Abstract
Sacroiliac (SI) joint pain can result from degeneration, infection, malignancy, and trauma. Patients with metastatic bone pain who do not respond to conventional treatment may need more aggressive neuroinvasive approaches. Recently, pulsed radiofrequency (PRF) neuromodulation has emerged as a promising treatment alternative for refractory cases of SI joint pain. Nevertheless, there is no report on the treatment of pain arising from SI joint metastases with PRF. We are reporting about a 63-year-old woman suffering from buttock pain due to breast cancer metastases in the SI joint. We treated this patient with PRF neuromodulation of the L4-S3 primary dorsal rami and lateral branches using a rotating curved needle technique. The patient tolerated the procedures well, without any complications. She experienced about 70% reduction in pain, and pain relief was sustained for 10 months. This result suggests that PRF neuromodulation is a safe, effective treatment for pain from SI joint metastases.
Go to : 
Pain generated by the sacroiliac (SI) joint is not simply a result of degeneration, but of many other factors, including infection, inflammatory diseases, malignancy, and trauma. Metastatic tumor involvement of the sacrum is far more common than primary sacral lesions, and bone invasion causes pain localized to the sacrum [1]. The conventional therapy for metastatic bone pain requires the use of multidisciplinary therapies, such as radiotherapy along with chemotherapy and analgesic therapy. However, about 20-30% of patients treated with radiotherapy and analgesics may not have optimal pain relief [2]. For these patients who do not respond to conventional treatment, interventional treatments such as pulsed radiofrequency (PRF) neuromodulation may be a useful alternative for alleviating their pain.
Since its first clinical application took place in 1996, PRF was proposed as a safer method of neuromodulation, possibly expanding the indications for clinical use with results equal to conventional radiofrequency (CRF) [3]. Nevertheless, there are still insufficient studies on the efficacy of this method for pain from the SI joint. There is only one study in which patients underwent PRF neuromodulation in SI joint syndrome [4], and no published data on using PRF for metastatic pain in the SI joint.
Therefore, we present a case of PRF neuromodulation of the lumbar dorsal rami and sacral lateral branches in intractable buttock pain originating in sacroiliac metastases.
A 63-year-old female with breast cancer was referred from the Oncology department for the management of pain in both buttocks of 3 months' duration. She had multiple bone and lung metastases, and her pain was rated as 9/10 on an NRS, where 0 represents no pain and 10 corresponds to the worst imaginable pain. Her treatment had included chemotherapy and radiotherapy, and at the time of referral she was using a 25 µg/hr fentanyl patch (Durogesic DTrans®, Janssen Pharmaceutica, Turnhoutseweg, Belgium) with oral medication of pregabalin 300 mg/day, oxycodone 20 mg/day, and amitriptyline 10 mg/day for pain control. The dosage of opioids couldn't be increased because of the side effects such as nausea and vomiting. The pain was characterized as constant, deep aching pain localized in the buttocks, with radiation to the left thigh, and her pain decreased slightly on lying down. Her physical examination revealed marked tenderness over the SI joint and positive Gaenslen's tests, but no motor/sensory change. A bone scan and computed tomography showed metastases in the pelvic bone, spine, femur, and lung (Fig. 1). After SI joint injections, her pain intensity was reduced from 9 to 4 on an NRS, but this improvement was maintained only for 2 days. At this point, we decided to proceed with PRF.
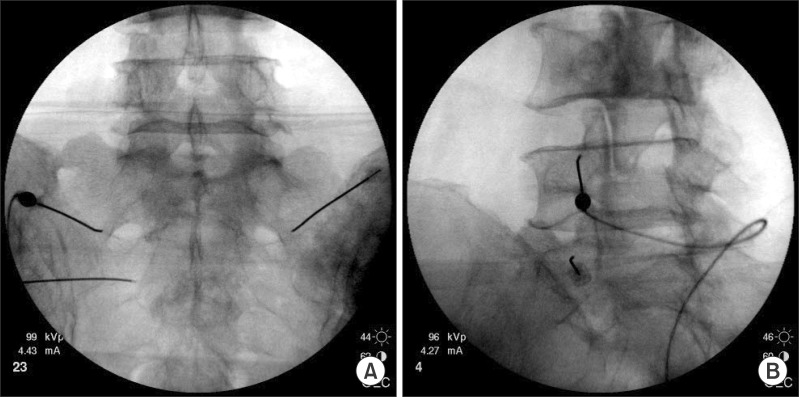
After an informed consent, she underwent PRF neuromodulation of the dorsal rami of L4, L5, and the lateral branches of S1-S3 bilaterally under fluoroscopic guidance. The target locations for the L4-5 dorsal ramus were the notch between the transverse process and superior articular process of L5 and the notch between the ala of the sacrum and the superior articular process of the sacrum. For S1-S3 lateral branch neuromodulation, the cannulas were inserted to the perimeter of the foramen in a semi-circumferential pattern. At the S1 and S2 levels, lesion locations were targeted on the right at the 2:30, 4 o'clock, and 5:30 positions, and on the left at 9:30, 8 o'clock, and 6:30 positions. At the S3 level, lesion locations were targeted on the right at the 2:30 and 4 o'clock positions, and on the left at the 9:30 and 8 o'clock positions. An RFK-C10520S-P cannula (Cosman, Burlington, MA, USA) with 5-mm curved active tips was used at each level; placement of the electrode in close proximity to the nerve was confirmed using electrostimulation at 50 Hz, with concordant sensation achieved at voltage from 0.3 V to 0.5 V. Before lesioning, the absence of leg and sphincter contractions was verified with stimulation at 2 Hz up to 2 V. After confirming correct placement of the needle, two or three PRF lesions were made at each location using a PRF lesion generator (RFG-1A, Cosman, Burlington, MA, USA) (Fig. 2). For S1-S3 lateral branch neuromodulation, after the first cycle was performed, the needle was rotated 180 degrees and a second lesion was made at a target point to increase the area exposed to the electrical field. This procedure was repeated for all lesions at each level. The PRF parameters were 45 V for 120 s. Registered temperatures during the procedure ranged from 39 to 41℃. After the procedure, the patient was transferred to the recovery room and monitored for 30 min. While the NRS was 9 before the procedure, it had decreased to 4 after the procedure. Seven days after the procedure, the NRS had decreased to 2. No complications related to the procedure were observed. The patient experienced about a 70% reduction in pain, and could sit and move after the treatment. She was able to discontinue her use of oxycodone, but continue to take pregabalin, amitriptyline, and use the fentanyl patch. Afterwards, she received repeated chemotherapy in the Oncology department. Bone scans showed no interval change at 5 months and 9 months after PRF neuromodulation. The pain relief was sustained for 10 months until the patient's death from pneumonia.
Go to : 
Sacroiliac joint pain can result from cancer metastases. Analgesia for bone metastatic pain is achieved by blocking a primary nociceptive afferent or by disrupting the nerves carrying the pain input to the central nervous system [5]. Therefore, the treatment of metastatic bone pain might need a more neuroinvasive method in its early stage. There was one reported case using cooled RF in an SI joint metastases [6]. Although the result was excellent, the patient was followed only for a few days.
PRF delivers short bursts of RF current, resulting in considerably lower maximum temperatures compared with continuous mode, and reduces the risk of neighboring tissue destruction [7]. The advantages of PRF compared to conventional RF (CRF) is the absence of any mitochondrial degeneration or structural pathology in cell or nuclear membranes in response to the PRF treatment [8]. Therefore, PRF is minimally invasive, well tolerated, and lacks potential adverse effects associated with high temperatures and can be repeated if pain recurs because minimal tissue has been destroyed. However, lack of randomized controlled trials and known mechanism of action are recognized limitations. One study reported the use of PRF for the treatment of SI joint syndrome [4], and evidence of a good or excellent result was obtained in 73% of the patients. There was one case report on 3 patients that suffered from uncontrolled vertebral metastatic pain and were successfully treated by selective ganglion root PRF [9]. Therefore, we thought that PRF might play an important role for relieving pain from SI joint metastasis.
The positive predictor of a successful outcome for the SI joint is the lesion size [10]. Based on the anatomic variability of the lateral branch nerves, treating a greater volume of tissue lateral to the S1 through S3 sacral foramina is more likely to interrupt targeted sacral lateral branches. Therefore, using small conventional lesions, some of this nociceptive input is likely to be missed. Conventional bipolar RF and cooled RF may be able to create larger lesions compared with conventional RF, so the chance of getting hold of the nerves increases [11]. However, since there are only two studies assessing the effectiveness of conventional bipolar RF, it cannot be said that this method is an effective and reliable treatment option. Although the use of cooled RF was associated with a positive outcome in SI joint pain [12], some complications due to inadvertent lesioning of the sacral spinal nerves may occur. Therefore, we planned PRF neuromodulation with a curved cannula using rotating curved needle technique [13] for increasing the lesion size. A curved cannula may be more beneficial for two reasons: the tip of the cannula can be positioned closer to the target nerve; and rotating the tip of a curved cannula will further increase the size of lesion [14]. Unlike CRF, the greatest electrical field is created in front of the needle during PRF. However, rotation of the curved needle seems to maximize the area exposed to the electrical field during PRF [4]. In the present case, using PRF with rotating curved needle technique resulted in a satisfactory outcome without any side effects, which might be attributed to making a larger lesion.
Another problem with PRF procedure is the variable duration of clinical effectiveness due to nerve regeneration. Vallejo et al. [4] reported that the duration of the clinical effect of PRF in SI joint syndrome varied from 6 to 32 weeks. The mean duration of PRF effects in metastatic bone pain are from 2 to 6 months in a case report [9]. The PRF used in our case was effective in that pain relief was maintained for 10 months and did not cause any procedure-related complications. Therefore, considering the limited life expectancy, PRF neuromodulation appears to be an effective treatment modality for patients with metastatic SI joint pain, as well as chronic SI joint syndrome.
In conclusion, this case report describes the first reported use of PRF neuromodulation to relieve the intractable pain associated with SI joint metastases that was refractory to conservative treatment modalities. It is believed that pain control using PRF neuromodulation in the L4-S3 primary dorsal rami and lateral branches can be a high-priority treatment modality for managing localized pain in SI joint metastasis.
Go to : 
References
1. Raque GH Jr, Vitaz TW, Shields CB. Treatment of neoplastic diseases of the sacrum. J Surg Oncol. 2001; 76:301–307. PMID: 11320524.

2. Mercadante S, Fulfaro F. Management of painful bone metastases. Curr Opin Oncol. 2007; 19:308–314. PMID: 17545792.

3. Chua NH, Vissers KC, Sluijter ME. Pulsed radiofrequency treatment in interventional pain management: mechanisms and potential indications-a review. Acta Neurochir (Wien). 2011; 153:763–771. PMID: 21116663.

4. Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph NJ. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med. 2006; 7:429–434. PMID: 17014602.

5. Ripamonti C, Fulfaro F. Malignant bone pain: pathophysiology and treatments. Curr Rev Pain. 2000; 4:187–196. PMID: 10998732.

6. Ramasubba C, Cohen SP. Cooled sacroiliac radiofrequency denervation for the treatment of pain secondary to tumor infiltration: a case-based focused literature review. Pain Physician. 2013; 16:1–8. PMID: 23340529.
7. Cahana A, Van Zundert J, Macrea L, van Kleef M, Sluijter M. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006; 7:411–423. PMID: 17014600.

8. Podhajsky RJ, Sekiguchi Y, Kikuchi S, Myers RR. The histologic effects of pulsed and continuous radiofrequency lesions at 42 degrees C to rat dorsal root ganglion and sciatic nerve. Spine (Phila Pa 1976). 2005; 30:1008–1013. PMID: 15864151.

9. Zeldin A, Ioscovich A. Pulsed radiofrequency for metastatic pain treatment. Pain Physician. 2008; 11:921–922. PMID: 19057638.
10. Cohen SP, Strassels SA, Kurihara C, Crooks MT, Erdek MA, Forsythe A, et al. Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation. Reg Anesth Pain Med. 2009; 34:206–214. PMID: 19587617.

11. Cohen SP, Hurley RW, Buckenmaier CC 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008; 109:279–288. PMID: 18648237.

12. Karaman H, Kavak GO, Tüfek A, Çelik F, Yildirim ZB, Akdemir MS, et al. Cooled radiofrequency application for treatment of sacroiliac joint pain. Acta Neurochir (Wien). 2011; 153:1461–1468. PMID: 21479801.

13. Gofeld M, Faclier G. Radiofrequency denervation of the lumbar zygapophysial joints--targeting the best practice. Pain Med. 2008; 9:204–211. PMID: 18298703.

14. Racz GB, Stanton-Hicks M. Lumbar and thoracic sympathetic radiofrequency lesioning in complex regional pain syndrome. Pain Pract. 2002; 2:250–256. PMID: 17147739.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download