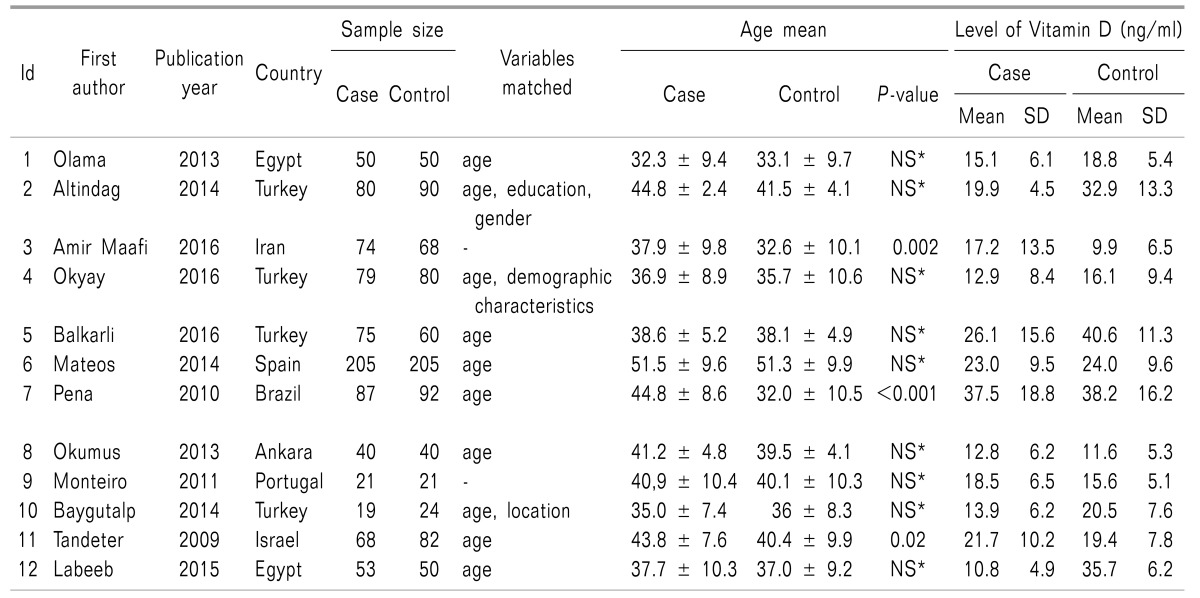
1. Olama SM, Senna MK, Elarman MM, Elhawary G. Serum vitamin D level and bone mineral density in premenopausal Egyptian women with fibromyalgia. Rheumatol Int. 2013; 33:185–192. PMID:
22311432.

2. Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American college of rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum. 1990; 33:160–172. PMID:
2306288.

3. Okyay R, Koçyigit B, Gürsoy S. Vitamin D levels in women with fibromyalgia and relationship between pain, tender point count and disease activity. Acta Med Mediterr. 2016; 32:243–247.
4. Labeeb AA, Al-Sharaki DR. Detection of serum 25(OH)-vitamin D level in the serum of women with fibromyalgia syndrome and its relation to pain severity. Egypt Rheumatol Rehabil. 2015; 42:196–200.

5. Baygutalp NK, Baygutalp F, Şeferoğlu B, Bakan E. The relation between serum vitamin D levels and clinical findings of fibromyalgia syndrome. Dicle Med J. 2014; 41:446–450.

6. Abokrysha NT. Vitamin D deficiency in women with fibromyalgia in Saudi Arabia. Pain Med. 2012; 13:452–458. PMID:
22221390.

7. Abeles AM, Pillinger MH, Solitar BM, Abeles M. Narrative review: the pathophysiology of fibromyalgia. Ann Intern Med. 2007; 146:726–734. PMID:
17502633.

8. Wood PB, Holman AJ, Jones KD. Novel pharmacotherapy for fibromyalgia. Expert Opin Investig Drugs. 2007; 16:829–841.

9. Bergman S. Management of musculoskeletal pain. Best Pract Res Clin Rheumatol. 2007; 21:153–166. PMID:
17350550.

10. Arnold LM, Clauw DJ, Dunegan LJ, Turk DC. FibroCollaborative. A framework for fibromyalgia management for primary care providers. Mayo Clin Proc. 2012; 87:488–496. PMID:
22560527.

11. Bhatty SA, Shaikh NA, Irfan M, Kashif SM, Vaswani AS, Sumbhai A, et al. Vitamin D deficiency in fibromyalgia. J Pak Med Assoc. 2010; 60:949–951. PMID:
21375201.
12. Atherton K, Berry DJ, Parsons T, Macfarlane GJ, Power C, Hyppönen E. Vitamin D and chronic widespread pain in a white middle-aged British population: evidence from a cross-sectional population survey. Ann Rheum Dis. 2009; 68:817–822. PMID:
18697776.

13. Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. 2003; 78:1463–1470. PMID:
14661675.

14. Altindag O, Ögüt E, Gur A, Gursoy S, Gunay M. Serum vitamin D level and its relation with clinical parameters in fibromyalgia as a neuropathic pain. Orthop Muscular Syst. 2014; 3:171.

15. Ulusoy H, Sarica N, Arslan S, Ozyurt H, Cetin I, Birgul Ozer E, et al. Serum vitamin D status and bone mineral density in fibromyalgia. Bratisl Lek Listy. 2010; 111:604–609. PMID:
21384747.
16. Okumus M, Koybası M, Tuncay F, Ceceli E, Ayhan F, Yorgancioglu R, et al. Fibromyalgia syndrome: is it related to vitamin D deficiency in premenopausal female patients? Pain Manag Nurs. 2013; 14:e156–e163. PMID:
24315268.

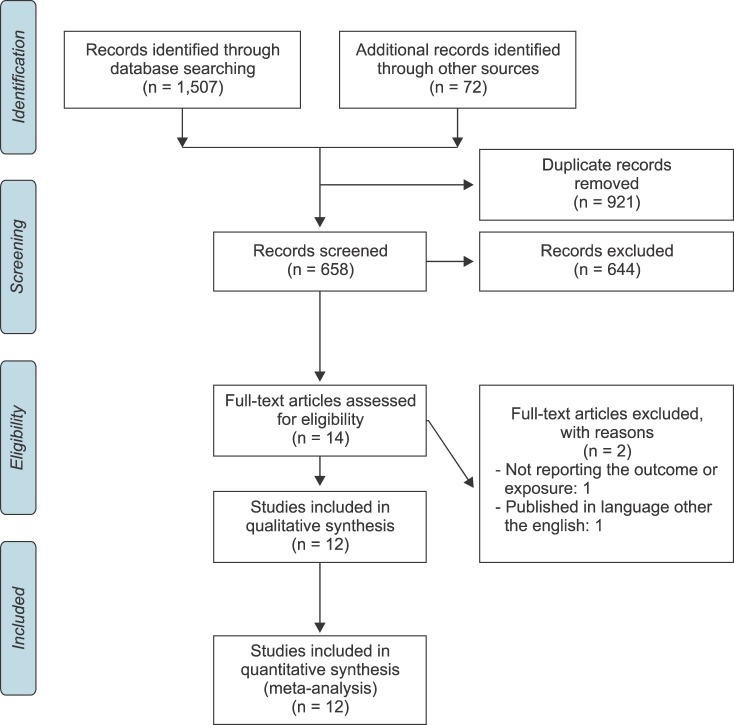
17. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009; 62:1006–1012. PMID:
19631508.

18. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID:
843571.

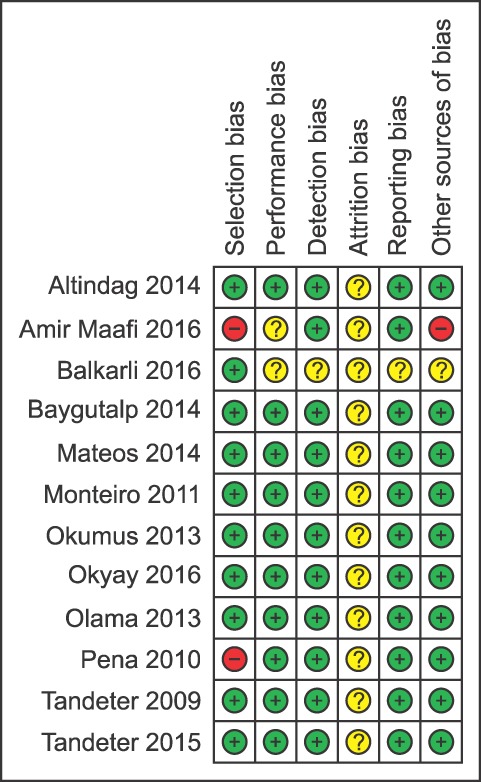
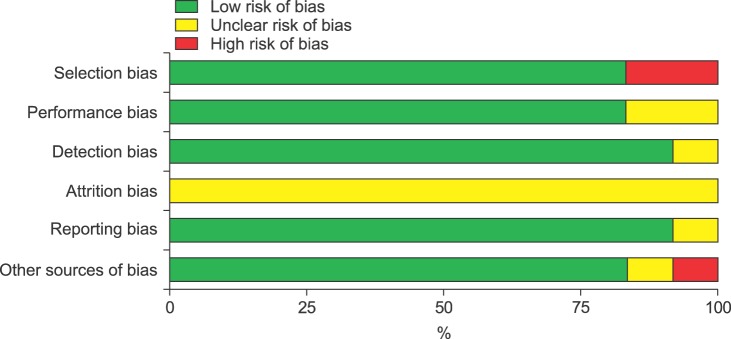
19. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [Internet]. London: The Cochrane Collaboration;2011. cited 2011 March 3. Available at
http://handbook.cochrane.org.
20. Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters M, et al. Assessing the risk of bias of individual studies in systematic reviews of health care interventions [Internet]. Rockville (MD): Agency for Healthcare Research and Quality;2012. cited 2012 March 8. Available at
https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0077771/.
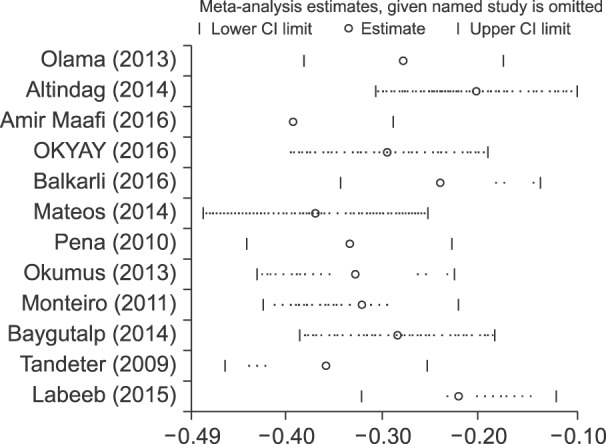
21. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21:1539–1558. PMID:
12111919.

22. Al-Allaf AW, Mole PA, Paterson CR, Pullar T. Bone health in patients with fibromyalgia. Rheumatology (Oxford). 2003; 42:1202–1206. PMID:
12810939.

23. Maafi AA, Ghavidel-Parsa B, Haghdoost A, Aarabi Y, Hajiabbasi A, Shenavar Masooleh I, et al. Serum vitamin D status in Iranian fibromyalgia patients: according to the symptom severity and illness invalidation. Korean J Pain. 2016; 29:172–178. PMID:
27413482.

24. Balkarli A, Balkarlı H, Temel S, Ozhan N, Ozkan U, Cobankara V. AB0656 Serum vitamin D and parathyroid hormone levels in premenopausal women with fibromyalgia syndrome. Ann Rheum Dis. 2013; 72:A989.
25. Mateos F, Valero C, Olmos JM, Casanueva B, Castillo J, Martínez J, et al. Bone mass and vitamin D levels in women with a diagnosis of fibromyalgia. Osteoporos Int. 2014; 25:525–533. PMID:
24008400.

26. Monteiro DM. Evaluation of vitamin D status in a population with fibromyalgia [master thesis]. Coimbra: Univ. of Coimbra;2011.
27. Özcan DS, Öken Ö, Aras M, Köseoğlu BF. Vitamin D levels in women with fibromyalgia and relationship between pain, depression, and sleep. Turk J Phys Med Rehabil. 2014; 60:329–334.

28. de Rezende Pena C, Grillo LP, das Chagas Medeiros MM. Evaluation of 25-hydroxyvitamin D serum levels in patients with fibromyalgia. J Clin Rheumatol. 2010; 16:365–369. PMID:
21085020.

29. Tandeter H, Grynbaum M, Zuili I, Shany S, Shvartzman P. Serum 25-OH vitamin D levels in patients with fibromyalgia. Isr Med Assoc J. 2009; 11:339–342. PMID:
19697583.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download