MATERIALS AND METHODS
This study was approved by the Institutional Review oard, and signed written consent was obtained from all participants who visited the pain clinic as outpatients. The procedure was conducted by one pain clinician who had sufficient experience and skill performing TFEB.
Patients enrolled in this study had no trauma history, fracture, or herniated nucleus pulposus before herpes zoster or PHN developed. Thoracic levels T2 to T11 were included in this study.
The procedure was conducted in the following sequence. The patient was placed in a prone position on the bed. A 4-cm distance from the midpoint of the spinous process was marked at the site of the procedure. Using the anteroposterior (AP) image on the fluoroscope, a 22-gauge spinal needle was advanced to the lateral margin of the vertebral body. After the needle was advanced 4–5 cm, the fluoroscope was switched to the lateral image [
4]. Using the lateral image, the needle tip was advanced to the mid-portion of the AP foraminal diameter. To avoid vessel puncture, the needle tip was usually located near the middle portion of the cephalocaudal foraminal diameter.
A total of 26 patients with herpes zoster or PHN were enrolled in this study. All participants received 1 ml, 2 ml, or 3 ml of contrast medium. Results were divided into Groups A, B and C based on the volume (1 ml, 2 ml, or 3 ml), with n = 26 for each group. To analyze spread according to the contrast volume, 1 ml of contrast medium was injected at 5 s intervals (once for 1 ml in Group A, twice for 2 ml in Group B, and three times for 3 ml in Group C) using a constant injection speed of 0.5 ml/s. After evaluating the cephalocaudal and AP spread in the epidural space on the lateral image after 3 ml of contrast medium was injected, the fluoroscope was switched to the AP image. In the AP image, the ipsilateral and contralateral contrast medium spreads were evaluated. Paravertebral and intercostal spreads were excluded from this study. After confirming the spread in the AP image, 3 ml of a mixture of 1 ml dexamethasone (5 mg/ml) and 2 ml 0.5% lidocaine was injected for pain reduction.
1. Data analysis
Radiologic charts were reviewed by a physician who did not conduct the procedure. Epidurography was used to analyze the degree of contrast medium spread and patterns under the following parameters: 1) anterior or posterior epidural spread on the lateral image; 2) cephalad and caudal spread from the injection site on the lateral image; and 3) ipsilateral or contralateral spread on the AP image.
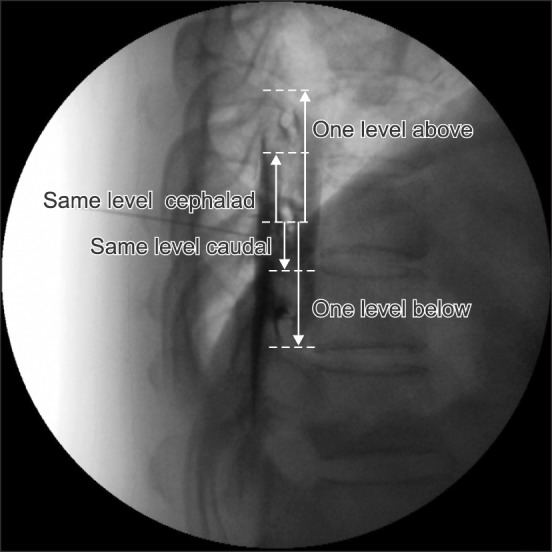
On the lateral image, anterior epidural spread was defined as contrast medium spread extending in an anterior direction for a distance of one-third of the epidural space. The extent of contrast medium spread was determined depending on whether it included the intervertebral foramen or not. If the contrast reached the lower endplate of one vertebral body, it would be recorded as one level below when it was counted in the cephalad direction. If the contrast medium reached the upper endplate of one vertebral body, it would be recorded as that level, when it was counted in the cephalad direction. If the contrast medium reached the upper endplate of one vertebral body, it would be recorded as one level above when it was counted in the caudal direction. If the contrast medium reached the lower endplate of one vertebral body, it would be recorded as that level when it was counted in the caudal direction (
Fig. 1) [
3].
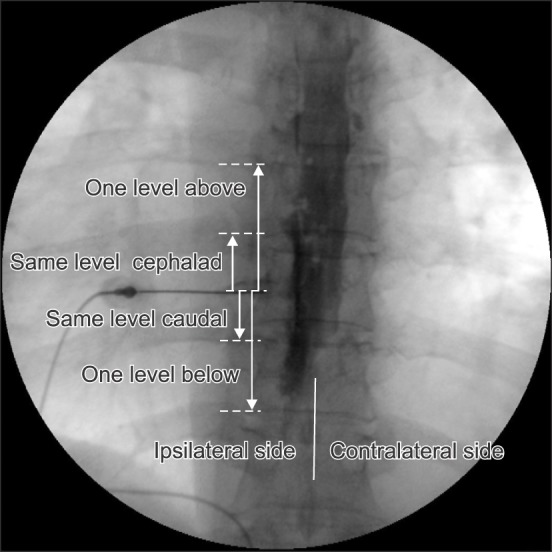
In analyzing the spread of contrast medium on the AP image, the contralateral side was defined as the opposite side from which the procedure was conducted. Ipsilateral or contralateral spread on the AP image was defined as the contrast medium spreading across the spinous process and was defined as one-side spread when the contrast spread only within the spinous process. Contrast spread on the AP image was calculated the same as on the lateral image, and ipsilateral contrast medium spread was compared with contralateral spread (
Fig. 2).
2. Statistics
There was no previous study utilizing the same methodology. Therefore, this study was designed as an exploratory investigation, and a power analysis was not performed. The target number of patients completing the study was 20; considering a 20% dropout rate, 26 patients were enrolled in this study.
Values for age, height, weight, and duration of symptoms before admission to our clinic are presented as mean ± standard deviation. Values associated with the spread level of contrast medium are reported as median (interquartile range). Contrast spreads were analyzed using the Friedman test with repeated measurements among the groups, and the Wilcoxon signed-rank test was used for post hoc analysis. In further analysis of the data, all patients were divided into three groups, including the upper (T1−T4), middle (T5−T8) and lower thoracic group (T9−12). Contrast medium spread in the lateral image was analyzed using the Kruskal-Wallis test among these groups and the Mann-Whitney test was used for post hoc analysis. IBM SPSS 18.0 statistical software (IBM, Chicago, IL) was used for statistical analysis.
A P value < 0.05 with Bonferroni's correction was considered significant. The Wilcoxon signed-rank test was adopted for comparison of values within the groups, and a P value < 0.05 was considered significant.
RESULTS
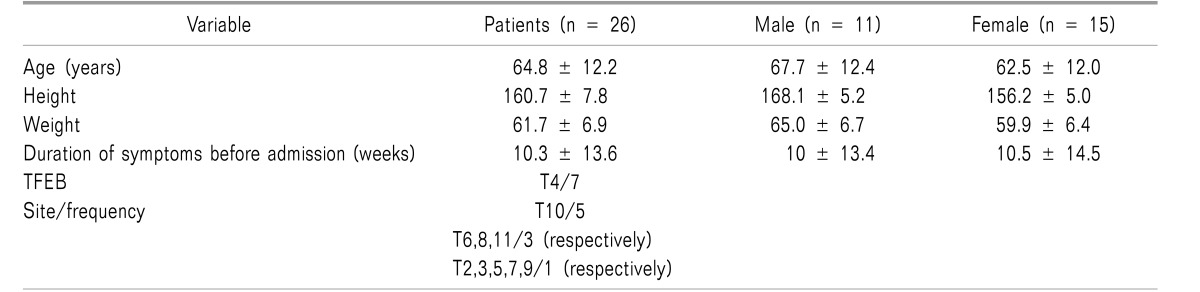
A total of 26 patients with herpes zoster or PHN were enrolled in this study; 11 patients were male, and 15 patients were female. The average age was 64.8 ± 12.2 years. Average duration of symptoms before admission was 10.3 ± 13.6 weeks. Other demographic data and the site and frequency of TTFEB performed are presented in
Table 1.
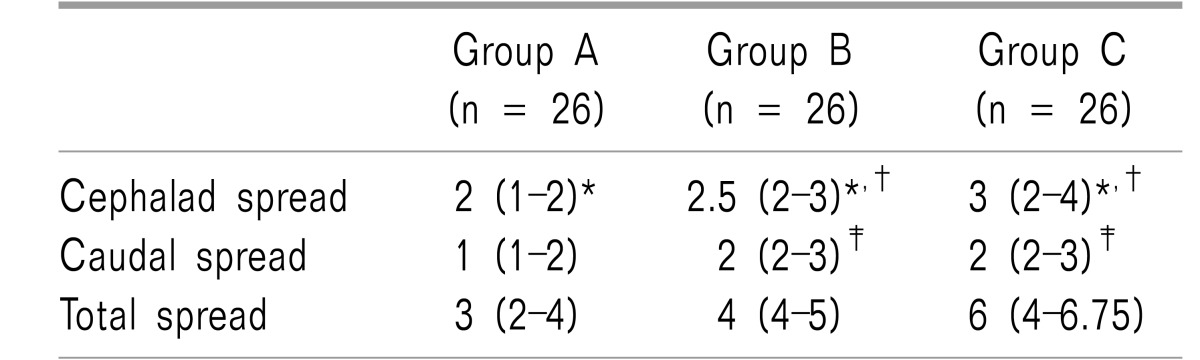
The cephalad spread level of contrast medium expressed as median (interquartile range) on the lateral image was 2.00 (1.00–2.00) for Group A, 2.50 (2.00–3.00) for Group B, and 3.00 (2.00–4.00) for Group C. There were significant differences in the cephalad spread of contrast agent between Groups A and B, Groups B and C, and Groups A and C (
P < 0.001 for all) (
Table 2). The caudal spread level of contrast medium was 1.00 (1.00–2.00) for Group A, 2.00 (2.00–3.00) for Group B, and 2.00 (2.00–3.00) for Group C. There were significant differences in caudal spread of contrast medium between Groups A and B, B and C, and A and C (
P < 0.001 for all) (
Table 2).
In all groups, the spread of contrast due was wider in the cephalad direction than in the caudal direction (
P < 0.05 for Group A,
P < 0.01 for Group B, and
P < 0.01 for Group C). The total spread was 3.00 (2.00–4.00) for Group A, 4.00 (4.00–5.00) for Group B, and 6.00 (4.00–6.75) for Group C (
Table 2).
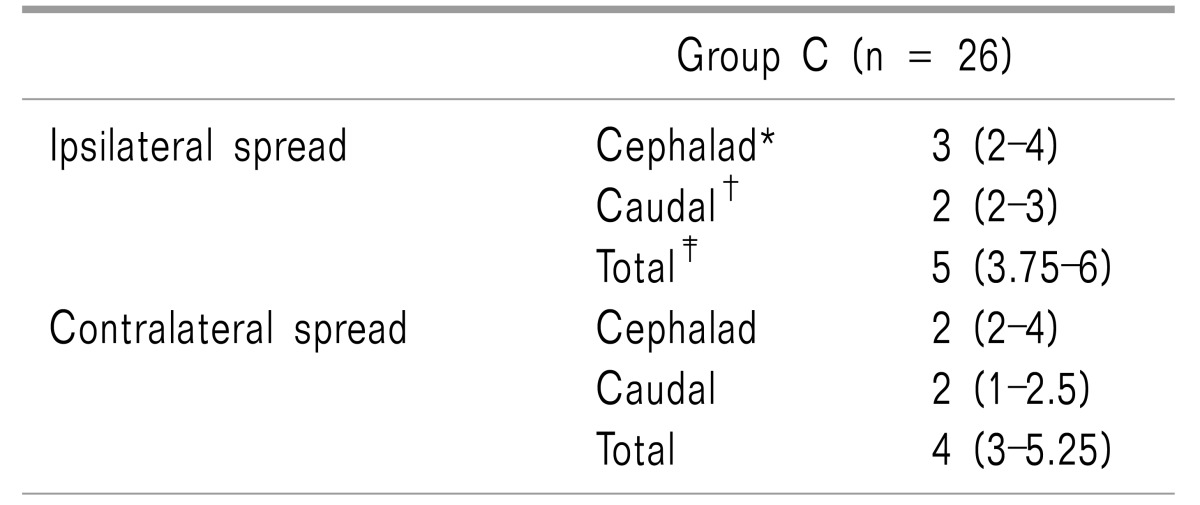
Both ventral and dorsal spread of the 3 ml contrast medium injection was revealed in 88% (23/26) of cases. Either ventral-only or dorsal-only spread after a 3 ml contrast medium injection was shown in 12% (3/26) of cases. Bilateral (ipsilateral and contralateral) epidural spread of contrast medium on the AP image was exhibited in 85% (22/26) of cases after the 3 ml contrast medium injection. The remaining 4 cases (15%) showed unilateral spread on the ipsilateral side.
After the 3 ml injection of contrast medium, the ipsilateral spread level was wider than the spread on the contralateral side in all directions (cephalad,
P < 0.05; caudal direction,
P <0.01; and total spread,
P < 0.001) (
Table 3).
For further analysis, all patients were divided according to the site of their TTFEB, conducted according to the described method. Of the nine patients included in the upper thoracic group, eight were in the middle and nine were in the lower thoracic groups. There was no difference in sex frequency, age, weight and height among the groups.
The results were that the spread level to the cephalad or caudal direction after 1, 2, and 3 ml injections of contrast medium showed no difference between the upper, middle, and lower thoracic groups, respectively (P > 0.05). There was no significant difference in total spread among the groups either.
The total spread level, expressed by a median (interquartile range) of 1 ml of contrast medium injected, were 3.00 (2.00–3.50) in the upper thoracic group, 3.00 (2.25–4.00) in the middle thoracic group, and 3.00 (2.00–3.00) in the lower thoracic group. The total spread level of 2 ml of contrast medium, were 5.00 (4.00–5.50) in the upper thoracic group, 4.50 (4.00–5.00) in the middle thoracic group, and 4.00 (3.00–5.00) in the lower thoracic group. The total spread level of 3 ml of contrast medium, were 6.00 (4.50–7.50) in the upper thoracic group, 5.50 (4.25–7.75) in the middle thoracic group, and 6.00 (4.00–6.00) in the lower thoracic group.
DISCUSSION
TTFEB is commonly used in pain clinics for the treatment of herpes zoster or PHN. Twenty-six patients with herpes zoster or PHN were enrolled in this study. This study analyzed the spread of contrast medium following injections of 1, 2, and 3 ml contrast in TTFEB on the AP and lateral images. Cephalad and caudal spreads were significantly different according to the injection volume on the lateral image, and there was a larger spread in the cephalad direction than in the caudal direction. There was bilateral spread of 3 ml injections of contrast medium in 85% of cases in the AP image, but there was a significant difference in spread levels between the ipsilateral and contralateral sides in the cephalad direction, caudal direction, and total spread.
In this study, contrast medium spread in the cephalad direction was wider than in the caudal direction on the lateral view in all three groups (
Table 2). This contrast medium spread pattern is similar in the thoracic interlaminar epidural block (TIEB) [
5], and in other studies of the lumbar area [
6]. A greater tendency toward cephalad spread than caudal spread may be common in epidural procedures.
Yokoyama et al. [
6] reported that the spread of contrast medium in the epidural space correlated with sensory blocks. Therefore, we suggest that a sensory block after a local anesthetic injection combined with a steroid may reveal similar results.
In rabbits, there is a linear correlation between contrast medium volume and its spread in the epidural space. Contrast medium spread showed even distribution to the rostral and caudal direction at the T7 site, but it spread rostally twice as far as caudally at the T12 site [
7]. Visser et al. [
8] described an extension of sensory blockade after 60 mg lidocaine epidural administration at high (C7−T1 or T1−T2), mid (T3−T4 or T4−T5), and low thoracic level (T7−T8 or T8−T9). In our study, we analyzed the difference in the contrast medium spread level between the upper, middle, and lower thoracic groups (n = 9/8/9, respectively). The results showed no difference in the cephalad, caudal and total spread of 1 ml, 2 ml, and 3 ml of contrast medium, respectively, among the groups. We guessed that results were due to the small numbers of patients in the divided groups, and it was difficult to generalize due to the small number of patients in each group.
Our study protocol called for a total of 3 ml of contrast medium to be divided into 1-ml injections for each patient. One study examined sensory blocks between four groups which were divided into a single 5 ml epidural mepivacaine injection, a single 10 ml injection, two 5 ml injections with a 5-minute interval, and two 5 ml injections with a 10-minute interval. The results revealed that the segment of sensory block between the 10 ml single injection and the two 5 ml injections with a 5-minute interval showed no statistical difference [
9]. Therefore, three 1 ml injections totaling a volume of 3 ml at 5 s intervals may spread in a similar pattern to a single 3-ml injection.
Furman et al. [
10] described medium spread on the contralateral side for 0.5 to 3 ml contrast volumes in lumbar transforaminal epidural block procedures. Their study revealed that contrast crossover cumulated 67% to 90% according to the volume of contrast medium from 1 ml to 3 ml. Kim et al. [
11] described lumbar transforaminal block selectivity. That study conducted that 2 ml of contrast medium mixed with 1 ml of saline was injected through the lumbar transforaminally from L1 to L5. Bilateral contrast medium spread revealed around 28.2% (n = 37/131). However, differences in contrast spread level between the ipsilateral and contralateral sides were not described. We checked bilateral spread in the AP image only after an injection of 3 ml contrast medium in TTFEB. Bilateral spread was observed in 85% of 26 cases after injection of 3 ml of contrast medium; in cases of bilateral spread, there were significant differences in spread levels between the ipsilateral and contralateral sides.
Thoracic and lumbar epidural anatomy is different. The dura mater in the lumbar spine is an adherent vertebral bony canal, and it contributes segmented and discontinued epidural space. In contrast, the dura in the thoracic spine reveal less adherent to the vertebral bony canal [
12]. The thoracic vertebral canal is rounder and smaller than in the cervical and lumbar region. The superior-inferior height of the thoracic vertebra is greater than the anterior-posterior length in T1 and T2, but this ratio is reversed in the rest of the thoracic vertebra [
12]. Meanwhile, in cryo-microtome, there is no dorsomedial fold or fibrous tissue but dorsomedial fat tissue may occur resistant to the spread of contrast medium or local anesthetics though the foramen. The thoracic epidural space contains less fat tissue than the lumbar area [
13].
We suggested less fat tissue in the thoracic epidural space resulted in less resistance to the spread of contrast medium. This made it easy for the bilateral contrast spread in our study. Meanwhile, according with increased age, the amount of epidural fat tissue decreases. This made the epidural space wider [
14] and more compliant, less resistant [
15]. The mean age of the enrolled patients in this study was 64.8 ± 12.2 (mean ± SD). Therefore, the property of the spread patterns at a young age were not reflect in this study.
Goel and Pollan [
16] described that the incidence of ventral spread in the cervical epidural block with contrast medium of 2, 3, or 4 ml was 44.6%. Another study conducted at the lumbar spine using 5 ml contrast medium mixed with a steroid, using the interlaminar approach, revealed an incidence of 43–51% of ventral contrast medium spreading according to needle location to spinal process [
17]. In herpes zoster, segmental zoster paresis (pseudohernia) in the abdominal wall may cause the virus to invade the anterior horn cells or anterior spinal nerve roots [
18]. The delivery of steroids close to the dorsal root ganglion would be expected to reduce inflammation [
19]. Ventral spread may contribute to reduce inflammation of involved segmental nerves. In our study, we observed ventral spread of 3 ml contrast medium in 96% (25/26) of cases.
Purcell-Jones et al. [
20] described paravertebral contrast medium spread of 5 ml mixed with local anesthetics. Paravertebral spread was only 18% (n = 8/45) and mean segmental sensory loss was 1.43. Paravertebral and some epidural spread was 27% (n = 12/45) and mean segmental sensory loss was 2.27. The other study described that similarly, paravertebral injection with 1.5 mg/kg of bupivacaine 0.5% produced sensory loss at the level of the injection with a mean superior spread of 1.4 dermatomes and a mean inferior spread of 2.8 dermatomes [
21]. Multiple injections of the paravertebral block reduced acute pain and prevented PHN significantly [
22].
Meanwhile, the transforaminal epidural block in the thoracolumbar area increased risk of trauma to the Adamkiewicz artery leading to paraplegia [
23]. The Adamkiewicz artery is located mainly on the left side (83%) and was found between T8 and L1 93% of the time. TIEB is accompanied by risks of dural puncture and neurologic injury [
24]. In the middle thoracic levels, the spinous processes are aligned more steeply, rendering TIEB difficult [
13]. For this, pain physicians choose TIEB or TTFEB in terms of risk and technical skill.
In analysis of this study, contrast enhancement revealed clearly in the AP and lateral view images in the fluoroscopic monitor, but showed slightly more blurred images in the AP than lateral image through picture archiving and communication systems (PACs) at review after the procedure, and we analyzed the results divided into the ipsilateral and contralateral side at AP images. We theorized these reasons was that the median total spread level differed between the AP and lateral views after injection of 3 ml of contrast medium.
This study has several limitations. First, the subject of the enrolled patients was variable according to the site of the TTFEB. Second, the middle and lower thoracic spread pattern may be expected to be different due to thoracic kyphosis and vertebral height according to levels, but the numbers of enrolled patients were not enough to reflect the two points. Third, spread range may reveal differences between young and old-aged group but this study did not include a young age group. These factors limit the results of this study in a generalized way. Fourth, this study did not investigate the correlation between contrast medium spreading pattern and the effectiveness of the drug injected, therefore, it was not necessary to enroll patients limited to herpes zoster and PHN.
In conclusion, contrast medium spread in the thoracic transforaminal epidural block is sufficient to cover 3 levels in the cephalad direction and 2 levels in the caudal direction from the site at which the procedure was performed. Furthermore, high percentages of cases exhibited concurrent dorsal and ventral spread, and concurrent ipsilateral and contralateral spread. Further study is needed for generalized results for the TTFEB.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download