Abstract
Meralgia paresthetica (MP) is a sensory mononeuropathy, caused by compression of the lateral femoral cutaneous nerve (LFCN) of thigh. Patients refractory to conservative management are treated with various interventional procedures. We report the first use of extended duration (8 minutes) pulsed radiofrequency of the LFCN in a case series of five patients with refractory MP. Four patients had follow up for 1–2 years, and one had 6 months follow up. All patients reported remarkable and long lasting symptom relief and an increase in daily life activities. Three patients came off medications and two patients required minimal doses of neuropathic medications. No complications were observed.
Meralgia paresthetica (MP) is a sensory mononeuropathy of multifactorial etiology, resulting in compression of the lateral femoral cutaneous nerve (LFCN) of the thigh with a reported incidence of 4.3/10,000 [12]. Symptoms vary from paresthesia and numbness to burning discomfort along the distribution of the LFCN. Diagnosis of MP is confirmed by either nerve conduction studies or a diagnostic nerve block to the LFCN. Management of MP involves a stepwise approach.
Firstly, identification of the precipitating factors, and treating the same, halts the progression of the disease, followed by pharmacotherapy with neuropathic pain medications to treat the existing symptoms. Conservative management provides satisfactory results in around 85% of patients [2]. Patients refractory to conservative management have been treated with various other interventional procedures, like local anaesthetic infiltration at the LFCN, pulsed radiofrequency (PRF) of the LFCN, alcohol infiltration around the LFCN, and surgical treatment, including decompression and transection of the nerve [2].
Infiltration of local anaesthetic to the LFCN provides excellent pain relief, but for a short duration. Alcohol mediated neurolysis has also shown promising results, but is often associated with differentiation pain, anaesthesia dolorosa, dysesthesia, etc [3]. Surgical transection of the LFCN results in permanent anaesthesia in the anterolateral portion of the thigh [4]. The use of PRF has emerged as a relatively new treatment option for MP refractory to conservative treatment [5]. Surgical transection of the LFCN can be avoided with the use of PRF, with an equally effective outcome and minimal complications. However, the evidence to support this is weak due to lack of randomized controlled trials (RCTs) or quasi-RCTs [6].
Recent literature has controversial results with regard to use of short duration PRF, specifically in terms of the duration of pain relief. This has questioned the optimum duration of PRF for refractory neuropathic pain [78]. Further on when conventional radiofrequency (CRF) was compared to with a short duration of PRF (2 minutes) for trigeminal neuralgia (TGN), no long term benefits with PRF were reported [8]. Hence, prolonged duration PRF (8–10 minutes) was used in recent case reports, one for TGN [9], a second for the saphenous nerve and a third for osteoarthritis of the knee [1011]. All the case reports showed a prolonged pain relief compared to short duration (2 minutes) PRF.
After a thorough review of the literature, we did not find any study using extended duration (8 minutes) PRF for management of MP. We report the first case series with a long term follow up highlighting the use of extended duration (8 minutes) PRF of the LFCN for MP refractory to conservative treatment.
This is a case series of five patients who presented to the pain clinic of our institute from July 2015 to February 2017 with refractory MP. Imaging studies like X-ray, ultrasound (US) of the pelvis, and MRI of pelvis and thigh were done to rule out correctable causes. Nerve conduction studies of all patients showed decreased sensory nerve action potentials (SNAP < 10 µV) and increased latency (> 3.0 ms) with side-to-side amplitude difference.
After the confirmation of MP, a written informed consent was obtained and a USG-guided diagnostic block of the LFCN with local anaesthetic, 0.5% bupivacaine, and methylprednisolone 40 mg was performed.
Patients were followed up after the diagnostic block for pain relief and reoccurrence of symptoms. All patients reported a reduction in symptoms of more than 50%. Following reoccurrence of symptoms, a written consent was obtained and US guided PRF was performed with a 22 G, 10 cm with 5 mm active tip radiofrequency (RF) needle. The LFCN was located with the high frequency (613 Hz) linear USG probe (M-Turbo® Ultrasound System; Sonosite International, Washington DC).
The probe was placed below and medial to the anterior superior iliac spine. The LFCN was found to lie between the fascia lata and fascia iliaca and above the sartorius muscle. The RF needle was directed towards the nerve under US guidance using in-plane approach with its final position between the two fascia.
Selective stimulation of sensory fibers (50 Hz) showed concordant pain between 0.3 and 0.5 V, which confirmed proper localization of the RF electrode. Motor stimulation was negative till 1.7 V. PRF was done for 8 minutes (45 V) with a maximum temperature of 42℃, and procedures were uneventful.
All patients were advised to exercise in the form of quadriceps stretching and hip extension and abduction. Patients were followed up at one month and then three monthly or as and when required after PFR for complications and reoccurrence of symptoms.
A 50-year-old male had a sudden onset of severe pain (visual analogue scale, VAS 8–9/10) in the anterolateral aspect of his right thigh for the last 1.5 years. On taking his history and investigation, no underlying cause was detected.
Initially the patient was prescribed acetaminophen and non-steroidal antiinflammatory drugs, the VAS score continued to be 8/10, and pain relief was obtained on and off on these medications.
The patient started having numbness two months after the onset of pain. Nerve conduction studies (NCV) of the LFCN showed decreased sensory nerve action potentials, with side-to-side amplitude differences. The patient was prescribed amitriptyline 20 mg once a day, and a good response was noted for 2 months. After two months, pain recurred (VAS:6/10) with slight numbness, and the patient also complained of sedation and dryness of the mouth since starting the medication.
A diagnostic block of the LFCN with local anaesthetic and a steroid was given and pain relief noted. Four months later the VAS score again increased to 7/10 for which PRF of the LFCN was performed and a prolonged relief was noted on follow up at 24 months. The patient came off medication four months post-PRF.
A 45-year-old presented with complaints of severe paresthesia and a burning sensation over the lateral aspect of his right thigh for the previous 8 months. The patient also complained of pain in his back and left leg with numbness in the big toe which was diagnosed as radicular pain in the distribution of the L5 and S1 nerve.
The patient was diagnosed with a prolapsed intervertebral disc on the left side, and was managed conservatively initially, followed by a transforaminal injection at L5 and S1 nerves. A good response to the back pain and posterior aspect of the leg pain was obtained, but the paresthesia and burning sensation persisted in the right lateral aspect of the thigh. The nerve conduction velocity of the LFCN revealed decreased amplitude in nerve action potential.
The patient was prescribed oral amitriptyline 20 mg once and pregabalin 75 mg twice a day. The patients persistently had a VAS score of 8/10 despite medications for 2 months. An LFCN block with local anesthetic and a steroid was given. Symptoms reoccurred after 2 months even with neuropathic medication and a post diagnostic block.
PRF of the LFCN was performed and pain relief was obtained with a VAS score of 3/10. Pregabalin was tapered and stopped and amitriptyline 20 mg once a day continued for 3 months, and then stopped. The patient had complete pain relief during the 1.5 years of follow up.
A 22-year-old presented with complaints of paresthesia, burning, and pain (VNRS) of the left lateral aspect of her thigh for the previous 6 months was diagnosed as MP on the nerve conduction velocity of the LFCN. She was prescribed gabapentin 100 mg twice a day which was increased up to 300 mg twice a day, over a period of three months but without any relief.
A diagnostic block of the LFCN was given with LA and a steroid. Good pain relief was obtained post block. The patient reported a reoccurrence of symptoms 1 month later. PRF of the LFCN was performed, subsequent to which she reported a VAS of 3/10 and medications were gradually reduced to gabapentin 100 mg once a day over a period of three months. Follow up after 1.3 years reported a VAS 1/10.
A 30-year-old male patient reported with severe numbness and paraesthesia (VNRS 9/10) on the anterolateral aspect of his left thigh for the previous 8 years following some weight lifting activities at the gym. The patient was on amitriptyline 25 mg once and pregabalin 150 mg twice a day for the previous six months before being referred to our pain clinic, but his VNRS score persisted at 9/10.
His nerve conduction velocity reported decreased sensations in the distribution of the left LFCN. A diagnostic block of the LFCN was performed with LA and a steroid with significant symptoms relief (VNRS 2/10). Four months following the diagnostic block, there was a reoccurrence of the symptoms.
PRF of the left LFCN caused symptom relief and he reported an absence of abnormal sensations on the affected side, which he reported had never had in the previous 8 years. Medications were tapered and stopped over a period of 3 months. Complete symptom relief lasted through the last follow up at 1 year.
A 60-year-old male patient with pain (VNRS score 7/10) on the left lateral aspect of his thigh for 2 years and was diagnosed with MP of the LFCN. A good response to neuropathic adjuncts pregabalin 150 mg twice and amitriptyline 10 mg once a day, as well as exercises, were obtained during the 8 months prior to his being referred to us.
An LFCN block with LA and a steroid provided good pain relief for 3.5 months, followed by a recurrence of symptoms. After this, PRF of the LFCN provided good relief at 3 months and complete pain relief at the last follow up at 6 months.
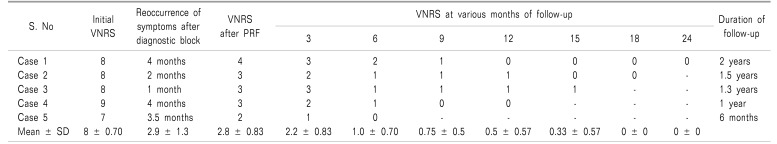
Mean ± SD age of the patients was 41.4 ± 15.32 (22–60 years) years. Four were males and one was female. Mean ± SD duration to the reoccurrence of symptoms after local anaesthetic and a steroid diagnostic block was 2.9 ± 1.3 months. Mean ± SD for the VAS score at baseline was 8 ± 0.70, and decreased remarkably after PRF and at follow up at 3, 6, 9, 12, 15, 18, and 24 months (Table 1).
None of the patients reported of any complications. All the patients reported an increase in daily life activities. Three patients had come off medications during the 3–6 months of follow up, and two patients required reduced doses of neuropathic medications.
MP was first described in 1885 by Hager and further in 1895 by Roth. It is implicated in causing nerve entrapment with the LFCN of the thigh. Patients commonly present at 30–40 years of age with a higher incidence in the male population [2].
Diagnosis of MP is based on clinical assessment and investigations which include: nerve conduction studies of LFCN, diagnostic block and when indicated imaging to rule various etiologies [1].
Management of MP involves a stepwise approach. Around 85% of patients effectively respond to oral neuropathic medications, whereas 10–15% of patients remain refractory [2]. Patients who do not respond to conservative management are treated by various interventional modalities such as local anaesthetic infiltration of the LFCN, alcohol mediated neurolysis, PRF to the LFCN of the thigh, and surgical treatment.
Few case reports and case series have demonstrated the use of PRF with 2 minutes' duration in patients with MP [61213]. However, use of short duration PRF has recently been debated. Recent literature reports in animal studies showed that increased duration of PRF, i.e. 8 minutes, leads to a significant decrease in tumor necrosis factor (TNF)-α and interleukin (IL)-6 at the site of inflammatory pain, as compared to 2 and 4 minutes [14]. Further, literature reports that short duration PRF for the trigeminal nerve required earlier repeat PRF [7], and did not yield any advantage over conventional radiofrequency [8], in terms of pain relief in patients.
Recently, extended duration PRF for both 8 and 6 minutes for trigeminal nerve [912], and 8 minutes for the saphenous nerve in chronic knee pain [10], was found to be associated with a longer duration of pain relief. Treatment of osteoarthritis in the knee with PRF to the genicular nerve for 10 minutes also had promising results [11].
Although the mechanism of prolonged duration PRF is still a matter of debate, recent literature has revealed that prolonged duration PRF provided long term relief to patients with chronic pain [9101112131415]. A thorough search of the literature did not reveal use of PRF of more than 2 minutes for refractory MP. So, we are demonstrating the first successful use of PRF with 8 minutes' duration for treating MP.
We achieved clinically significant results, with four patients remaining symptom free on long term follow up of 1–2 years and one patient at a 6 months follow up. The analgesic effect of PRF may be governed by various factors such as electrode position or duration. In the present case series, the use of USG on the LFCN of the thigh helped in visualizing the exact anatomical location of the LFCN and helped in controlling the electrode position [16].
We achieved concordant pain/paresthesia at 0.3–0.5 V sensory stimulation in all patients, suggesting the appropriate needle position near the LFCN. Although the literature does not reveal any RCT or large human study of the appropriate duration for prolonged PRF, we chose 8 minutes, as it has been used in the past for management of trigeminal nerve and the saphenous nerve for chronic knee pain [10]. Also, animal study reveals a significant decrease in inflammatory markers following 8 minutes of PRF at the site of pain as compared to 2 and 4 minutes [15]. This extended duration PRF most probably produced symptom relief for a long duration. None of the patients reported of any complications and patients remained symptom free on follow up. Three patients had no further requirement of neuropathic medications, and two patients reported remarkably reduced dosages.
We used local anesthetic along with a steroid for diagnostic blocks as per our institutional protocol, and this has been reported in the literature as well [1]. Our patients reported pain relief with a diagnostic block ranging from 1–4 months, which is in accordance with the reported duration of pain relief obtained by the local anesthetic and steroid combination used for the LFCN block [1].
A recent case series has also described alcohol neurolysis of the LFCN for intractable MP; but they reported the presence of hypoesthesia and numbness in two patients out of three [16]. The above mentioned complications were not reported in any of the patients in our case series, hence we would like to state that extended duration PRF is a safer invasive modality for treatment of intractable MP, and provides long term relief of symptoms.
The present case series reports that USG guided, extended duration PRF (8 minutes) is a safe modality for management of refractory cases of MP, providing good symptom relief on prolonged follow-up to 2 years, and no reported complication.
Sufficient evidence in terms of RCTs, using either short or extended duration PRF for management of refractory MP is lacking. Further RCTs may be required in the future to evaluate and prove the effectiveness of extended duration PRF for treatment of refractory MP. However, as the incidence of MP is low, and patients presenting to a single center are generally scarce, this limits the pain physicians to conduct randomized control trials to prove the beneficial effects of PRF for refractory MP. We advocate conducting a multicentre RCT to effectively prove the benefits of prolonged duration PRF.
References
1. Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013; 8:883–893. PMID: 24377074.
2. Patijn J, Mekhail N, Hayek S, Lataster A, van Kleef M, Van Zundert J. Meralgia Paresthetica. Pain Pract. 2011; 11:302–308. PMID: 21435164.

3. Chen CK, Phui VE, Saman MA. Alcohol neurolysis of lateral femoral cutaneous nerve for recurrent meralgia paresthetica. Agri. 2012; 24:42–44. PMID: 22399128.

4. de Ruiter GC, Wurzer JA, Kloet A. Decision making in the surgical treatment of meralgia paresthetica: neurolysis versus neurectomy. Acta Neurochir (Wien). 2012; 154:1765–1772. PMID: 22766927.

5. Lee JJ, Sohn JH, Choi HJ, Yang JS, Lee KH, Do HJ, et al. Clinical efficacy of pulsed radiofrequency neuromodulation for intractable meralgia paresthetica. Pain Physician. 2016; 19:173–179. PMID: 27008291.
6. Khalil N, Nicotra A, Rakowicz W. Treatment for meralgia paraesthetica. Cochrane Database Syst Rev. 2008; CD004159. PMID: 18646102.

7. Van Zundert J, Brabant S, Van de Kelft E, Vercruyssen A, Van Buyten JP. Pulsed radiofrequency treatment of the Gasserian ganglion in patients with idiopathic trigeminal neuralgia. Pain. 2003; 104:449–452. PMID: 12927617.

8. Erdine S, Ozyalcin NS, Cimen A, Celik M, Talu GK, Disci R. Comparison of pulsed radiofrequency with conventional radiofrequency in the treatment of idiopathic trigeminal neuralgia. Eur J Pain. 2007; 11:309–313. PMID: 16762570.

9. Thapa D, Ahuja V, Dass C, Verma P. Management of refractory trigeminal neuralgia using extended duration pulsed radiofrequency application. Pain Physician. 2015; 18:E433–E435. PMID: 26000693.
10. Akbas M, Luleci N, Dere K, Luleci E, Ozdemir U, Toman H. Efficacy of pulsed radiofrequency treatment on the saphenous nerve in patients with chronic knee pain. J Back Musculoskeletal Rehabil. 2011; 24:77–82.

11. Ahmed A. Prolonged pulsed radiofrequency ablation of genicular nerves of knee for intractable pain from knee osteoarthritis: a case report. J Pain Relief. 2016; 5:265.

12. Chua NH, Halim W, Beems T, Vissers KC. Pulsed radiofrequency treatment for trigeminal neuralgia. Anesth Pain Med. 2012; 1:257–261. PMID: 24904811.

13. Philip CN, Candido KD, Joseph NJ, Crystal GJ. Successful treatment of meralgia paresthetica with pulsed radiofrequency of the lateral femoral cutaneous nerve. Pain Physician. 2009; 12:881–885. PMID: 19787014.
14. Choi HJ, Choi SK, Kim TS, Lim YJ. Pulsed radiofrequency neuromodulation treatment on the lateral femoral cutaneous nerve for the treatment of meralgia paresthetica. J Korean Neurosurg Soc. 2011; 50:151–153. PMID: 22053239.

15. Ramzy EA, Khalil KI, Nour EM, Hamed MF, Taha MA. Evaluation of the effect of duration on the efficacy of pulsed radiofrequency in an animal model of neuropathic pain. Pain Physician. 2018; 21:191–198. PMID: 29565949.
16. Ahmed A, Arora D, Kochhar AK. Ultrasound-guided alcohol neurolysis of lateral femoral cutaneous nerve for intractable meralgia paresthetica: a case series. Br J Pain. 2016; 10:232–237. PMID: 27867513.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download