This article has been
cited by other articles in ScienceCentral.
Abstract
Differential diagnosis of posterior neck pain is very challenging based on symptoms and physical examination only. Retropharyngeal calcific tendinitis is a rare and frequently misdiagnosed entity in various causes of neck pain. It results from calcium hydroxyapatite deposition in the longus colli muscle which is characterized by severe neck pain, painful restriction of neck movement, dysphagia, and odynophagia. We herein report a case of a patient with acute retropharyngeal calcific tendinitis, who complained of posterior neck pain, initially diagnosed and treated as a myofascial neck pain syndrome.
Go to :

Keywords: Differential diagnosis, Longus colli, Myofascial pain syndrome, Odynophagia, Posterior neck pain, Retropharyngeal calcific tendinitis
Retropharyngeal calcific tendinitis, also known as acute calcific prevertebral tendinitis, is a rare disease which was first described by Hartley in 1964 [
1]. Calcium hydroxyapatite deposition in the longus colli muscle and associated inflammation is a principal etiology of this disease. The typical signs and symptoms are characterized by acute neck pain and limitation of neck movement, dysphagia and/or odynophagia, low grade fever, mild leukocytosis, and a slightly elevated erythrocyte sedimentation rate. Definitive diagnosis is usually confirmed by detecting amorphous calcifications and prevertebral tissue swelling on radiography, CT, and MRI. Although a few cases have been reported on retropharyngeal calcific tendinitis in Korea, there is no report related with pain management [
23]. It is critical for the pain physician to be aware of this condition to prevent unnecessary evaluation and management in pain practice. In this report, we introduce a case of retropharyngeal calcific tendinitis, which was resolved completely with conservative treatments only. The patient gave consent for their medical records concerning this case to be published.
CASE REPORT
A 25-yr-old relatively healthy male (weight 62 kg, height 178 cm) visited our pain clinic complaining of posterior neck pain and mild limitation of motion for a couple of days. Neck pain was initially of a waxing and waning nature and the numerical rating pain scale (NRS) was 5-6/10. There was no history of trauma, upper respiratory infection, or dental problems. Physical examination revealed no lymphadenopathy but reduced range of motion and moderate tenderness over the posterior neck area. Under the initial impression that the problem was myofascial neck pain syndrome, a trigger point injection with 0.5% mepivacaine 6 ml and dexamethasone 2 mg was performed around the splenius capitis and splenius cervicis muscle area. Additional treatments, including a soft cervical collar, non-steroidal anti-inflammatory drugs (NSAIDs), and muscle relaxants were prescribed for pain control.
Several days later, the patient revisited our clinic with the complaints of worsening neck pain (NRS 7-8/10) and neck stiffness, combined with dysphagia and odynophagia symptoms. He described it as severe neck pain extending into the deep neck and radiating upward to the occiput and vertex of the head. He also complained of difficulty in opening his jaw and swallowing due to throat pain. On physical examination, there was a severely limited range of all neck motion in flexion, extension and rotation due to pain. Mouth opening was difficult but no palpable adenopathy was noted. Cardiopulmonary, abdominal, musculoskeletal, and neurological examinations were all within normal limits. The laboratory tests showed a mild elevation of white blood cell count at 10.1 × 103/µl and an increase of the erythrocyte sedimentation rate (25 mm/h) and C-reactive protein (3.11 mg/dl) accompanied by low grade fever (37.3℃).
An imaging study with a plain radiograph of the cervical spine showed a large area of prevertebral soft tissue swelling from C1 to C5 and focal calcifications anterior to the C1 (
Fig. 1). Given the clinical presentation and plain radiographic finding, a cervical MRI was performed with contrast medium. A sagittal T2 weighted MR image showed a high signal retropharyngeal effusion with acute inferior margin extending from the skull base to the inferior border of C5 (
Fig. 2). After revealing a high signal retropharyngeal effusion on MRI, the patient was referred to a radiologist and otolaryngologist to investigate a further definitive diagnosis. A cervical CT was performed with contrast medium and the bone sagittal view revealed retropharyngeal fluid collection and three calcific deposits anterior to the C1-C2 level (
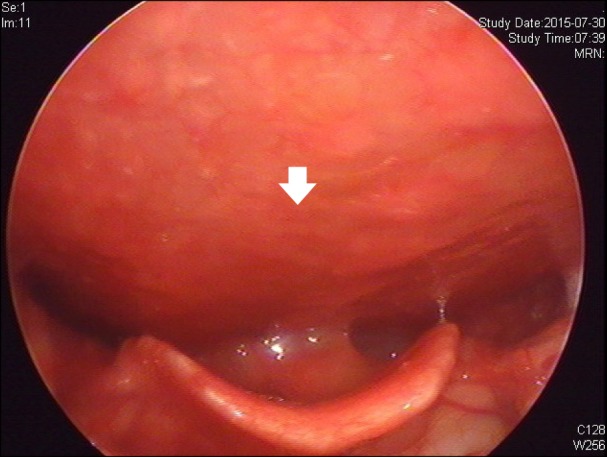
Fig. 3). Because of dysphagia and odynophagia complaints, we consulted the otolaryngologist and he performed a flexible nasopharyngolaryngoscopy which showed posterior pharyngeal wall swelling in the arytenoid (
Fig. 4).
 | Fig. 1Lateral view of the cervical plain radiograph showed a large area of prevertebral soft tissue swelling from C1 to C5 (white arrow) and focal calcifications anterior to the C1 and C2.
|
 | Fig. 2Sagittal T2 weighted MR image shows the high signal retropharyngeal effusion with acute inferior margin extending from the skull base to the inferior border of C5 (white arrow).
|
 | Fig. 3Bone sagittal view of contrast-enhanced computed tomography shows retropharyngeal fluid collection and three calcific deposits anterior to the C1-C2 level (white arrow).
|
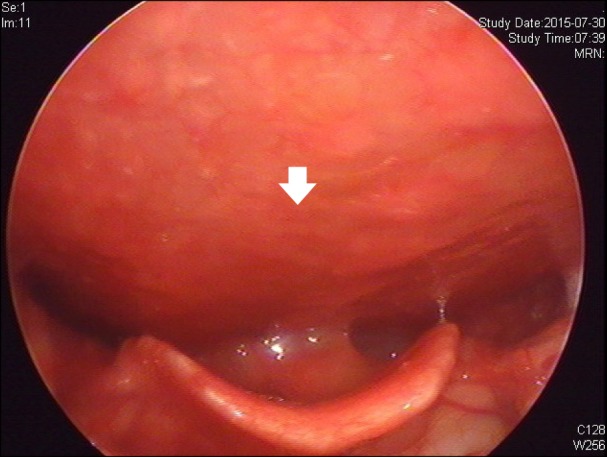 | Fig. 4Nasopharyngolaryngoscopy shows posterior pharyngeal wall swelling overlying arytenoids (white arrow).
|
After considering the clinical presentation and reviewing various radiologic studies in the inter-department conference, the patient was diagnosed with acute retropharyngeal calcific tendinitis of the longus colli muscle rather than myofascial pain syndrome. Because of the retropharyngeal fluid collection and concern over the possibility of a retropharyngeal abscess, the patient was admitted to the hospital and started on regimens of antibiotic and NSAIDs such as intravenous amoxicillin, clindamycin, aconitum, acetylcysteine and intramuscular diclofenac. The posterior neck pain and limitation of neck motion were resolved progressively within approximately a couple of days after the initiation of therapy, and the dysphagia and odynophagia symptoms were also improved within a few days. The patient was discharged with a marked improvement of his disturbing symptoms several days after admission. During two months of follow-up visits, the symptoms were resolved without any significant sequelae, and the follow-up radiograph showed that the preverteral swelling was much improved (
Fig. 5).
 | Fig. 5Follow up lateral view of the cervical plain radiograph showed much improved prevertebral swelling.
|
Go to :

DISCUSSION
In pain clinic practice, it is generally common to meet patients who complain of posterior neck pain that refers to the occiput, shoulder or other areas. Myofascial pain is a one of most common causes of posterior neck pain syndrome with referred pain. Sometimes, differential diagnosis of posterior neck pain is very challenging based on symptoms and physical examination only. Yoon et al. [
4] also reported a case of an intraspinal tumor during treatment of myofascial pain syndrome. An additional difficulty to this process of diagnosis is that clinical manifestations might be the summation of referred pain from multiple myofascial trigger points and even from other structures including bones, joints and visceral organs in patients with musculoskeletal pain [
5].
Retropharyngeal calcific tendinitis, also known as calcific tendinitis of the longus colli muscle, is often unrecognized or misdiagnosed because of its relatively rare occurrence. This entity was first introduced by Hartley in 1964 [
1]. And Ring et al. [
6] determined that the disorder was caused by calcium hydroxyapatite deposition in the longus colli muscle. The pathomechanism of calcium hydroxyapatite deposition is still unknown. Some suggest that repetitive trauma, recent injury, tissue necrosis, or ischemia may play a role in the pathogenesis of calcification [
78]. In this patient, there was no recent history of trauma or upper respiratory infection. It is believed that once the calcium crystals have deposited within the longus colli muscle, they provoke a painful inflammatory response and secondary retropharyngeal effusion.
Clinical manifestations of retropharyngeal calcific tendinitis are relatively nonspecific symptoms such as posterior neck pain and tenderness, motion limitation of the neck, dysphagia, and odynophagia, combined with mild fever, leukocytosis, and an elevated erythrocyte sedimentation rate or C-reactive protein [
7]. Oropharyngeal symptoms of dysphagia and odynophagia are assumed to be caused by the close proximity of the retropharyngeal space to the adjacent pharyngeal constrictors [
9]. In this case, the patient also complaint of dysphagia and odynophagia associated with posterior neck pain on the second visit to the hospital.
The pathognomonic radiographic findings of retropharyngeal calcific tendinitis hold true for plain film, CT, and MRI: prevertebral soft-tissue swelling and amorphous calcification anterior to C1-C2 body. The diffuse, prevertebral soft-tissue thickening usually extends from C1 to C5. The soft-tissue swelling represents either discrete effusion or diffuse edema, which could be discriminated in CT or MRI study. The lack of enhancement surrounding the effusion can be helpful in differentiating a reactive effusion from an infectious abscess [
10]. In this patient, we had a dilemma in diagnosis because there were findings of low signal components and heterogenous enhancement within the effusion on enhanced cervical spine MRI.
Differential diagnosis between retropharyngeal calcific tendinitis and other pathological entites showing similar features, such as an abscess, meningitis, neoplasm, disc herniation, and myofascial neck pain, is considered important concern to avoid unnecessary managements or interventions [
411]. Definitive diagnosis of retropharyngeal calcific tendinitis can be established by computed tomography, the gold standard examination for identifying the presence of prevertebral effusion and calcific deposits around C1 and C2. As also shown in this case, the definitive diagnosis was confirmed from the typical radiologic findings of CT and MRI.
In general, the natural progress of retropharyngeal calcific tendinitis is usually a benign and self-limiting course with conservative care. However, antibiotic treatment or surgical intervention is required in cases of retropharyngeal abscess with high morbidity. NSAIDs are the first-line treatment of retropharyngeal calcific tendinitis, but additional drugs, such as antibiotics, corticosteroids or opioids may be prescribed in severe cases. In this case, fearing retropharyngeal abscess, the otolaryngologist recommended admission and the prescriptions of antibiotics in addition to conservative treatments. Immobilization with a soft cervical collar is another useful method to avoid aggravation of posterior neck pain. Usually, the disturbing symptoms begin to be resolved within a couple of days from the initiation of treatment and the patients become symptom-free after 1-3 weeks of management [
12]. Thorough understanding of this abstruse disease is clinically important, as it can prevent unnecessary evaluation and invasive interventions.
In conclusion, retropharyngeal calcific tendinitis is a cause of acute or subacute neck pain that can be mistaken for myofascial pain syndrome or more ominous diagnoses such as retropharyngeal abscess, meningitis, neoplasm, or other diseases. We report a relatively rare but serious case of retropharyngeal calcific tendinitis which was initially diagnosed and evaluated as a myofascial neck pain syndrome. So, we recommend that a cervical spine CT or MRI should be performed to exclude the possibility of retropharyngeal calcific tendinitis in cases when severe refractory neck pain is combined with oropharyngeal symptoms such as dysphagia and/or odynophagia. In pain medicine practice, the critical importance of recognizing this rare entity lies in preventing the misdiagnosis of posterior neck pain associated with retropharyngeal fluid collections, which might result in unnecessary surgical intervention rather than conservative managements.
Go to :







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download