1. Bellingham GA, Peng PW. A low-cost ultrasound phantom of the lumbosacral spine. Reg Anesth Pain Med. 2010; 35:290–293. PMID:
20921841.

2. Eastwood CB, Moore DL. A simple, inexpensive model for the practice of ultrasound-guided regional anesthesia techniques. Reg Anesth Pain Med. 2010; 35:323–324. PMID:
20460978.

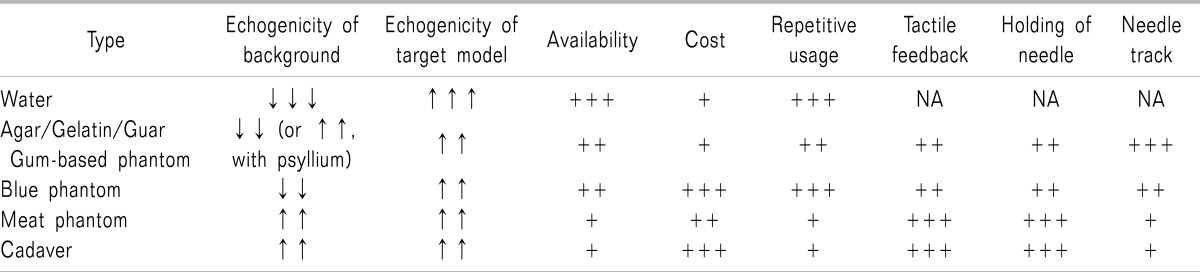
3. Hocking G, Hebard S, Mitchell CH. A review of the benefits and pitfalls of phantoms in ultrasound-guided regional anesthesia. Reg Anesth Pain Med. 2011; 36:162–170. PMID:
21425513.

4. Michalek P, Donaldson W, McAleavey F, Johnston P, Kiska R. Ultrasound imaging of the infraorbital foramen and simulation of the ultrasound-guided infraorbital nerve block using a skull model. Surg Radiol Anat. 2013; 35:319–322. PMID:
23129265.

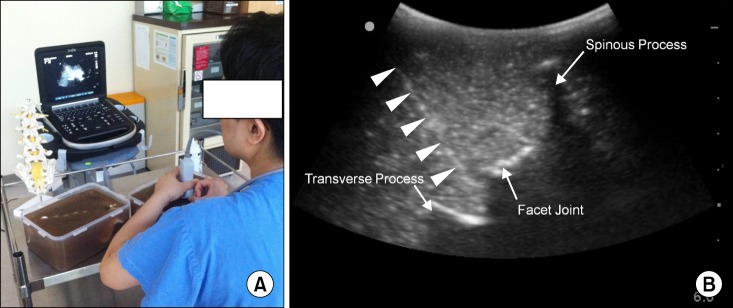
5. Karmakar MK, Li X, Kwok WH, Ho AM, Ngan Kee WD. Sonoanatomy relevant for ultrasound-guided central neuraxial blocks via the paramedian approach in the lumbar region. Br J Radiol. 2012; 85:e262–e269. PMID:
22010025.

6. Gibson RN, Gibson KI. A home-made phantom for learning ultrasound-guided invasive techniques. Australas Radiol. 1995; 39:356–357. PMID:
8561709.

7. Di Domenico S, Santori G, Porcile E, Licausi M, Centanaro M, Valente U. Inexpensive homemade models for ultrasound-guided vein cannulation training. J Clin Anesth. 2007; 19:491–496. PMID:
18063202.

8. Li JW, Karmakar MK, Li X, Kwok WH, Ngan Kee WD. Gelatin-agar lumbosacral spine phantom: a simple model for learning the basic skills required to perform real-time sonographically guided central neuraxial blocks. J Ultrasound Med. 2011; 30:263–272. PMID:
21266566.
9. Brascher AK, Blunk JA, Bauer K, Feldmann R Jr, Benrath J. Comprehensive curriculum for phantom-based training of ultrasound-guided intercostal nerve and stellate ganglion blocks. Pain Med. 2014; 15:1647–1656. PMID:
24506310.

10. Morehouse H, Thaker HP, Persaud C. Addition of Metamucil to gelatin for a realistic breast biopsy phantom. J Ultrasound Med. 2007; 26:1123–1126. PMID:
17646379.

11. Chao SL, Chen KC, Lin LW, Wang TL, Chong CF. Ultrasound phantoms made of gelatin covered with hydrocolloid skin dressing. J Emerg Med. 2013; 45:240–243. PMID:
23399392.

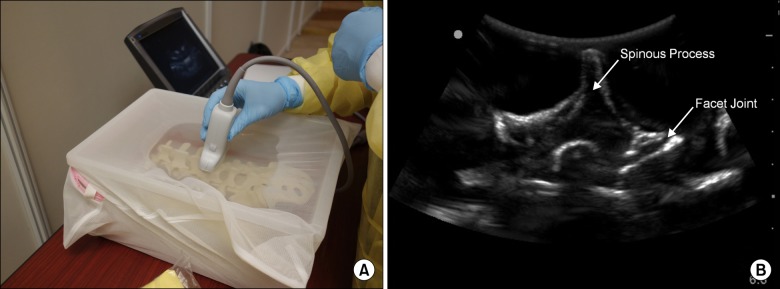
12. Hocking G, McIntyre O. Achieving change in practice by using unembalmed cadavers to teach ultrasound-guided regional anaesthesia. Ultrasound. 2011; 19:31–35.

13. West SJ, Mari JM, Khan A, Wan JH, Zhu W, Koutsakos IG, et al. Development of an ultrasound phantom for spinal injections with 3-dimensional printing. Reg Anesth Pain Med. 2014; 39:429–433. PMID:
25105983.

14. Mendiratta-Lala M, Williams T, de Quadros N, Bonnett J, Mendiratta V. The use of a simulation center to improve resident proficiency in performing ultrasound-guided procedures. Acad Radiol. 2010; 17:535–540. PMID:
20097583.

15. Moore DL, Ding L, Sadhasivam S. Novel real-time feedback and integrated simulation model for teaching and evaluating ultrasound-guided regional anesthesia skills in pediatric anesthesia trainees. Paediatr Anaesth. 2012; 22:847–853. PMID:
22612411.

16. Kwon SY, Hong SH, Kim ES, Park HJ, You Y, Kim YH. The efficacy of lumbosacral spine phantom to improve resident proficiency in performing ultrasound-guided spinal procedure. Pain Med. 2015; 16:2284–2291. PMID:
26234900.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download