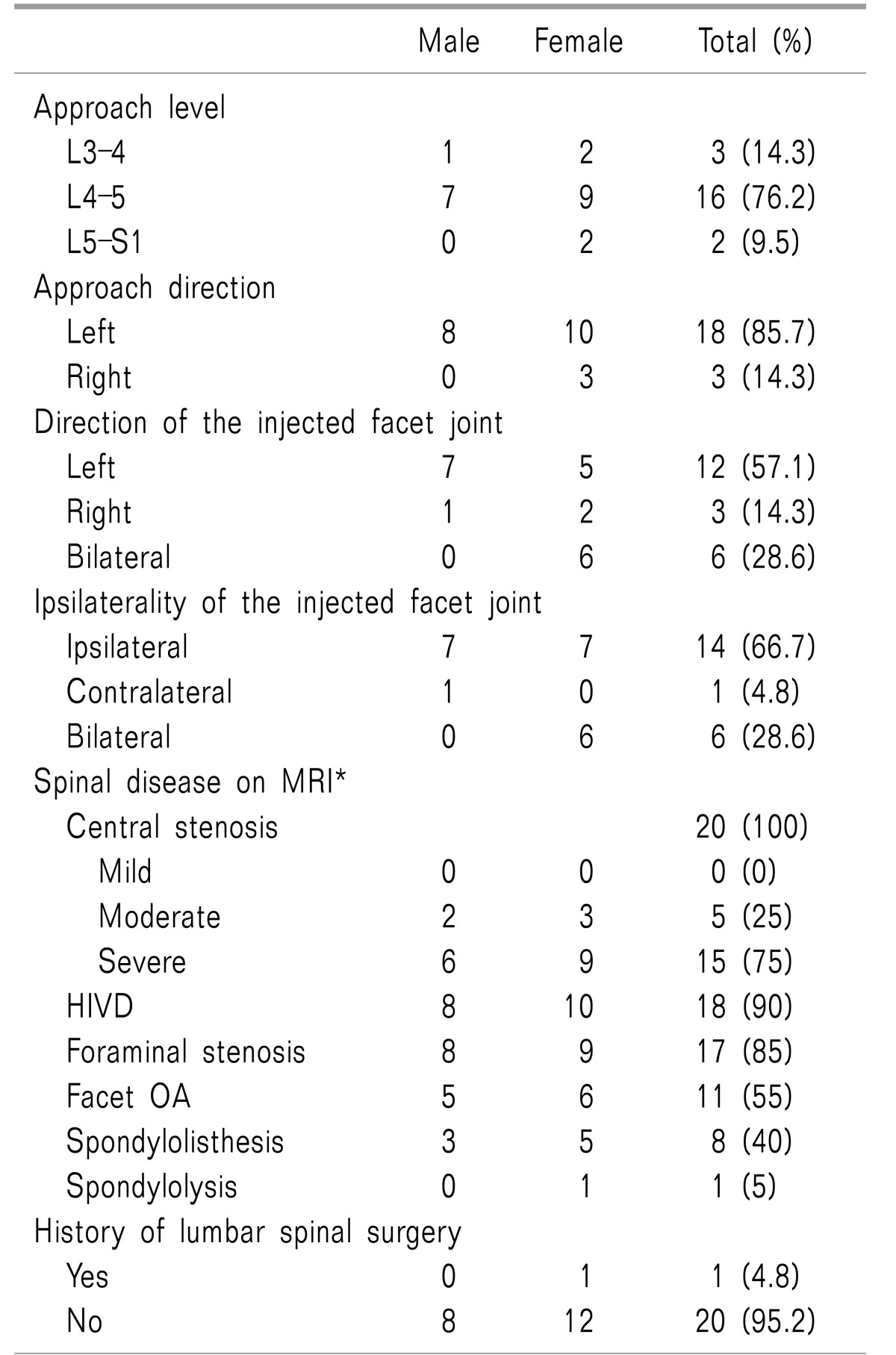
From December 2015 to May 2017, among 662 interlaminar lumbar ESIs, a total of 24 cases (21 patients) were selected. The incidence of unintentional lumbar facet joint injection was 3.6%. Among the 21 patients, there were 13 female patients (61.9%) and eight males (38.1%), so the proportion of females was higher than that of males. The average age in the overall patient population was 68.47 years. The average age in male patients was 68.25 years, and the average age in females was 68.62 years. Among the 21 patients, three (14.3%) experienced two facet joint injections in the same pattern during this study.
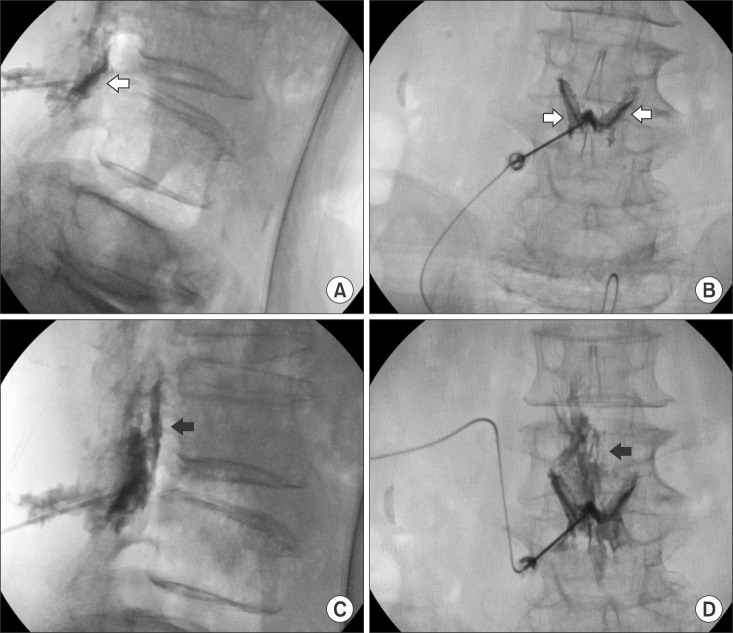
After the facet joint injection, the operator placed the needle deeper into the posterior epidural space without changing the direction, or tried to insert the needle into the adjacent level. The contrast pattern within the posterior epidural space was then identified by the operator. Sixteen of 21 patients (76.2%) showed contrast at the L4-L5 level, three patients (14.3%) at L3-L4, and two patients (9.5%) at L5-S1. In 18 patients (85.7%), the direction of the needle approach was left, and in the others (14.3%), it was right. Fourteen of the 21 patients (66.7%) were injected in the facet joint ipsilaterally to the needle approach. Six patients (28.6%) were injected bilaterally, and one patient (4.8%) was injected contralaterally. The contrast pattern in the facet joint has a sigmoid or ovoid shape, confined to the vicinity of the facet joint (
Fig. 1A, B) [
2].
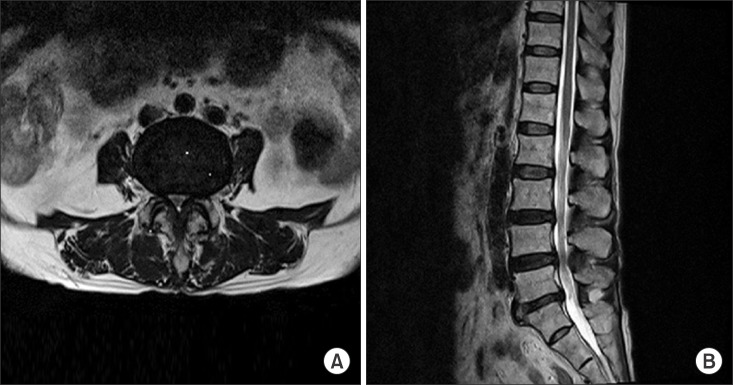
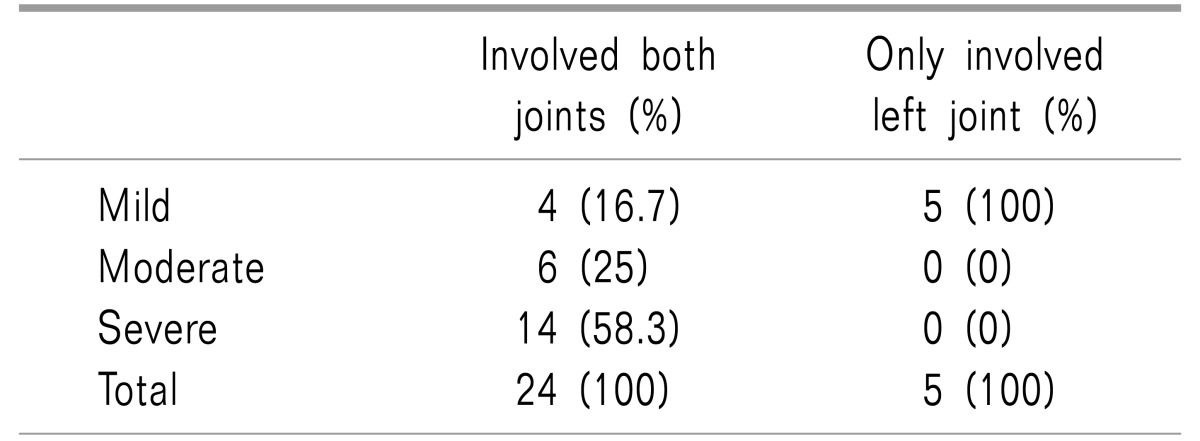
Twenty of 21 patients (95.2%) had an MRI before the interlaminar ESI. All of these patients (100%) had central stenosis, 18 patients (90%) had HIVD, 17 patients (85%) had foraminal stenosis, 11 patients (55%) had facet degenerdegenerative changes, eight patients (40%) had spondylolisthesis, and one patient (5%) had spondylolysis. Among the patients with central stenosis, 15 patients (75%) had severe stenosis, five (25%) had moderate stenosis, and there were no patients with mild stenosis. Among the 17 patients with the foraminal stenosis, 12 patients (70.6%) had it on both sides and five patients (29.4%) had it only on the left side. Of the 24 facet joints of the 12 patients with foraminal stenosis on both sides, 14 joints (58.3%) were severe, six (25%) were moderate, and four joints (16.7%) were mild. Of the five joints from the five patients with left foraminal stenosis, all of the joints (100%) were mild. However, only one patient (4.8%) underwent a laminectomy at L4-L5.
Go to :

DISCUSSION
In this study, unintentional lumbar facet joint blocks during ESI were commonly found to be ipsilateral in severe central stenosis in females.
ESI increases in elderly patients who have multiple spinal diseases and it is difficult to perform on them. The appropriate location of the needle tip within the posterior epidural space can be assessed in the lateral fluoroscopic view. In the lateral view, the appearance (flow of contrast material) and feeling (loss of resistance) are methods to evaluate an appropriate epidural injection [
23]. The typical epidural injection has a crescent contrast pattern delineating the posterior epidural space that can spread into the anterior epidural space and diffuse cranially or caudally for at least one vertebral segment (
Fig. 1C) [
2]. However, uunintentional facet joint injections show sigmoid or ovoid contrast patterns that are confined to one vertebra in the lateral view and are ipsilateral or bilateral in the AP view (butterfly pattern;
Fig. 1A, B). Unintentional facet joint injection during a fluoroscopically guided interlaminar ESI is not common, but it may mimic a proper epidural injection. So recognizing the imaging features of facet joint injections permits the operator to move the needle tip forward and increase the success rate of ESIs [
2].
There are only a few case studies, and it is not easy to understand the characteristic tendencies of unintentional facet joint injection. In a study by Huang et al. [
2], the imaging features of unintentional facet joint injection during an interlaminar ESI were described and identified in 42 cases based on a text search of 6,631 interlaminar ESI reports (0.6% positive rate). Another study, Lehman et al. [
4], also mentioned that the incidence of unintentional lumbar facet joint injections during an interlaminar ESI was low (1.2% positive rate). Our results showed a similar result (3.6%).
In a study by Huang et al. [
2], the proportion of the female groups was higher than that of males (male:female = 2:6), and the average age in the overall patient population was 66.1 years old. The level of L3-4 was the most injected site of the facet joints (50%). The most commonly used direction for injecting the facet joint was ipsilateral (62.5%). However, there were no statistically significant differences among the injection sites [
3]. Our results were similar to the previous study. In our study, the level of L4-L5 was the most injected site for the facet joints (76.2%).
The phenomenon of facet joint injection during LESI seems to be caused by the connection of the facet joint and extradural space. Okada et al. reported that 80% of arthrograms communicated with the facet joints and extradural space in the cervical space [
56]. Lehman et al. mentioned that the retrodural space, which is similar to the extradural space described in Okada's study, was posterior to the ligamentum flavum in the interlaminar space and connected with the posterior ligamentous complex (bilateral facet joints, adventitial interspinous bursa, and retrodural cyst) [
47]. Pars interarticularis defects are often a contributing factor that connect with adjacent ipsilateral joints [
48]. In a previous study, the facet joint capsule formed an anteromedial joint recess into the ligamentum flavum [
9], and Xu et al. [
10] mentioned that the facet joint capsule can extend medially or dorsally to the ligamentum flavum. Consequently, facet joint injection may occur when the contrast material is injected outside the dura due to the connection between these structures.
Previous studies have shown that a patient's spinal disease may affect unintentional facet joint injection. In a cadaveric study, McCormick et al. [
8] mentioned that facet arthrograms in patients with lumbar spondylolysis show the spread of contrast material through the pars interarticularis defects into the adjacent ipsilateral facet joint space and across the midline into the contralateral joint space. Maldague et al. [
11] mentioned that channels between the pars interarticularis defects in patients with lumbar spondylolysis can connect with each facet joint. Thus, the spondylolysis can lead to an unintentional lumbar facet joint injection during interlaminar ESI, but there are few articles about other spinal diseases that can contribute to unintentional lumbar facet joint injection. In our study, we analyzed the patients' spinal diseases on the lumbar MRI at the same level of their injections. All of the patients (100%) had central stenosis, HIVD (90%), and/or foraminal stenosis (85%), which were not directly relevant to the facet joints. Facet joint osteoarthritis (55%), spondylolisthesis (40%), and spondylolysis (5%), which are directly relevant to the facet joints, were less commonly seen than the other diseases. Furthermore, most patients had a severe grade of the central and foraminal stenosis. Judging from these findings, it appears that central stenosis, HIVD, and foraminal stenosis may cause a narrowing of the retrodural space so that the injection into the facet joint recess may happen more easily.
Only one anesthesiologist administered all of the procedures, and our results could be affected by the physician's skill level. Because patients were selected by our physicians who administered the procedure to them, our study was prone to referral bias. Furthermore, we checked only levels of needle approach on the MRIs, but other spinal diseases at adjacent levels of the needle approach could have affected the unintentional facet joint injection because the lumbar spine is related to other areas. Our study was a retrospective analysis and we could not compare the results with a control group. Thus, we could not determine whether our study results were statistically significant.
Patients who have undergone the unintentional lumbar facet joint injection during interlaminar ESI had central spinal stenosis disease on MRI. Not only is the spinal disease associated with the facet joint directly, but also the spinal diseases associated with narrowing of the retrodural space, could affect the unintentional facet joint injection. The contrast pattern should be carefully examined to distinguish between the epidural space and facet joint. Thus, in the future, additional research is likely to be needed and should include more cases and a control group.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download