1. Chen XT, Pitis P, Liu G, Yuan C, Gotchev D, Cowan CL, et al. Structure-activity relationships and discovery of a G protein biased µ opioid receptor ligand, [(3-methoxythiophen-2-yl)methyl]({2-[(9R)-9-(pyridin-2-yl)-6-oxaspiro-[4.5]de can-9-yl]ethyl})amine (TRV130), for the treatment of acute severe pain. J Med Chem. 2013; 56:8019–8031. PMID:
24063433.

2. Williams JT, Ingram SL, Henderson G, Chavkin C, von Zastrow M, Schulz S, et al. Regulation of µ-opioid receptors: desensitization, phosphorylation, internalization, and tolerance. Pharmacol Rev. 2013; 65:223–254. PMID:
23321159.

3. Fredriksson R, Lagerström MC, Lundin LG, Schiöth HB. The G-protein-coupled receptors in the human genome form five main families. Phylogenetic analysis, paralogon groups, and fingerprints. Mol Pharmacol. 2003; 63:1256–1272. PMID:
12761335.

4. Kochman K. Superfamily of G-protein coupled receptors(GPCRs)--extraordinary and outstanding success of evolution. Postepy Hig Med Dosw (Online). 2014; 68:1225–1237. PMID:
25380205.

5. Schiöth HB, Fredriksson R. The GRAFS classification system of G-protein coupled receptors in comparative perspective. Gen Comp Endocrinol. 2005; 142:94–101. PMID:
15862553.

6. Smith HS. Peripherally-acting opioids. Pain Physician. 2008; 11:S121–S132. PMID:
18443636.

7. Sehgal N, Smith HS, Manchikanti L. Peripherally acting opioids and clinical implications for pain control. Pain Physician. 2011; 14:249–258. PMID:
21587328.
8. Burness CB, Keating GM. Oxycodone/naloxone prolonged-release: a review of its use in the management of chronic pain while counteracting opioid-induced constipation. Drugs. 2014; 74:353–375. PMID:
24452879.

9. Morlion B, Clemens KE, Dunlop W. Quality of life and healthcare resource in patients receiving opioids for chronic pain: a review of the place of oxycodone/naloxone. Clin Drug Investig. 2015; 35:1–11.

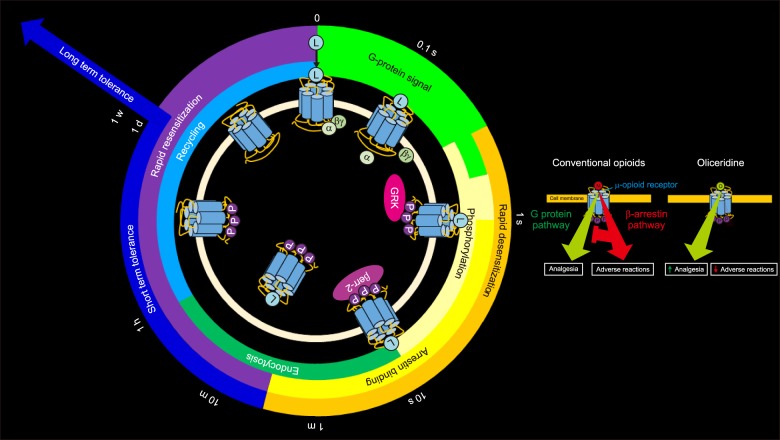
10. Violin JD, Crombie AL, Soergel DG, Lark MW. Biased ligands at G-protein-coupled receptors: promise and progress. Trends Pharmacol Sci. 2014; 35:308–316. PMID:
24878326.

11. Bohn LM, Lefkowitz RJ, Gainetdinov RR, Peppel K, Caron MG, Lin FT. Enhanced morphine analgesia in mice lacking beta-arrestin 2. Science. 1999; 286:2495–2498. PMID:
10617462.

12. Bohn LM, Gainetdinov RR, Lin FT, Lefkowitz RJ, Caron MG. Mu-opioid receptor desensitization by beta-arrestin-2 determines morphine tolerance but not dependence. Nature. 2000; 408:720–723. PMID:
11130073.

13. Raehal KM, Walker JK, Bohn LM. Morphine side effects in beta-arrestin 2 knockout mice. J Pharmacol Exp Ther. 2005; 314:1195–1201. PMID:
15917400.
14. Soergel DG, Subach RA, Sadler B, Connell J, Marion AS, Cowan CL, et al. First clinical experience with TRV130: pharmacokinetics and pharmacodynamics in healthy volunteers. J Clin Pharmacol. 2014; 54:351–357. PMID:
24122908.

15. Soergel DG, Subach RA, Burnham N, Lark MW, James IE, Sadler BM, et al. Biased agonism of the µ-opioid receptor by TRV130 increases analgesia and reduces on-target adverse effects versus morphine: a randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Pain. 2014; 155:1829–1835. PMID:
24954166.

16. Fossler M, Sadler B, Farrell C, Burt D, Pitsiu M, Skobieranda F, et al. (342) Oliceridine (TRV130), a novel µ receptor G protein pathway selective modulator (µ-GPS), demonstrates a predictable relationship between plasma concentrations and pain relief. I: development of a pharmacokinetic/pharmacodynamic (PK/PD) model. J Pain. 2016; 17:S61.

17. Fossler M, Sadler B, Farrell C, Burt D, Pitsiu M, Skobieranda F, et al. (343) Oliceridine (TRV130), a novel µ receptor G protein pathway selective modulator (µ-GPS), demonstrates a predictable relationship between plasma concentrations and pain relief. II: simulation of potential dosing regimens using a pharmacokinetic/pharmacodynamic (PK/PD) model. J Pain. 2016; 17:S61.

18. Viscusi E, Minkowitz H, Webster L, Soergel D, Burt D, Subach R, et al. (433) Rapid reduction in pain intensity with oliceridine (TRV130), a novel µ receptor G protein pathway selective modulator (µ-GPS), vs. morphine: an analysis of two phase 2 randomized clinical trials. J Pain. 2016; 17:S82–S83.

19. Singla N, Minkowitz H, Soergel D, Burt D, Skobieranda F. (432) Respiratory safety signal with oliceridine (TRV130), a novel µ receptor G protein pathway selective modulator (µ-GPS), vs morphine: a safety analysis of a phase 2b randomized clinical trial. J Pain. 2016; 17:S82.

20. Minkowitz H, Singla N, Soergel D, Burt D, Skobieranda F. (435) Nausea and vomiting with oliceridine (TRV130), a novel µ receptor G protein pathway selective modulator (µ-GPS), vs morphine: an analysis of tolerability from a phase 2b randomized clinical trial. J Pain. 2016; 17:S83.

21. Viscusi ER, Webster L, Kuss M, Daniels S, Bolognese JA, Zuckerman S, et al. A randomized, phase 2 study investigating TRV130, a biased ligand of the µ-opioid receptor, for the intravenous treatment of acute pain. Pain. 2016; 157:264–272. PMID:
26683109.

22. Madariaga-Mazón A, Marmolejo-Valencia AF, Li Y, Toll L, Houghten RA, Martinez-Mayorga K. Mu-Opioid receptor biased ligands: a safer and painless discovery of analgesics? Drug Discov Today. 2017; 22:1719–1729. PMID:
28743488.

23. Pierce KL, Premont RT, Lefkowitz RJ. Seven-transmembrane receptors. Nat Rev Mol Cell Biol. 2002; 3:639–650. PMID:
12209124.

24. Jacoby E, Bouhelal R, Gerspacher M, Seuwen K. The 7 TM G-protein-coupled receptor target family. ChemMedChem. 2006; 1:760–782.
25. McCudden CR, Hains MD, Kimple RJ, Siderovski DP, Willard FS. G-protein signaling: back to the future. Cell Mol Life Sci. 2005; 62:551–577. PMID:
15747061.

26. Patel TB. Single transmembrane spanning heterotrimeric G protein-coupled receptors and their signaling cascades. Pharmacol Rev. 2004; 56:371–385. PMID:
15317909.

27. Whalen EJ, Rajagopal S, Lefkowitz RJ. Therapeutic potential of β-arrestin- and G protein-biased agonists. Trends Mol Med. 2011; 17:126–139. PMID:
21183406.

28. Kliewer A, Reinscheid RK, Schulz S. Emerging paradigms of G protein-coupled receptor dephosphorylation. Trends Pharmacol Sci. 2017; 38:621–636. PMID:
28478994.

29. Dang VC, Christie MJ. Mechanisms of rapid opioid receptor desensitization, resensitization and tolerance in brain neurons. Br J Pharmacol. 2012; 165:1704–1716. PMID:
21564086.

30. Allouche S, Noble F, Marie N. Opioid receptor desensitization: mechanisms and its link to tolerance. Front Pharmacol. 2014; 5:280. PMID:
25566076.

31. Wright JM. The double-edged sword of COX-2 selective NSAIDs. CMAJ. 2002; 167:1131–1137. PMID:
12427705.
32. Del Vecchio G, Spahn V, Stein C. Novel opioid analgesics and side effects. ACS Chem Neurosci. 2017; 8:1638–1640. PMID:
28603962.

33. Manglik A, Lin H, Aryal DK, McCorvy JD, Dengler D, Corder G, et al. Structure-based discovery of opioid analgesics with reduced side effects. Nature. 2016; 537:185–190. PMID:
27533032.

34. Siuda ER, Carr R 3rd, Rominger DH, Violin JD. Biased mu-opioid receptor ligands: a promising new generation of pain therapeutics. Curr Opin Pharmacol. 2017; 32:77–84. PMID:
27936408.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download