Abstract
Background
To compare the effects of adding two different doses of dexamethasone on the duration and quality of the fascia iliaca block in patients undergoing proximal femoral fracture surgery.
Methods
A total of 60 patients (age 18–70 years) undergoing proximal femoral nailing surgery under spinal anesthesia were given fascia iliaca block after random assignment to one of the two groups: Group H received an injection of levobupivacaine (0.5%) 28 ml with 2 ml (8 mg) dexamethasone, and Group L received an injection of levobupivacaine (0.5%) 28 ml with dexamethasone 1 ml (4 mg) with 1 ml normal saline. Assessment of the duration of analgesia and the total tramadol requirement over 48 hours were noted after a successful block.
Results
The duration of analgesia was found to be significantly longer in Group H (17.02 ± 0.45 h) than in the Group L patients (14.29 ± 0.45 h) with a p-value of 0.000. Postoperative analgesic requirement (amount of tramadol in mg) was significantly higher in Group L (Q2: 200.0; IQR: 100.0, 200.0) as compared to Group H (Q2: 100.0; IQR: 100.0, 200.0) with a p-value of 0.034. No patient showed any sign of neurotoxicity.
Conclusions
Dexamethasone, in a dose of 8 mg, is superior to 4 mg when used as an adjuvant with levobupivacaine in the FIB. Though both prolonged analgesia and were effective in reducing oral/intravenous analgesics, 8 mg dexamethasone can be recommended as a more efficacious adjuvant to local anesthetics in the FIB.
Pain is the most dreaded associated feature of hip fractures, which is even more intense immediately after fracture correction surgery [1]. To improve analgesia and facilitate mobilization, regional anesthesia is a rescue technique which may be used alone or as an adjunct to general anesthesia. Positioning for neuraxial blocks in patients with a fractured femur is always challenging because even slight overriding of the fracture ends is intensely painful [2].
Local anesthetics (LA) have been used traditionally for the peripheral nerve blocks, but alone they are limited due to a shorter duration of action. To prolong the duration of action, several additives have been studied in the literature with varying results [3]. Corticosteroids are the new addendum to the list of additives. A single dose of Dexamethasone is found to be safe with rare adverse effects with short-term use (> 24 h) [4]. Most studies used dexamethasone in a dose of 8 mg to augment peripheral nerve block analgesia [4567]. Some studies have used doses of less than 8 mg of dexamethasone and shown satisfactory outcome [8]. A systematic review by Choi et al. [9] demonstrates the beneficial effects of the addition of dexamethasone to LA for peripheral nerve blocks. The same meta-analysis also reported no dexamethasone-induced neuronal damage. In a study, Williams and co-workers [10] showed that dexamethasone did not result in increased neurotoxicity when used as an adjuvant to Ropivacaine. Moreover, an in vitro study by Ma et al. [11] actually demonstrates that dexamethasone decreases the neurotoxicity of bupivacaine.
Here we attempt to compare the effects of the use of 4 mg dexamethasone versus 8 mg as an adjuvant to 0.5% levobupivacaine in the fascia iliaca block (FIB). The present work is a prospective, randomized study examining the analgesic properties of two different doses of dexamethasone with levobupivacaine.
The present study is a randomized control trial (RCT). The study involved two groups–one group being the control group (H) receiving the tested anesthesia procedure (L-Bupivacaine with 8 mg dexamethasone), and the other group (L) receiving L-Bupivacaine with 4 mg dexamethasone (low dose). It was conducted at a tertiary care center in Eastern India, in the operation theatre and ward of the orthopedics department, by the department of anesthesia. The institutional ethical committee approved the study. A written informed consent from the participants was obtained before including them in the study.
It was calculated that a total of 54 patients were needed for this two-treatment, parallel-design study. The probability was 85 percent that the study would detect a treatment difference at a two-sided 0.05 significance level when the true difference between treatments is 0.842 times the standard deviation. Considering a dropout rate of 20%, a total of 65 cases, if allocated for the study, would be sufficient to close the study; however, we had taken 72 cases for our study.
Inclusion criteria included adult patients (18–70 years) of both sex and having American Society of Anesthesiologists (ASA) grade I or II, with scheduled hip surgeries under spinal anesthesia. The patients had trochanteric fractures and were proposed candidates for proximal femoral nailing by surgeons with comparable surgical skills. These were randomly allocated into two groups (H and L) using a computer-generated random number sequence. Allocation concealment was also ensured through sealed, opaque envelops (group allocation being invisible even on an X-ray view box). Patients with a prior history of hypersensitivity reaction to dexamethasone/levobupivacaine, with abnormal coagulation parameters, previous opioid therapy, psychiatric disorders, poly-trauma, and those requiring/converted to general anesthesia, were excluded from the study. Similarly, patients having local infection at the site of the block, inguinal hernia, and femoral artery graft were also precluded. Further, those patients who had satisfactory analgesia (comfortable while positioning for spinal anesthesia after the block) were included in the study.
The two groups received treatments as discussed below. Group L received 28 ml of 0.5% levobupivacaine plus 1 ml of normal saline, with 4 mg (1 ml) dexamethasone; Group H received 28 ml of 0.5% levobupivacaine plus dexamethasone 8 mg (2 ml). Thus, a total volume of 30 mL of the mixture was used in each group to provide the highest rate of success in their FIB, administered using the ultrasound guided technique. An additional one ml of normal saline that was added in the L group acted to blind the participant and the anesthetist involved in the trial (double blinding).
After establishing intravenous access, standard ASA monitors were applied, and supplemental oxygen was provided at 2 L/min via nasal cannula. Moderate levels of sedation were provided by intravenous administration of midazolam 1 mg before the block.
The fascia iliaca compartment is a potential space between the posterior surface of the fascia iliaca (covering the iliacus muscle) and the anterior surface of the iliacus muscle and the psoas major muscle. Thus, the space is posterior to the femoral vessels which lie superficial to the fascia iliaca above the inguinal ligament, and continues in the lateral lacuna musculorum compartment below the inguinal ligament. The major nerves that are contained include the femoral, obturator, and lateral femoral cutaneous nerves. This closed compartment allows the local anesthetic to spread to affect these major nerves with one simple injection in the area around the groin and thigh.
The block was performed by either of the anesthesiologists (BS, RA), who were blinded to the preparation and randomization process in the preoperative room by using an ultrasound machine as follow: skin was disinfected and the transducer positioned to identify the femoral artery and the iliopsoas muscle and fascia iliaca. The transducer was moved laterally until the Sartorius' muscle was identified (Fig. 1A). After a skin wheal rose, the needle was inserted in the plane. The needle was passed through the fascia iliaca, and the fascia may be seen to snap back on the US image (Fig. 1B). After negative aspiration, 1–2 ml of prepared local anesthetic solution was injected to confirm the proper injection plane between the fascia and iliopsoas muscle (Fig. 1C). The needle was positioned until the separation of the fascia iliaca in a mediolateral direction from the point of injection (Fig. 1D).
The degree of the block was evaluated 30 m later by assessing the analgesia for making a position for spinal anesthesia. All surgeries were performed under spinal anesthesia with a standard dose of 15 mg of heavy bupivacaine. Proximal femur nail (PFN) surgeries were done for the study and three surgeons with similar skills performed them.
Oral administration of Acetaminophen 500 mg twice daily in all patients was given as a supplemental analgesic. Patients were given intravenous injection of 100 mg of tramadol as rescue analgesia for breakthrough pain (when the VAS score exceeded 3).
Duration of analgesia was reported as the time in hours from the time of performing the block to when the patients felt pain for the first time at an intensity of more than 3 on the VAS. The total dose of tramadol for the first 48 hours after the FIB was recorded. Also, patients were monitored for any neurotoxic adverse effects with complaints of heightened sensitivity to temperature variations, numbness, tingling, or impaired fine-motor movements. Long-term complications could not be assessed, which could include difficulty in walking.
Data was entered in IBM SPSS v 20.0 licensed to the institute and analyzed. Depending on the normality of the data (done using the Kolmogorov Smirnov test/Shapiro Wilk test), results were presented either in the form of mean with standard error (for a normal distribution) and median with inter-quartile range (for non-normal distribution). Comparison between the groups was done using the appropriate statistical test (t-test for normal distribution and Mann-Whitney U test for non-normal distribution). Categorical data were presented as numbers with a percentage (%). Significance was assessed at a 5% level of significance. Appropriate graphs were used to visualize the findings.
There were 72 surgical cases willing to participate in the study. Out of these, four were excluded in the initial phase (some did not meet inclusion criteria (n = 3), while one did not give consent (n = 1)). The rest (n = 68) were randomized and allocated to the two different intervention groups (Groups L and H), with a proper allocation concealment in place (n = 34 each). The interventions were applied to the cases and followed up. There was no loss to follow up in either group (n = 0). However, some of them were excluded from the study due to unsuccessful blocks, changes in surgical plans, or surgical time exceeding 4 hours in both groups (n = 8). Thus, a total of 60 patients were analyzed (n = 30 in each group). Details have been summarized using the CONSORT flow diagram (Fig. 2).
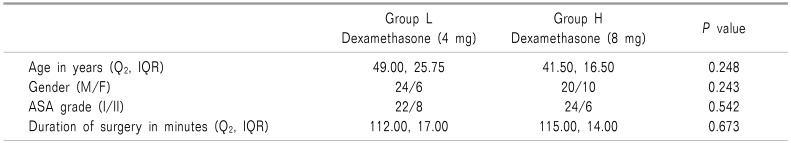
The average age of the patients in both the groups was similar and statistically not significant. Even the gender ratio and ASA grade were similar and non-significant. The duration of surgery was also similar between both the groups (Table 1).
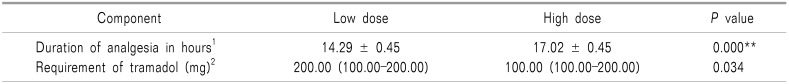
This ensures that randomization had been done properly and there is no selection bias. The duration of analgesia was, however, found to be significantly longer in Group H (17.02 ± 0.45 h) than group L (14.29 ± 0.45 h) with a P-value of 0.000 (Table 2).
Postoperative analgesic requirement (the amount of tramadol in mg) was assessed for the first and second postoperative days. Analgesic consumption for the first postoperative 48 h was found to be significantly higher in group L (Q2: 200.0; IQR: 100.0, 200.0) as compared to group H (Q2: 100.0; IQR: 100.0, 200.0) with a P-value of 0.034 (Table 2). No patient showed any sign of neurotoxicity.
Proximal femoral fractures are common fractures in the aging population owing to bone fragility [1]. Analgesia is the key component in their management in toto, starting from the pre-hospital, pre-operative to post-operative time periods. The fascia-iliaca block is a useful component of the multimodal analgesia arsenal. Ever since it was first described in 1989, it has now become routinely used to provide analgesia following surgical procedures in the hip, femur, and knee, as well as treatment for burns on the thigh and in pre-hospital treatment scenarios [23].
Ultrasound-guided FIB has increased its safety and efficacy [4]. Being easy to perform, it is also associated with minimal risk as the analgesic is injected at a safe distance from the femoral artery and femoral nerve. It blocks both the lateral cutaneous nerve of the thigh and femoral nerve, and allows patients to tolerate a sitting position with fractures [56]. Delirium is common in elderly patients with a fractured femur, and as pain is an important contributor, it can be effectively managed with adequate analgesia in the form of an FIB, which not only prevents delirium, but also has an opioid-sparing effect and allows increased mobility and a shorter hospital stay [7].
Steroids induce a degree of vasoconstriction and act by reducing local anesthetic absorption; they also increase the activity of inhibitory potassium channels on nociceptive C-fibers, thus decreasing their activity and modifying the membrane lipid phase equilibrium [8]. The half-life of dexamethasone is between 36 and 54 h, and its effects are most apparent in the first 48 h [1]. Dexamethasone as an adjuvant to epidural local anesthetics has been studied [12]. To date, no trial has reported neurotoxicity attributable to dexamethasone dosage.
In a study, Lee et al. [13] using a rat spared nerve injury (SNI) model, have shown that pre-operative infiltration of bupivacaine with dexamethasone as an adjuvant had a significantly better analgesic effect than did infiltration of bupivacaine or dexamethasone alone, and indicated that dexamethasone acts synergistically or additively with bupivacaine to exert a preemptive analgesic effect, but has no effect on its own. Block prolongation was observed when dexamethasone was combined with mepivacaine for supra-clavicular blocks [14]. Similarly, Cummings et al. [15] also observed that dexamethasone significantly prolonged the duration of ropivacaine and Bupivacaine when used for the inter-scalene block. Nallam [16] in their study comparing the various doses of dexamethasone (4 mg = low, 8 mg = high), found similar efficacy of analgesia prolongation in the inter-scalene block when used with levobupivacaine with the lower requirement of analgesia in first 48 hours in both groups. Similar comparative studies of different doses of dexamethasone in lower limb blocks are lacking, prompting us to undertake this study.
Suresh Kumar et al. [17] in their study on the FIB, have observed that when dexamethasone was added as an additive to plain bupivacaine, the duration of the block was prolonged to almost double (bupivacaine 7.85 ± 1.62 h; additional with 8 mg dexamethasone 16.33 ± 5.69 h; P < 0.05). The duration of the block with the addition of 8 mg dexamethasone in the study by Suresh Kumar et al. [17] was found to be similar to what we got in our study with a similar dose (17.02 ± 0.45 h, P > 0.05). In addition, we found that the duration of analgesia with 4 mg dexamethasone was 14.29 ± 2.45 h, which is statistically significant. In the same study by Suresh Kumar et al. [17] consumption of Tramadol was found to be higher in patients receiving plain bupivacaine than patients with dexamethasone (8 mg), which was statistically significant. In our study, when two different doses of dexamethasone were compared, patients with a higher dose of dexamethasone (8 mg) had a lower consumption of tramadol then with those receiving a lower dose (4 mg), which implies that the effect of dexamethasone is dose-related in the FIB, as the duration of analgesia increased and the requirement of analgesics decreased with higher doses of dexamethasone, statistically.
Woo et al. [18] compared the interscalene ultrasoundguided brachial plexus blocks using a volume of 12 ml ropivacaine with a graded dose of dexamethasone and found that 7.5 mg and 5 mg produced a similar effect, but a better effect than 2.5 mg. This means the “effective D/LA” (dexamethasone/local anaesthetic of 12 ml) concentration was reached with 5 mg and remained the same with 7.5 mg, but was suboptimal with 2.5 mg. Similarly, a meta-analysis for brachial plexus blocks by Knezevic and co-worker [19] found similar efficacy for 4 mg and 8 mg of dexamethasone. In the FIB, with a volume of 40 ml LA, Suresh Kumar et al. [17], using 8 mg dexamethasone, showed a beneficial effect. However, in our comparative study of the FIB using 30 ml of LA solution, we found 8 mg dexamethasone to be advantageous over 4 mg. Thus “effective D/LA” (dexamethasone/local anaesthetic of 30 ml) was better in the 8 mg group than the 4 mg group, which could be the possible reason for the significant difference between them in a higher volume block like the FIB.
Decreased analgesic consumption has inherited the advantages of reducing multiple issues like gastrointestinal upset, delirium, etc., all leading to early ambulation and a decreased hospital stay. The study by Srinivas and his team found similar efficacy in the two doses of dexamethasone with bupivacaine in interscalene brachial plexus blocks, which is different in our study of the fascia iliaca block. The possible reason could be the compact arrangement of nerve fibers in the brachial plexus, compared to the distant location of nerve fibers in the fascia iliaca block. As the FIB is a fascia block, the drug injection is away from the nerves, hence the distribution and concentration of drugs may vary, sparing some nerve fibers. Further studies are needed to evaluate the same issue in lower limb fractures, with individual nerve blocks to confirm the drug (dexamethasone) response. Another shortcoming of our study was lack of long-term follow up for late-onset neurotoxicity.
To conclude, use of the FIB in patients with proximal femoral fractures provides analgesia for positioning during spinal anesthesia. Dexamethasone, in a dose of 8 mg, is superior to 4 mg when used as an adjuvant with levobupivacaine in the FIB. Due to both prolonged analgesia and effective reduction of oral/intravenous analgesics, 8 mg dexamethasone can be recommended as a more efficacious adjuvant to local anesthetics in the FIB.
References
1. Soles GL, Ferguson TA. Fragility fractures of the pelvis. Curr Rev Musculoskelet Med. 2012; 5:222–228. PMID: 22589010.

2. Cuignet O, Mbuyamba J, Pirson J. The long-term analgesic efficacy of a single-shot fascia iliaca compartment block in burn patients undergoing skin-grafting procedures. J Burn Care Rehabil. 2005; 26:409–415. PMID: 16151286.

3. Lopez S, Gros T, Bernard N, Plasse C, Capdevila X. Fascia iliaca compartment block for femoral bone fractures in prehospital care. Reg Anesth Pain Med. 2003; 28:203–207. PMID: 12772137.

4. Rahimzadeh P, Imani F, Sayarifard A, Sayarifard S, Faiz SH. Ultrasound-guided fascia iliaca compartment block in orthopedic fractures: bupivacaine 0.2% or 0.3%? Med J Islam Repub Iran. 2016; 30:433. PMID: 28210598.
5. Candal-Couto JJ, McVie JL, Haslam N, Innes AR, Rushmer J. Pre-operative analgesia for patients with femoral neck fractures using a modified fascia iliaca block technique. Injury. 2005; 36:505–510. PMID: 15755432.

6. Morau D, Lopez S, Biboulet P, Bernard N, Amar J, Capdevila X. Comparison of continuous 3-in-1 and fascia iliaca compartment blocks for postoperative analgesia: feasibility, catheter migration, distribution of sensory block, and analgesic efficacy. Reg Anesth Pain Med. 2003; 28:309–314. PMID: 12945024.

7. Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol. 2009; 10:127–133. PMID: 19690943.

8. Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID: 2167604.

9. Choi S, Rodseth R, McCartney C. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014; 112:427–439. PMID: 24413428.

10. Williams BA, Hough KA, Tsui BY, Ibinson JW, Gold MS, Gebhart GF. Neurotoxicity of adjuvants used in perineural anesthesia and analgesia in comparison with ropivacaine. Reg Anesth Pain Med. 2011; 36:225–230. PMID: 21519308.

11. Ma R, Wang X, Lu C, Li C, Cheng Y, Ding G, et al. Dexamethasone attenuated bupivacaine-induced neuron injury in vitro through a threonine-serine protein kinase B-dependent mechanism. Neuroscience. 2010; 167:329–342. PMID: 20038443.

12. Jebaraj B, Khanna P, Baidya DK, Maitra S. Efficacy of epidural local anesthetic and dexamethasone in providing postoperative analgesia: a meta-analysis. Saudi J Anaesth. 2016; 10:322–327. PMID: 27375389.

13. Lee JB, Choi SS, Ahn EH, Hahm KD, Suh JH, Leem JG, et al. Effect of perioperative perineural injection of dexamethasone and bupivacaine on a rat spared nerve injury model. Korean J Pain. 2010; 23:166–171. PMID: 20830261.

14. Parrington SJ, O'Donnell D, Chan VW, Brown-Shreves D, Subramanyam R, Qu M, et al. Dexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2010; 35:422–426. PMID: 20814282.

15. Cummings KC 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011; 107:446–453. PMID: 21676892.

16. Nallam SR. Interscalene brachial plexus block: comparison of efficacy of varying doses of dexamethasone combined with levobupivacaine: a double-blind randomised trial. J Evol Med Dent Sci. 2014; 3:6900–6908.

17. Suresh Kumar N, Kiran N, Ravi M, Sebastian D, Gowda Rm P. Dexamethasone as an additive to bupivacaine in fascia lliaca compartment block: a prospective, randomized and double blind study. J Clin Diagn Res. 2014; 8:GC05–GC08. PMID: 25302209.
18. Woo JH, Kim YJ, Kim DY, Cho S. Dose-dependency of dexamethasone on the analgesic effect of interscalene block for arthroscopic shoulder surgery using ropivacaine 0.5%: a randomised controlled trial. Eur J Anaesthesiol. 2015; 32:650–655. PMID: 25603389.

19. Knezevic NN, Anantamongkol U, Candido KD. Perineural dexamethasone added to local anesthesia for brachial plexus block improves pain but delays block onset and motor blockade recovery. Pain Physician. 2015; 18:1–14. PMID: 25675053.
Fig. 1
Ultrasound images. (A) Ultrasound image showing Sartorius muscle and Iliacus muscle with overlying fascia iliaca, (B) Ultrasound image showing in plane needle technique through fascia iliaca and the fascia may be seen to snap back (hollow arrow pointing). (C) Ultrasound image showing plane between fascia and iliopsoas muscle being separated by 1 ml of solution (hollow arrow pointing). (D) Ultrasound image showing drug spread and separation of fascia iliaca (hollow arrows pointing).





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download