Abstract
We report a case of fluoroscopy-guided intraarticular steroid injection for sternoclavicular joint (SCJ) arthritis caused by limited cutaneous systemic sclerosis (SSc). A 50-year-old woman diagnosed with limited cutaneous SSc presented with swelling and pain in the right SCJ. MRI revealed signs of inflammation consistent with right-sided sternoclavicular joint arthritis. After the failure of oral medications, we performed fluoroscopy-guided injection in this region. She reported complete resolution of her symptoms at 4 and 12-week follow-ups. This outcome suggests that a fluoroscopy-guided SCJ injection might be a safe and successful treatment option for sternoclavicular joint arthritis.
Go to : 
Systemic sclerosis (SSc) is a connective tissue disorder characterized by internal organ involvement, dermal thickening and fibrosis. SSc is categorized into two groups: limited cutaneous (LcSSc) and diffuse cutaneous (DcSSc) forms. The former (the CREST syndrome) is characterized by calcinosis, Raynaud's phenomenon, sclerodactyly, esophageal dysmotility, and telangiectasia [1]. Although joint involvement is not so common in LcSSc, arthritis is reported to occur at a rate of 15% [23]. Hand joints are usually affected, followed by wrist, elbow, and knee joints. However, the sternoclavicular joint (SCJ) is rarely involved in limited cutaneous SSc, and there is insufficient information about this involvement. The primary treatment of such involvement is conservative, involving nonsteroidal anti-inflammatory drugs, rest, and cold application. In patients unresponsive to conservative treatment, steroid application into the SCJ is another option. Although ultrasonography (US) has been increasingly used for interventional pain management in recent years, other imaging techniques are also used for intra-articular injection [4]. One of these techniques, fluoroscopy-guided SCJ injection has been scarcely covered in the literature [5]. In this report, we present the technique of fluoroscopy-guided intra-articular steroid injection and its outcomes in SCJ arthritis resistant to conservative management in a patient with limited cutaneous SSc.
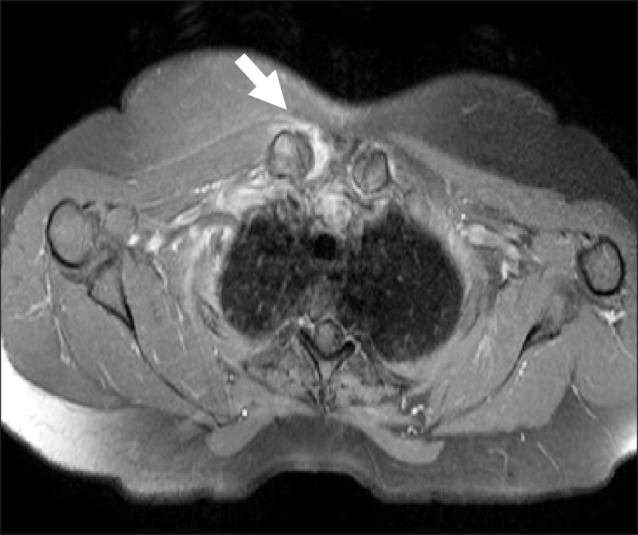
A 50-year-old woman diagnosed with limited cutaneous SSc two years earlier presented to the rheumatology outpatient clinic with swelling and pain on the right side of her neck and the ventral surface of her chest for 3 months. She had been using hydroxychloroquine 200 mg bid, nifedipine 30 mg/day, and acetylsalicylic acid 100 mg/day. Laboratory tests revealed antinuclear antibody 1/1000 +, anticentromere antibody +++, and CRP: 9,49 mg/dl, while other parameters were normal. MRI revealed signs of inflammation consistent with right-sided sternoclavicular joint arthritis (Fig. 1). Diagnosed with scleroderma-associated sternoclavicular joint arthritis, the patient was started on prednisolone 10 mg/day. Having no satisfactory relief of her pain despite a 10-day trial of medical therapy, the patient was referred to our pain medicine outpatient clinic. On physical examination she had tenderness, swelling, and minimally increased temperature on her right SCJ upon palpation. Her pain was rated 8 on the NRS (Numeric Rating Scale). A fluoroscopy-guided intra-SCJ steroid injection was planned.
After informed written consent was given for the SCJ injection, the patient was placed in a supine position on the fluoroscopy table and monitored. Skin overlying the area of interest was cleansed with povidine iodine and covered with a sterile drape. The right SCJ was palpated and then imaged with the aid of fluoroscopy in the anteroposterior view. Cutaneous and subcutaneous local anesthesia was applied with 1 cc 2% lidocaine. Under fluoroscopic guidance, a 5-cm, 21 G needle was entered into the right SCJ. The contrast material was injected to verify an intra-articular location of the needle (Fig. 2). Then, a mixture of 20 mg methylprednisolone and 0.5 cc bupivacaine 5% was injected. Radiation exposure was 2.25 mGy. The procedure was completed uneventfully. The NRS level was 0 and there was no tenderness in joint palpation at control examinations at the 1st hour, 1st month, and 3rd month.
Go to : 
In this case, steroid injection into SCJ was done under fluoroscopy guidance for SCJ arthritis secondary to limited cutaneous scleroderma. Pain level dropped to a level of NRS 0 at the control examinations at the 1st hour, 1st month, and 3rd month from a preprocedural level of NRS 8, indicating 100% pain relief and improvement in examination findings. No complications occurred during or after the procedure.
There are only a few reports about steroid injection into the SCJ under fluoroscopy guidance. One of these reports is the one reported by Galla et al. [6], in which 40 mg methyl prednisolone and 1 ml bupivacaine were injected into the SCJ under fluoroscopy guidance in a patient with osteitis condensans of the clavicle [6]. That patient experienced an immediate relief of pain following the procedure, and the outcomes of the procedure were consistent with that of our patient, whose pain had regressed to NRS 0 at the 1st hour. That case had some differences from ours, including the lack of reporting of long-term outcomes; using 40 mg methylprednisolone; and applying an SCJ injection for osteitis condensans of the clavicle.
In a retrospective analysis, Peterson et al. [7] explored the 20-30 minute results of the CT-guided injection of triamcinolone 40 mg into a total of 83 SCJs of 50 patients with osteoarthritis or SCJ subluxation. Multiple SCJ injections were repeated at an interval of 1 week to 1 year. Pain relief was immediate in two-thirds of patients. Pain relief was achieved in a short period in a majority of patients, as was the case in our study. That study, however, differs from our study with regard to reporting a CT-guided procedure; including patients with different etiological causes; and providing long-term follow-up data. Our technique has the significant advantage of using a lower radiation dose with fluoroscopy-guided technique compared to the CT-guided technique. Furthermore, taking into account the small size of SCJ and the possible risks of steroid injection, we preferred using a lower steroid dose compared to the cases of Galla et al. [6] and Peterson et al. [7]. In spite of this, the goal of effective treatment in a short time was still reached.
This case is an important contribution to the literature due to its reporting the rare SCj SCJ involvement in a patient with limited cutaneous scleroderma, obtaining an easy access to the target area under fluoroscopy-guidance, showing a lower complication risk, and providing long-term treatment outcomes. However, it also has some limitations, including the lack of reporting long-term treatment outcomes, exposing the patient to radiation unlike the US-guided procedure, and requiring special hardware and equipment unlike the blind procedure. Ultrasound provides the advantages of injection accuracy, reliability, and the ability to perform real-time image-guided procedures [8]. In this case, fluoroscopy-guided injection was preferred, as we had much more experience with fluoroscopy-guided injections than with ultrasound-guided injections.
In conclusion, SCJ arthritis should be considered among the etiological causes of chest pain in patients with limited cutaneous systemic sclerosis. For these patients, intra-SCJ steroid injection is an effective treatment option when pain does not respond to conservative treatment methods. Among injection options, fluoroscopy-guided intra-sternoclavicular joint steroid injection should be regarded as a safe alternative method.
Go to : 
References
1. Merlino G, Germano S, Carlucci S. Surgical management of digital calcinosis in CREST syndrome. Aesthetic Plast Surg. 2013; 37:1214–1219. PMID: 24142114.

2. Velayos EE, Masi AT, Stevens MB, Shulman LE. The 'CREST' syndrome. Comparison with systemic sclerosis (scleroderma). Arch Intern Med. 1979; 139:1240–1244. PMID: 508020.

3. Elhai M, Meunier M, Matucci-Cerinic M, Maurer B, Riemekasten G, Leturcq T, et al. Outcomes of patients with systemic sclerosis-associated polyarthritis and myopathy treated with tocilizumab or abatacept: a EUSTAR observational study. Ann Rheum Dis. 2013; 72:1217–1220. PMID: 23253926.

4. Joines MM, Motamedi K, Seeger LL, DiFiori JP. Musculoskeletal interventional ultrasound. Semin Musculoskelet Radiol. 2007; 11:192–198. PMID: 18095250.

5. Hassett G, Barnsley L. Pain referral from the sternoclavicular joint: a study in normal volunteers. Rheumatology (Oxford). 2001; 40:859–862. PMID: 11511753.

6. Galla R, Basava V, Conermann T, Kabazie AJ. Sternoclavicular steroid injection for treatment of pain in a patient with Osteitis condensans of the clavicle. Pain Physician. 2009; 12:987–990. PMID: 19935983.
7. Peterson CK, Saupe N, Buck F, Pfirrmann CW, Zanetti M, Hodler J. CT-guided sternoclavicular joint injections: description of the procedure, reliability of imaging diagnosis, and short-term patient responses. AJR Am J Roentgenol. 2010; 195:W435–W439. PMID: 21098176.

8. Jeon YH. Easier and safer regional anesthesia and peripheral nerve block under ultrasound guidance. Korean J Pain. 2016; 29:1–2. PMID: 26839663.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download