LETTERS TO EDITOR
Syringomyelia is the term used to indicate a glial-line cavity in the parenchymal spinal cord without involvement of the cord's central canal. Characterized by an intraspinal cavity, it may cause central neuropathic pain with various adverse symptoms [123].
The patient was a 50-year-old woman with a history of severe congenital syringomyelia, whose syrinx extended from the thoracic to the sacral region. There was a marked increase in the size of the syrinx cavity, mainly 4.78-3.88 cm as AP-Lateral at the diameter of the L1 level and 4.56-4.31 cm as AP-Lateral at the diameter of the L3 level (Fig. 1). She had severe neuropathic pain and sensory loss extending from the trunk to the bilateral lower extremities. Other symptoms include bowel and bladder incontinence. She had received 4 times operations, the last operation being two years ago. The clinical effects after these surgeries was that the patient worsened. The patient complained of progressive coxalgia, lower back pain, motor weakness, muscle atrophy in both lower extremities, numbness, and pain. Prior to consideration of SCS (spinal cord stimulation), the patient regularly used paracetamol (Parol 500 mg tablet, Atabey Pharma, Turkey) at 2 g/day, a fentanyl patch (Duragesic 100 µg/TTS, Janssen Pharmaceutica NV, Belgium) at 100 µg/TTS, pregabalin 600 mg/day (Alyse 150 mg tablet, Abdi İbrahim, Turkey), and dexketoprofen trometamol 50 mg/day (Leodex 25 mg tablet, Bilim Pharma, Turkey) at 4 mg/day. On the visual analog scale (VAS), with 0 representing no pain and 10 representing the worst pain imaginable, the patient rated her pain as 8. Her score on the Douleur Neuropathic 4 questionnaire (DN4), meanwhile was 5 under analgesic treatment. The syrinx extended from the thoracic to the sacral region and increased in size at the L1-L3 level. Implantation of SCS electrodes was highly challenging due to the enlarged spinal cord diameter and relatively narrow vertebral canal.
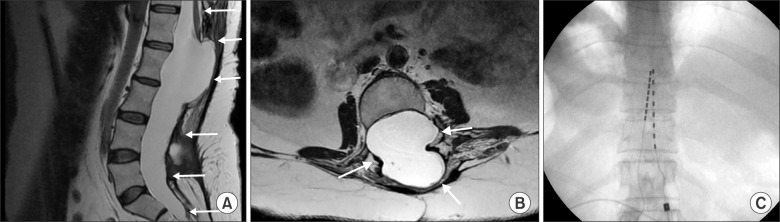 | Fig. 1(A) Sagittal T1- and T2-weighted magnetic resonance imaging (MRI) scan showed syringomyelia in the thoracolumbar region. There is a marked increase in the size of the syrinx cavity, mainly at the L1-L3 level (small arrows). (B) There is a narrow vertebral canal and enlarged spinal cord diameter, as seen in the axial MRI scan. (C) Postoperative X-ray view showing thoracic placement of the epidural percutaneous leads at the T9 and T10 vertebral levels. |
In the operation room, the patient was laid in a prone position, monitored, and given sedoanalgesia. She underwent percutaneous placement of 8-contact leads, both of which were placed in the midline of the epidural space with the distal tip reaching the T9 and T10 vertebral levels (Fig. 1). Both diameters (anterior and lateral) of the spinal canal were fairly wide, which aided the insertion of the SCS electrode (Boston Scientific Corporation, Valencia, CA).
The frequency used was 60 Hz for the left and right electrodes; pulse width varied from 260 to 580 µs and the current ranged from 7.1 to 4.6 mA. During the 15-day trial procedure, the patient reported up to 80% pain relief (VAS = 2, DN4 = 1). Two weeks after the trial, the patient proceeded to permanent SCS implantation. On one- and six-month postoperative follow-up visits, the patient reported continued response to the spinal cord stimulator without any adverse events.
The supposed pain mechanism was spinothalamic tract injury due to the syrinx cavity. In several studies, no correlation has been found between cyst dimension using MRI and clinical symptoms of the syrinx, including the intensity of neuropathic pain. According to some authors, the position of the syrinx, rather than its size, may be better correlated with the clinical findings [34]. The mechanisms behind the efficacy of this method remain unclear [5]. We have successfully treated the patient and based on our case, neuromodulation with SCS has been found to be successful in the treatment of the selected patient with medication-resistant neuropathic pain related to syringomyelia.
Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download