Abstract
Background
Recently, the use of ultrasound (US) techniques in regional anesthesia and pain medicine has increased significantly. However, the current extent of training in the use of US-guided pain management procedures in Korea remains unknown. The purpose of the present study was to assess the current state of US training provided during Korean Pain Society (KPS) pain fellowship programs through the comparative analysis between training hospitals.
Methods
We conducted an anonymous survey of 51 pain physicians who had completed KPS fellowships in 2017. Items pertained to current US practices and education, as well as the types of techniques and amount of experience with US-guided pain management procedures. Responses were compared based on the tier of the training hospital.
Results
Among the 51 respondents, 14 received training at first- and second-tier hospitals (Group A), while 37 received training at third-tier hospitals (Group B). The mean total duration of pain training during the 1-year fellowship was 7.4 months in Group A and 8.4 months in Group B. Our analysis revealed that 36% and 40% of respondents in Groups A and B received dedicated US training, respectively. Most respondents underwent US training in patient-care settings under the supervision of attending physicians. Cervical root, stellate ganglion, piriformis, and lumbar plexus blocks were more commonly performed by Group B than by Group A (P < 0.05).
Conclusions
Instruction regarding US-guided pain management interventions varied among fellowship training hospitals, highlighting the need for the development of educational standards that mandate a minimum number of US-guided nerve blocks or injections during fellowships in interventional pain management.
Go to : 
Recently, the use of ultrasound (US) during pain management interventions has increased exponentially due to several advantages over other techniques, such as improved safety, portability, cost-effectiveness, and reduced exposure to radiation [1].
US has proven especially useful for differentiating among acute injury, chronic disease, and normal anatomic variations within the musculoskeletal system. Furthermore, US is non-invasive, and can be used to facilitate the delivery of nerve blocks and soft tissue injections. Despite such advantages, US-based interventions are limited by the skill of the operator, which is dependent on proper instruction and sufficient practice/experience. Consequently, recent research has focused on the development of specific educational curricula for specialties in which US is frequently utilized. While a few such studies have focused on the field of pain management [23], no reports have discussed the application of such curricula in Korea.
Therefore, the present study aimed to assess the current state of US training in fellowship programs of the Korean Pain Society (KPS) through comparative analysis between training hospitals.
Go to : 
In February of 2017, we conducted an anonymous survey of 51 pain physicians who had completed a KPS fellowship program. The duration of most fellowship programs was 12 months (11.64 ± 0.77 m). The questionnaire was developed in conjunction with recommendations provided by members of the KPS Committee on US in Pain Medicine. The training hospitals at which KPS fellowships were completed were classified as first-, second-, and third-tier hospitals. This was based on the number of points, which were the sum of the number for outpatients, inpatients, and consulting patients treated annually. As a result, those with fewer than 3,000 points were classified as first-tier, those with from 3,000 to 6,000 points were considered second-tier, and those with more than 6,000 points as third-tier training hospitals. Survey respondents were categorized into two groups, as follows: Group A, graduates of programs conducted at first- and second-tier training hospitals; Group B, graduates of programs conducted at third-tier training hospitals.
The survey consisted of 12 questions regarding current US practices and education during pain management fellowships. Respondents of each group were asked to provide information regarding the type and duration of training in pain management procedures, as well as the presence of US equipment in each pain clinic, methods of US training, techniques, and their overall experience in performing US-guided procedures in pain management settings.
Additional questions regarding fluoroscopy-guided injections were included within the original questions to obtain further information. The rate of US utilization and types of procedures performed in clinical practice for each body part, which was classified based on bodily regions were as follows: cranial, cervical, thoracic, lumbar, or sympathetic/peripheral injection were compared between the two groups. The survey contents are referenced in Appendix 1.
Statistical analyses were performed using SPSS version 17 (SPSS Inc., Chicago, IL, USA). Mean differences were analyzed using independent Samples t-tests and descriptive statistics. Descriptive data are expressed as frequencies and percentages. Categorical data were analyzed using chi-square tests. The level of statistical significance was set at P < 0.05.
Go to : 
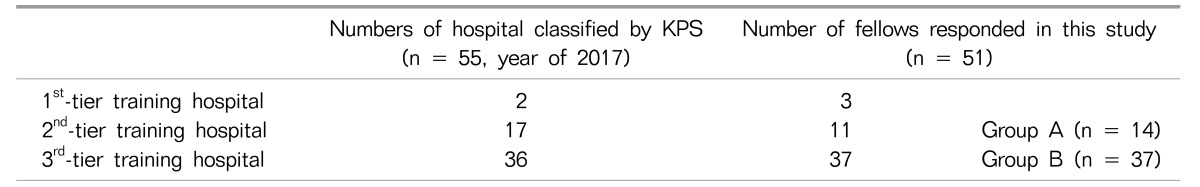
In 2017, there were 55 training hospitals with KPS pain management fellowships: 2 in first-tier hospitals, 17 in second-tier hospitals, and 36 in third-tier hospitals. The number of respondents from the included participants were 3 in first-tier hospitals, 11 in second-tier hospitals, and 37 in third-tier hospitals (Table 1).
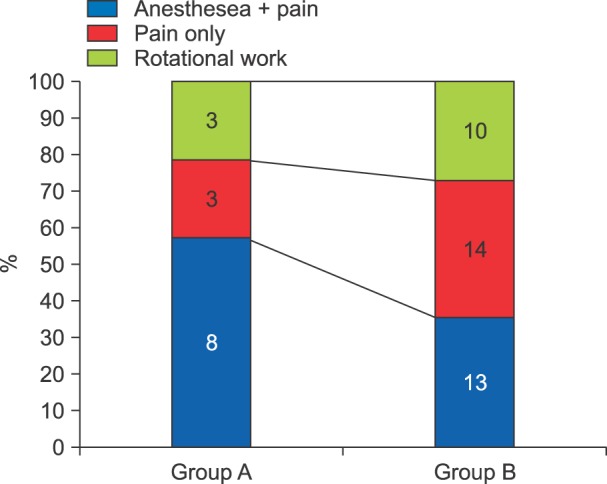
The types of work performed during each pain management fellowship were as follows: In Groups A and B, 21.4% (n = 3) and 37.8% (n = 10) of respondents performed only work associated with pain management via a pain clinic, respectively. Other participants had undergone combined training in anesthesia and pain medicine, or had completed rotations focused on several areas of pain medicine (Fig. 1). All respondents reported that US equipment had been available in their respective pain clinics, with the exception of one respondent in Group B.
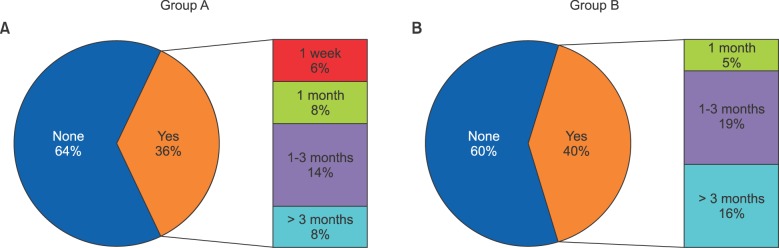
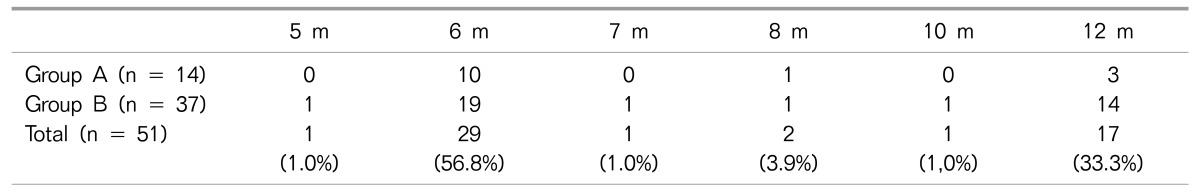
The duration of pain management training during the fellowship program varied from 5 months to 12 months in both groups (Table 2). In Group A, dedicated US training was provided for 36% (n = 5) of respondents, ranging from 1–3 months in 14% (n = 2) of respondents. In Group B, dedicated US training was provided for 40% (n = 15) of respondents, ranging from 1–3 months in 19% (n = 7) and > 3 months in 16% (n = 6) of respondents (Fig. 2).
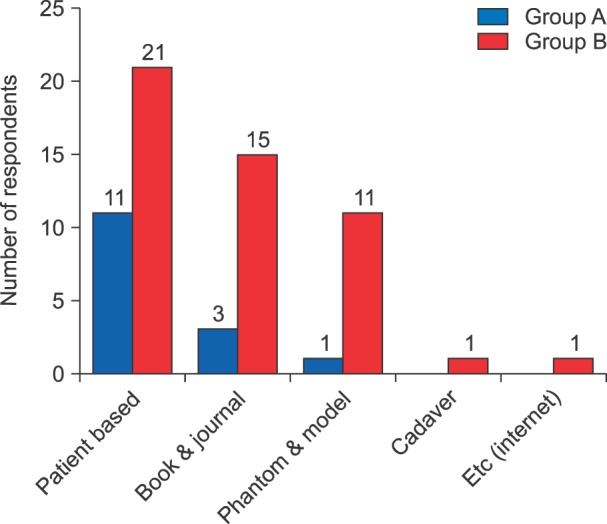
Although training methods varied, no significant differences were observed between the two groups based under the supervision of experienced clinicians (P = 0.150), by the journal or textbook (P = 0.202), and phantom or model-based training (P = 0.080). Additional training methods included cadaver-based training, online assessments, and educational workshops conducted by the KPS (Fig. 3).
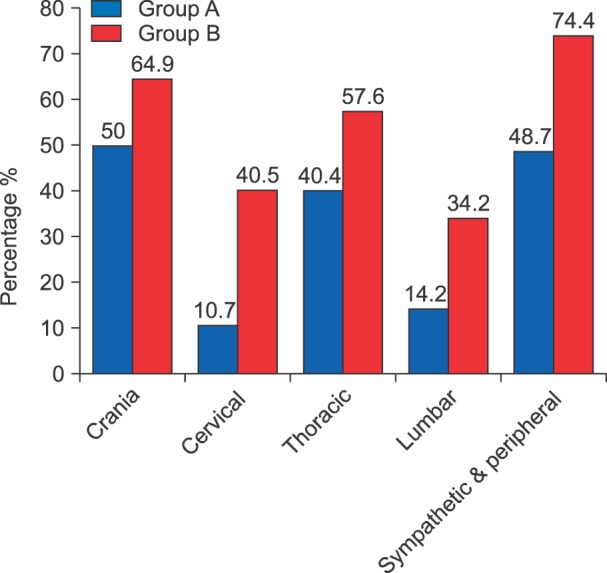
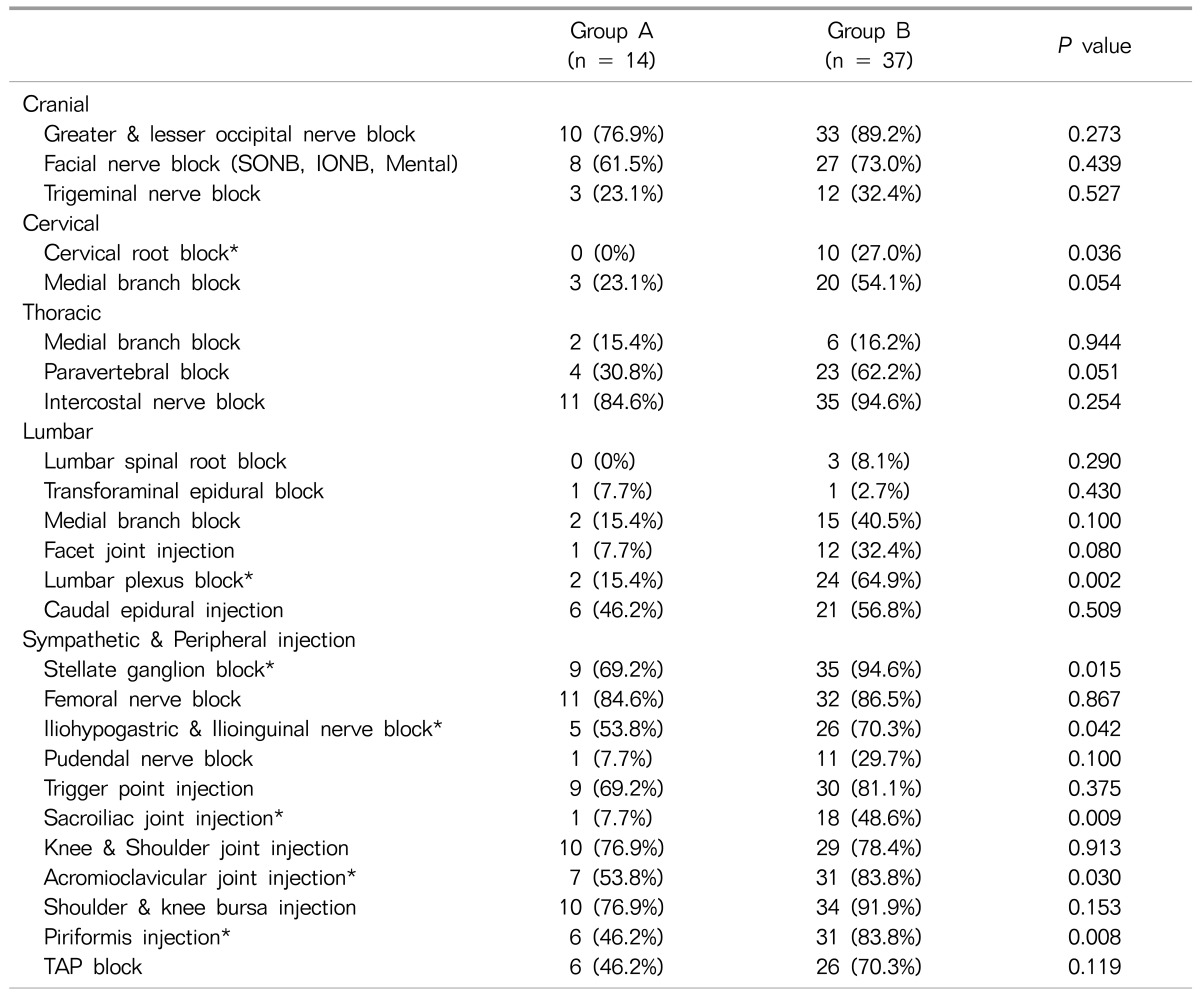
We further analyzed differences in the level of experience with common pain management procedures, which were classified based on bodily regions. The rates of each procedure for each bodily region within each group are presented in Fig. 4 and Table 3. Our results indicated that respondents received the greatest amount of training for cranial and sympathetic/peripheral nerve blocks. In Group A, more than 50% of respondents reported clinical experience was only with cranial procedures, while in Group B respondents had experience with cranial, sympathetic, and peripheral injections. In each procedure, both groups had similar levels of experience with greater and lesser occipital nerve blocks, facial nerve blocks, intercostal nerve blocks, stellate ganglion blocks, femoral nerve blocks, iliohypogastric, and ilioinguinal nerve blocks, trigger point injections, knee and shoulder joint injections, acromioclavicular joint injections, and knee/shoulder bursa injections with more than 50% having clinical experiences.
However, statistically significant differences in the amount of clinical experience were observed between the two groups with regard to the following: cervical root blocks, lumbar plexus blocks, stellate ganglion blocks, iliohypogastric and ilioinguinal nerve blocks, sacroiliac joint injections, acromioclavicular joint injections, and piriformis injections (P < 0.05).
Go to : 
In Korea, pain is regarded as the most common reason for seeking medical treatment, affecting approximately 30% of individuals at some point during their lifetime [4]. However, most patients remain underserved and often fail to obtain adequate relief from pain. Recently, the management of pain using US-guided techniques has increased due to its relative advantages for evaluating structures of the musculoskeletal and nervous system in a timely and cost-effective manner. Indeed, the use of US for interventional techniques continues to increase, especially for procedures involving the axial structure of spine and other peripheral part of the body. Moreover, previous studies have indicated that US guidance for pain management procedures is safer and more effective than guidance based on anatomic landmarks, nerve stimulation, and fluoroscopy [5].
In a meta-analysis of 41 case series and five randomized trials, Bhatia and Brull [6], demonstrated that US is safer for performing injections at the cervical nerve root, cervical sympathetic trunk, suprascapular nerve, and pudendal nerve, when compared with traditional techniques. Moreover, the authors observed that US was effective for performing lumbar nerve root blocks, greater occipital nerve blocks, suprascapular nerve blocks, intercostal nerve blocks, and lateral femoral cutaneous nerve blocks. However, the authors concluded that there is insufficient data to support the efficacy of the technique at present. In a systematic review of randomized controlled trials, Choi and Brull [7] compared US guidance with traditional nerve localization techniques for interventional management of acute pain and pain-related outcomes, reporting that US guidance was not inferior to traditional nerve block techniques for any outcome. However, Choi and Brull [7] concluded that there is insufficient evidence to determine the efficacy of US guidance on acute pain and pain-related outcomes relative to traditional nerve block techniques for interventional pain management.
Although the evidence regarding the use of US in pain management remains controversial, US-guided pain management is an evolving subspecialty in the field of pain medicine. Indeed, several studies support the use of US-guided techniques, as such techniques can decrease the volume of local anesthetics and related side effects, reduce the time required to perform nerve block procedures, and reduce the risk of nerve injury and inadvertent intravascular injection [8910]. Moreover, US-guided techniques allow pain physicians to perform neve blocks or injections on deep structures in patients with obesity or regions affected by degenerative conditions/prior surgery. In addition, US-guided procedures can be performed in patients with relative contraindications for other guidance techniques (e.g., anticoagulant use, which increases the risk of excessive bleeding) under careful monitoring [111213].
However, US is limited by the skill of the operator, the lack of evidence regarding neuraxial procedures, and the steep learning curve required to attain proficiency. Moreover, the resolution of US is limited at deep anatomical structures, particularly in patients with obesity, in whom artifacts may mimic signs of pathological conditions [14]. Thus, both novice pain physicians and those experienced in fluoroscopy will find it necessary to undertake specialized training to acquire proficiency before they can optimally integrate US into their clinical practices.
Interventional pain medicine is evolving as a distinct discipline that requires specialized knowledge and expertise. The introduction of new interventional techniques, such as US guidance, highlights the need for appropriate training in the relevant procedures to ensure both success and patient safety. Although continuing medical educational workshops or conferences may help to facilitate the learning process and skill development, such modalities are often limited in breadth, depth, and training duration. Thus, education regarding US techniques during KPS pain management fellowships is critical.
While residencies or fellowships conducted by anesthesiology and pain medicine departments aim to establish competency pertaining to patient care and pain management procedures, there are currently no core curricula designed to meet the special learning objectives associated with US-guided interventional procedures in Korea. Indeed, our data revealed that US-guided interventions are uncommon during the fellowship period, with the exception of greater and lesser occipital nerve blocks, stellate ganglion blocks, femoral nerve blocks, trigger point injections, and injections of the knee or shoulder joint/bursa. Moreover, less than 50% of respondents in each group reported clinical experience in performing US-guided cervical, thoracic, and lumbar procedures.
As spinal pain represents the most common disease entity in Korea [15], further training regarding spinal procedures should be provided during the fellowship program to ensure appropriate application, and reduce the risk of complications due to operator error. Furthermore, as new US-guided interventional techniques are introduced into clinical practice, fellowship programs should ensure that physicians have been properly trained to implement these techniques safely and effectively. Caudal epidural injections, lumbar plexus blocks, lumbar medial branch blocks, sacroiliac joint injections, and cervical root blocks are an integral part of training as they are a promising part of the interventional techniques for the management of spinal pain, in which US is a capable substitute for fluoroscopy. There is also rapidly growing interest in US as evidenced by the surging number of publications discussing it [14].
The present study possesses some limitations of note. First, data regarding clinical experience with US-guided interventions were only based on subjective responses. While the high response rate decreases the overall bias associated with non-response, some bias may have remained. In addition, we were unable to analyze the accuracy, quality, and proficiency of US training due to limitations associated with the questionnaire design. As future advancements in pain interventions are dependent on the quality of education and training, further studies regarding the status of US education are required [16].
In conclusion, the present study is the first to examine current educational practices associated with US-guided pain management techniques in Korea. It showed the diversity of education and training in US in the management of pain by each hospital. Most of them still showed lack of experiences during the training period. Therefore, our findings highlight the need for the development of educational standards that mandate a minimum number of US-guided nerve blocks or injections during fellowships in interventional pain management. Educational curriculum including a minimum number of procedures and duration of experience with US-guided techniques during the fellowship period, to ensure excellence in independent practice, will increase knowledge of and familiarity with US techniques among fellows. Ongoing surveys for the estimation of educational status by the KPS is also needed.
In both the residency and fellowship programs, training, competency, and proficiency requirements include both didactic and experiential components in US education. Proper understanding of the relevant techniques and application of evidence-based approaches for US-guided pain interventions may improve the overall efficacy of treatment by excellent pain physicians through standardized education.
Go to : 
ACKNOWLEDGEMENTS
This work was carried out by the Committee on Ultrasound in Pain Medicine, 2017 KPS. We would like to express our gratitude to the 2017 KPS fellows for their considerable assistance in this survey.
Go to : 
References
1. Jeon YH. Easier and safer regional anesthesia and peripheral nerve block under ultrasound guidance. Korean J Pain. 2016; 29:1–2. PMID: 26839663.

2. Conway JA, Adhikary SD, Giampetro D, Stolzenberg D. A survey of ultrasound training in US and Canadian chronic pain fellowship programs. Pain Med. 2015; 16:1923–1929. PMID: 26095214.

3. Asaad BO, Reinsel RA, DeVeaux E, Moten H, Durkin B. A survey on teaching ultrasound-guided chronic pain procedures in pain medicine fellowship programs. Pain Physician. 2014; 17:E681–E689. PMID: 25415783.
4. Shin SM. Prevalence and trends of pain associated with chronic diseases and personal out-of-pocket medical expenditures in Korea. Korean J Pain. 2017; 30:142–150. PMID: 28416998.

5. Hopkins PM. Ultrasound guidance as a gold standard in regional anaesthesia. Br J Anaesth. 2007; 98:299–301. PMID: 17307777.

6. Bhatia A, Brull R. Review article: is ultrasound guidance advantageous for interventional pain management? A systematic review of chronic pain outcomes. Anesth Analg. 2013; 117:236–251. PMID: 23592606.

7. Choi S, Brull R. Is ultrasound guidance advantageous for interventional pain management? A review of acute pain outcomes. Anesth Analg. 2011; 113:596–604. PMID: 21642604.

8. Gelfand HJ, Ouanes JP, Lesley MR, Ko PS, Murphy JD, Sumida SM, et al. Analgesic efficacy of ultrasound-guided regional anesthesia: a meta-analysis. J Clin Anesth. 2011; 23:90–96. PMID: 21377070.

9. Chin KJ, Chan V. Ultrasound-guided peripheral nerve blockade. Curr Opin Anaesthesiol. 2008; 21:624–631. PMID: 18784490.

10. Abrahams MS, Aziz MF, Fu RF, Horn JL. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2009; 102:408–417. PMID: 19174373.

11. Sites BD, Beach ML, Chinn CD, Redborg KE, Gallagher JD. A comparison of sensory and motor loss after a femoral nerve block conducted with ultrasound versus ultrasound and nerve stimulation. Reg Anesth Pain Med. 2009; 34:508–513. PMID: 19920428.

12. Assmann N, McCartney CJ, Tumber PS, Chan VW. Ultrasound guidance for brachial plexus localization and catheter insertion after complete forearm amputation. Reg Anesth Pain Med. 2007; 32:93.

13. Ferraro LH, Tardelli MA, Yamashita AM, Cardone JD, Kishi JM. Ultrasound-guided femoral and sciatic nerve blocks in an anticoagulated patient. Case reports. Rev Bras Anestesiol. 2010; 60:422–428. PMID: 20659615.

14. Narouze SN. Ultrasound-guided interventional procedures in pain management: evidence-based medicine. Reg Anesth Pain Med. 2010; 35:S55–S58. PMID: 20216026.
15. Kim YD, Moon HS. Review of medical dispute cases in the pain management in Korea: a medical malpractice liability insurance database study. Korean J Pain. 2015; 28:254–264. PMID: 26495080.

16. Smith HM, Kopp SL, Jacob AK, Torsher LC, Hebl JR. Designing and implementing a comprehensive learner-centered regional anesthesia curriculum. Reg Anesth Pain Med. 2009; 34:88–94. PMID: 19282705.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download