1. Evans RW, Armon C, Frohman EM, Goodin DS. Assessment: prevention of post-lumbar puncture headaches: report of the therapeutics and technology assessment subcommittee of the american academy of neurology. Neurology. 2000; 55:909–914. PMID:
11061243.

2. Oedit R, van Kooten F, Bakker SL, Dippel DW. Efficacy of the epidural blood patch for the treatment of post lumbar puncture headache BLOPP: a randomised, observer-blind, controlled clinical trial [ISRCTN 71598245]. BMC Neurol. 2005; 5:12. PMID:
15998467.

3. Arevalo-Rodriguez I, Ciapponi A, Roqué i Figuls M, Muñoz L, Bonfill Cosp X. Posture and fluids for preventing post-dural puncture headache. Cochrane Database Syst Rev. 2016; 3:CD009199. PMID:
26950232.

4. Boonmak P, Boonmak S. Epidural blood patching for preventing and treating post-dural puncture headache. Cochrane Database Syst Rev. 2010; CD001791. PMID:
20091522.

5. Desai MJ, Dave AP, Martin MB. Delayed radicular pain following two large volume epidural blood patches for postlumbar puncture headache: a case report. Pain Physician. 2010; 13:257–262. PMID:
20495590.
6. Nair AS, Rayani BK. Sphenopalatine ganglion block for relieving postdural puncture headache: technique and mechanism of action of block with a narrative review of efficacy. Korean J Pain. 2017; 30:93–97. PMID:
28416992.

7. Mojica J, Mo B, Ng A. Sphenopalatine ganglion block in the management of chronic headaches. Curr Pain Headache Rep. 2017; 21:27. PMID:
28432602.

8. Cho JC, Haun DW, Kettner NW, Scali F, Clark TB. Sonography of the normal greater occipital nerve and obliquus capitis inferior muscle. J Clin Ultrasound. 2010; 38:299–304. PMID:
20544865.
9. Natsis K, Baraliakos X, Appell HJ, Tsikaras P, Gigis I, Koebke J. The course of the greater occipital nerve in the suboccipital region: a proposal for setting landmarks for local anesthesia in patients with occipital neuralgia. Clin Anat. 2006; 19:332–336. PMID:
16258972.

10. Loukas M, El-Sedfy A, Tubbs RS, Louis RG Jr, Wartmann CH, Curry B, et al. Identification of greater occipital nerve landmarks for the treatment of occipital neuralgia. Folia Morphol (Warsz). 2006; 65:337–342. PMID:
17171613.
11. Güvençer M, Akyer P, Sayhan S, Tetik S. The importance of the greater occipital nerve in the occipital and the suboccipital region for nerve blockade and surgical approaches: an anatomic study on cadavers. Clin Neurol Neurosurg. 2011; 113:289–294. PMID:
21208741.

12. Ducic I, Moriarty M, Al-Attar A. Anatomical variations of the occipital nerves: implications for the treatment of chronic headaches. Plast Reconstr Surg. 2009; 123:859–863. PMID:
19319048.

13. Naja ZM, El-Rajab M, Al-Tannir MA, Ziade FM, Tawfik OM. Repetitive occipital nerve blockade for cervicogenic headache: expanded case report of 47 adults. Pain Pract. 2006; 6:278–284. PMID:
17129309.

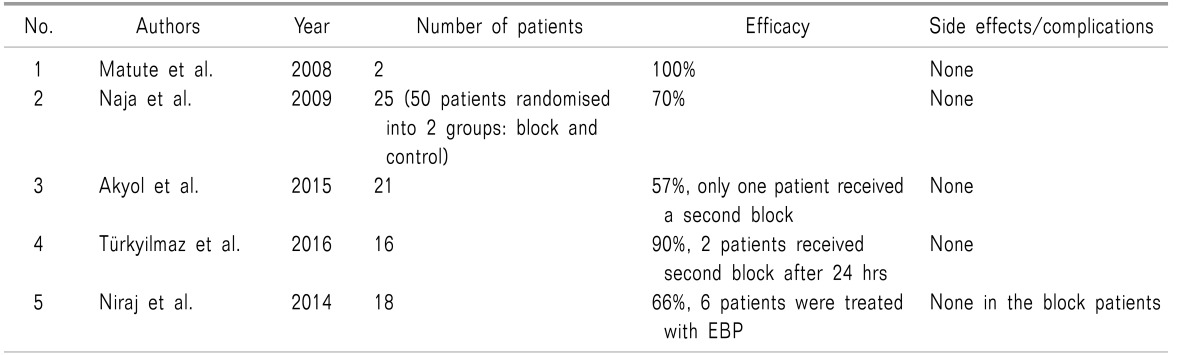
14. Naja Z, Al-Tannir M, El-Rajab M, Ziade F, Baraka A. Nerve stimulator-guided occipital nerve blockade for postdural puncture headache. Pain Pract. 2009; 9:51–58. PMID:
19019052.

15. Eom KS, Kim TY. Greater occipital nerve block by using transcranial Doppler ultrasonography. Pain Physician. 2010; 13:395–396. PMID:
20648209.
16. Walker KJ, McGrattan K, Aas-Eng K, Smith AF. Ultrasound guidance for peripheral nerve blockade. Cochrane Database Syst Rev. 2009; CD006459. PMID:
19821368.

17. Greher M, Moriggl B, Curatolo M, Kirchmair L, Eichenberger U. Sonographic visualization and ultrasound-guided blockade of the greater occipital nerve: a comparison of two selective techniques confirmed by anatomical dissection. Br J Anaesth. 2010; 104:637–642. PMID:
20299347.

18. Zipfel J, Kastler A, Tatu L, Behr J, Kechidi R, Kastler B. Ultrasound-guided intermediate site greater occipital nerve infiltration: a technical feasibility study. Pain Physician. 2016; 19:E1027–E1034. PMID:
27676673.
19. Binici O, Kuyrukluyıldız U, Şahin M, Alagöl A, Yılmaz İ. Ultrasound-guided bilateral greater occipital nerve block for mass excision. Turk J Anaesthesiol Reanim. 2015; 43:437–439. PMID:
27366544.
20. Shim JH, Ko SY, Bang MR, Jeon WJ, Cho SY, Yeom JH, et al. Ultrasound-guided greater occipital nerve block for patients with occipital headache and short term follow up. Korean J Anesthesiol. 2011; 61:50–54. PMID:
21860751.

21. Ashkenazi A, Levin M. Greater occipital nerve block for migraine and other headaches: is it useful? Curr Pain Headache Rep. 2007; 11:231–235. PMID:
17504651.

22. Selekler MH. Greater occipital nerve blockade: trigeminicervical system and clinical applications in primary headaches. Agri. 2008; 20:6–13.
23. Blumenfeld A, Ashkenazi A, Napchan U, Bender SD, Klein BC, Berliner R, et al. Expert consensus recommendations for the performance of peripheral nerve blocks for headaches: a narrative review. Headache. 2013; 53:437–446. PMID:
23406160.

24. Levin M. Nerve blocks in the treatment of headache. Neurotherapeutics. 2010; 7:197–203. PMID:
20430319.

25. Matute E, Bonilla S, Gironés A, Planas A. Bilateral greater occipital nerve block for post-dural puncture headache. Anaesthesia. 2008; 63:557–558. PMID:
18412667.

26. Uyar Türkyilmaz E, Camgöz Eryilmaz N, Aydin Güzey N, Moraloğlu Ö. Bilateral greater occipital nerve block for treatment of post-dural puncture headache after caesarean operations. Braz J Anesthesiol. 2016; 66:445–450. PMID:
27591456.

27. Niraj G, Kelkar A, Girotra V. Greater occipital nerve block for postdural puncture headache (PDPH): a prospective audit of a modified guideline for the management of PDPH and review of the literature. J Clin Anesth. 2014; 26:539–544. PMID:
25441250.

28. Akin Takmaz S, Unal Kantekin C, Kaymak C, Başar H. Treatment of post-dural puncture headache with bilateral greater occipital nerve block. Headache. 2010; 50:869–872. PMID:
20353435.

29. Naja ZM, El-Rajab M, Al-Tannir MA, Ziade FM, Tawfik OM. Occipital nerve blockade for cervicogenic headache: a double-blind randomized controlled clinical trial. Pain Pract. 2006; 6:89–95. PMID:
17309715.

30. Akyol F, Binici O, Kuyrukluyildiz U, Karabakan G. Ultrasound-guided bilateral greater occipital nerve block for the treatment of post-dural puncture headache. Pak J Med Sci. 2015; 31:111–115. PMID:
25878625.

31. Afridi SK, Shields KG, Bhola R, Goadsby PJ. Greater occipital nerve injection in primary headache syndromes--prolonged effects from a single injection. Pain. 2006; 122:126–129. PMID:
16527404.

32. Strauss L, Loder E, Rizzoli P. Transient facial nerve palsy after occipital nerve block: a case report. Headache. 2014; 54:1651–1655. PMID:
24913733.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download