This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Thoracic epidural anesthesia is frequently used to maintain intraoperative and postoperative analgesia. Frequently, 3 ml of local anesthetic is used as a test dose, or for intermittent epidural injection. We assessed the extent of the spread of 3 ml of contrast medium in the thoracic epidural space and attempted to identify any correlating factors affecting the epidurography.
Methods
A total of 70 patients were enrolled in the study, and thoracic epidural catheterizations were performed under fluoroscopic guidance. Using 3 ml of contrast medium, epidurography was evaluated to confirm the number of spinal segments covered by the contrast medium. Correlation analysis was performed between patient characteristics (sex, age, body mass index, weight, height, and location of catheter tip) and the extent of the contrast spread.
Results
The mean number of vertebral segments evaluated by contrast medium was 7.9 ± 2.2 using 3 ml of contrast medium. The contrast spread in the cranial direction showed more extensive distribution than that in the caudal direction, with statistical significance (P < 0.01). Patient height demonstrated a negative correlation with the extent of distribution of contrast medium (r = −0.311, P < 0.05).
Conclusions
Thoracic epidurography using 3 ml of contrast medium results in coverage of a mean of 7.9 ± 2.2 spinal segments, with more extensive cranial spread, and patient height showed a weak negative correlation with the distribution of contrast medium.
Go to :

Keywords: Correlation, Distribution, Epidurography, Height, Spinal segment, Thoracic epidural anesthesia
INTRODUCTION
Epidural anesthesia and analgesia have been widely used to maintain intraoperative analgesia, and are also employed for postoperative pain management. Thoracic epidural anesthesia (TEA), although not as common as lumbar epidural anesthesia, has also been used for similar purposes. Medications can be delivered either directly through an epidural needle or by means of an epidural catheter inserted in the epidural space. Thoracic epidural catheterization enables repeated or constant delivery of medications into the epidural space during surgery as well as during the postoperative period [
12]. Epidural injection of local anesthetic (LA) with or without opioids is known to provide a better quality of postoperative pain relief compared to the intravenous injection of an opioid [
3456]. In addition, epidural anesthesia induces targeted sympathectomy in the anesthetized region, which results in improvements in local microcirculation and splanchnic vasodilatation [
7]. TEA can also be applied in upper abdominal and thoracic surgery, and it has demonstrated a protective effect against pulmonary complications [
4].
The level of sensory blockade achieved following an epidural injection of LA differs considerably between individuals, and various factors that might affect this distribution remain controversial. Visser et al. [
8] suggested that the total volume of LA appears to be the most important factor in determining the levels of sensory, sympathetic, and motor blockade.
In our clinical practice, after the completion of epidural catheterization, 3 ml of LA is usually administered in the form of intermittent epidural injections to maintain intraoperative analgesia. For the administration of intermittent epidural injections, no other studies have suggested an optimal LA volume that could be used effectively with minimal adverse effects. Furthermore, the spread of sensory blockade after epidural injection of a specific dose of LA can be affected by various individual patient factors; however, these factors remain the subject of debate.
According to a study by Yokoyama et al. [
9], epidural spread of contrast medium correlated well with the spread of LA; therefore, epidurography could predict the dermatomal distribution of sensory blockade.
Therefore, the primary endpoint of the present study was to analyze the thoracic epidurography pattern using 3 ml of contrast medium, which is a frequently used volume for intermittent epidural injections. The secondary endpoint of this study was to identify patient characteristics influencing the extent of contrast spread.
Go to :

MATERIALS AND METHODS
1. Patients
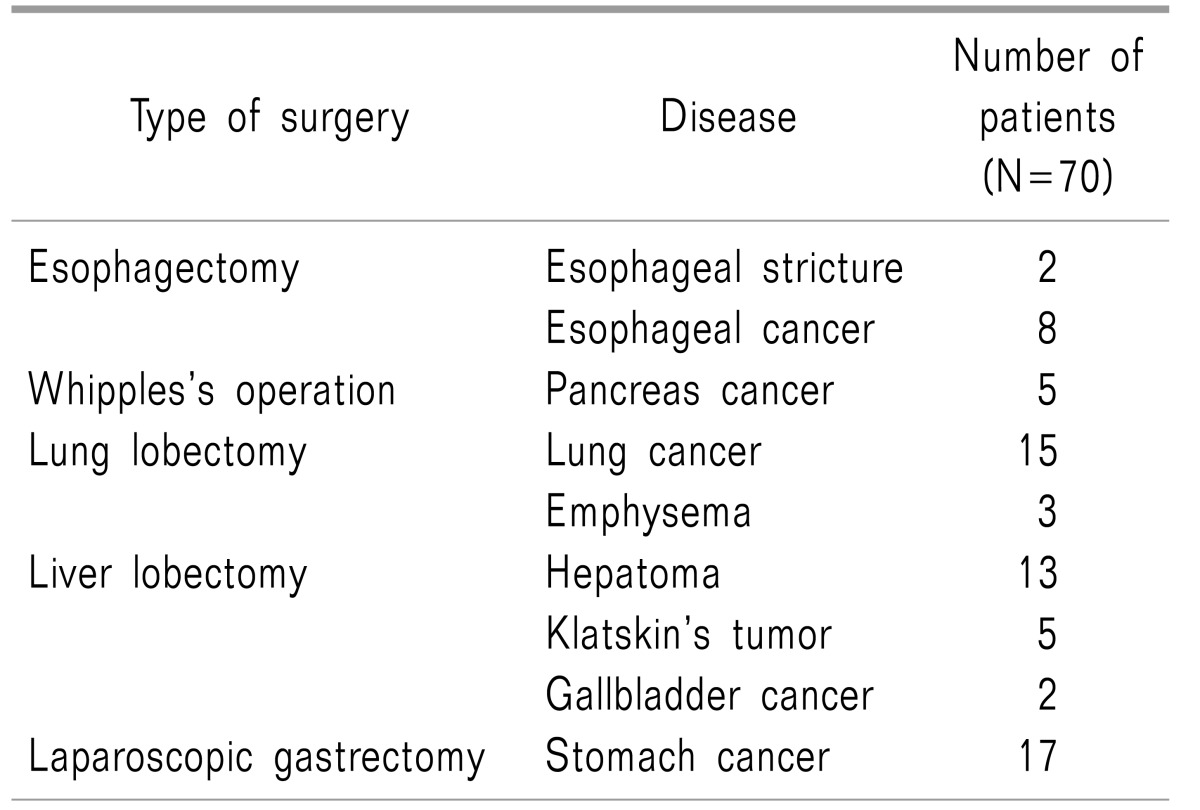
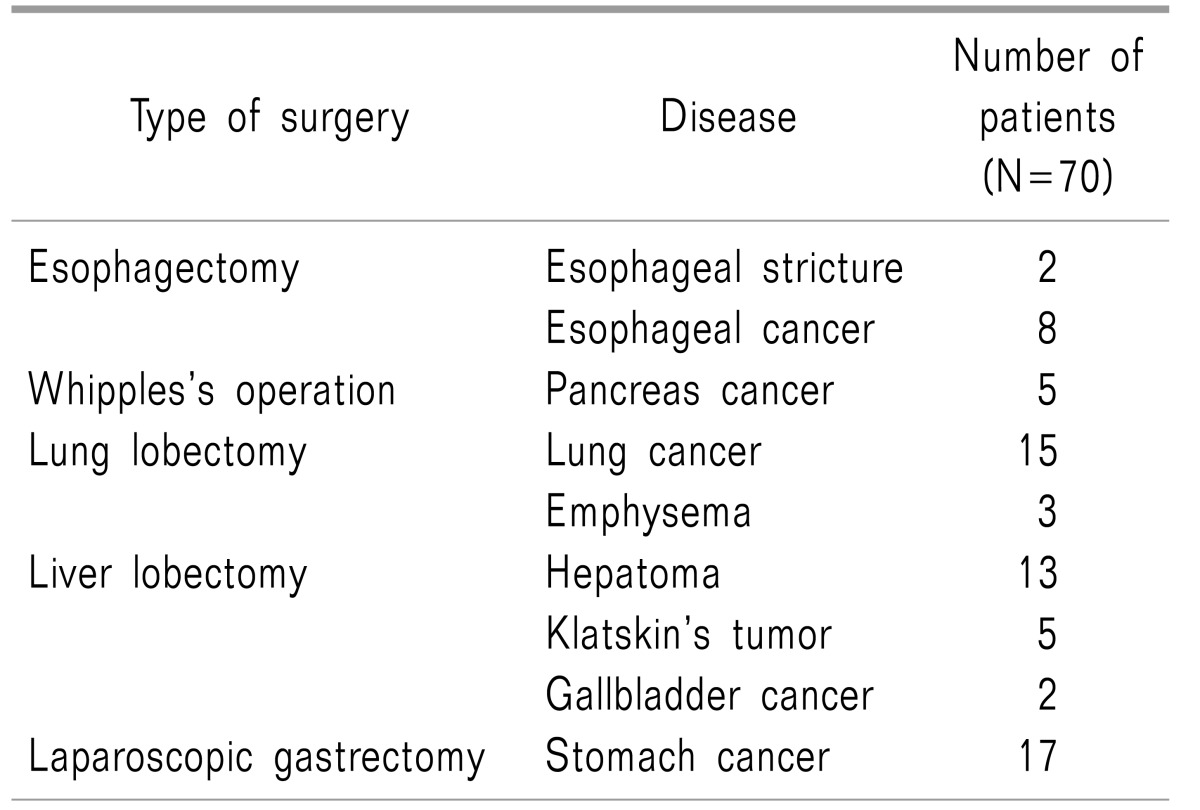
This study was approved by the Institutional Review Board of our institution. We explained the benefits, risks, and goals of the study to the patients and obtained written informed consent from all patients. Study participants included 75 patients who underwent C-arm-guided thoracic interlaminar epidural catheter insertion from March 2015 to February 2016. Patients who were scheduled to receive elective upper abdominal surgery including esophagectomy, liver lobectomy, laparoscopic gastrectomy, and lung lobectomy underwent thoracic epidural catheter insertion under C-arm guidance one day before elective surgery (
Table 1).
Table 1
The Distribution of Disease and Type of Surgery Who Received Thoracic Epidural Catheterization

We included patients who had stopped taking anticoagulants for the required time before thoracic epidural catheter insertion. We excluded pregnant patients, as well as those with laboratory findings suggesting infection, inflammation, or coagulopathy; those with allergy to contrast medium or LA; and those with a previous history of spinal surgery at the thoracic or lumbar level.
Five patients were excluded due to refusal to participate in the study. Finally, 70 patients were enrolled, and 70 cases of thoracic epidurography during epidural catheterization were analyzed.
2. Procedures
All catheter insertions (Arrow International CR, Hradec Králové, Czech Republic) were performed by an interventional pain physician with more than 10 years of experience in image-guided injections. Patients were placed in the prone position and draped in a sterile fashion. Anteroposterior (AP) views were obtained to confirm the T10-11 interlaminar space. After skin infiltration with 1 ml of 1% lidocaine, an 18 G Tuohy needle was inserted toward the paramedian interlaminar site of T10-11 and advanced slowly into the midline using loss of resistance with air under AP fluoroscopic views. When loss of resistance was felt, lateral fluoroscopic views were obtained to confirm that the needle was located within the posterior spinal canal. After checking the final needle position, we confirmed the epidural injection using 0.5 to 1 ml of contrast medium with AP and lateral fluoroscopic images.
3. Primary endpoint: analysis of thoracic epidurography
In cases of successful epidural injection, an epidural catheter was inserted through the Tuohy needle, and it was directed in the cranial direction. Prior to insertion of the catheter, a small amount of contrast medium was passed through the catheter to verify placement of the catheter tip. When the catheter was curled within the epidural space, it was pulled slightly to straighten it. Before the injection of 3 ml of contrast medium, the final location of the catheter tip was evaluated. An attempt was made to adjust the location of the catheter tip to between T7 and T8. Following the final assessment of the location of the catheter tip, 3 ml of contrast medium was injected through the epidural catheter to assess and evaluate the thoracic epidurography.
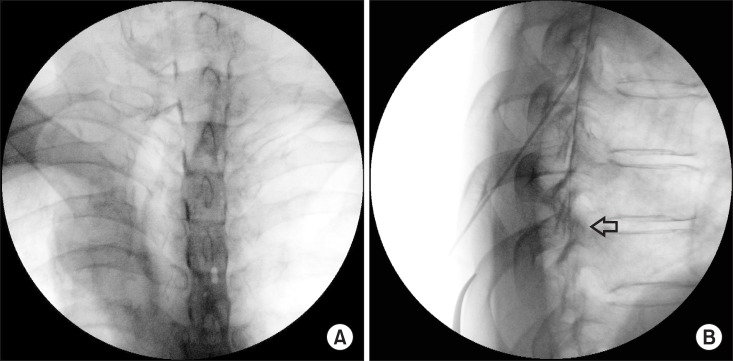
The primary goal was determination of the number of spinal segments covered by contrast medium. To evaluate the this, the cranial and caudal ends of spinal segments on the lateral view were examined. However, it was very difficult to examine the pattern of contrast spread to the first to third thoracic vertebrae on the lateral view due to the shoulder joint; therefore, the AP fluoroscopic image was used in such cases.
We assessed the unilateral or bilateral epidural spread by checking the AP fluoroscopic images (
Fig. 1A). In order to evaluate the total number of spinal segments covered by contrast medium more precisely, we created our own set of definite rules to determine which vertebrae should be included in the count. According to these rules, the count included the spinal segments covered by contrast medium for more than half of their vertebral body height on the lateral view, and excluded the segments with the contrast medium spread covering less than half of their vertebral body height (
Fig. 1B). Following completion of the epidural catheterization and epidurography study, patients returned to their hospital room, and the next day, upper abdominal or thoracic surgery was performed under general anesthesia combined with TEA.
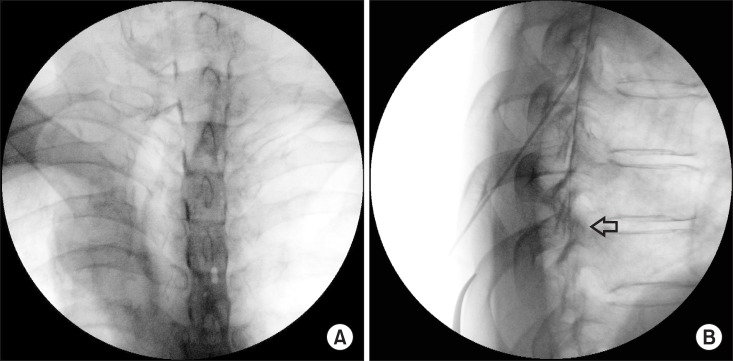 | Fig. 1Unilateral or bilateral epidural spread was checked through the anteroposterior fluoroscopic image (A) and the extent of contrast medium spread was assessed by evaluating the amount of contrast medium spread covering the vertebral body height through the lateral fluoroscopic image. Arrow indicates that contrast medium covers more than half of the vertebral body height (B).
|
4. Secondary endpoint: correlation factors
We collected patient clinical data including sex, age, body mass index (BMI), weight, and height through review of medical records, and recorded the location of the catheter tip through the analysis of fluoroscopic images.
We attempted to identify any correlation factors that affected the distribution of contrast medium during TEA.
5. Statistical analysis
As there were no previous data for contrast distribution patterns in TEA, we performed an initial preliminary study to obtain an estimate of the proper sample size. According to our preliminary study, epidural cranial spread was higher than that in the caudal direction. We assumed that the mean difference in spinal segments between the uppermost cranial and lowermost caudal spread would be 5.5. Assuming a mean difference of contrast medium spread between the uppermost cranial and lowermost caudal directions of 5.5 segments, an α level of 0.05, and a β level of 0.2, 65 patients undergoing TEA were required for a power of 80%.
We performed correlation analysis to identify any factors that affected the distribution of contrast medium during TEA. Pearson's (age, BMI, weight, height, and location of catheter tip) or Spearman's (sex) correlation coefficient was calculated according to the type of variables. SPSS version 20 (IBM, Armonk, NY, USA) was used for statistical analysis. Data are expressed as mean ± standard deviation (SD). A P value < 0.05 was considered to indicate statistical significance.
Go to :

RESULTS
For this study, 70 patients (49 men and 21 women) with a mean age of 61 years were enrolled, and 70 cases of thoracic epidural catheterizations were analyzed. There were no serious adverse events related to the procedure. Included patients underwent surgeries such as laparoscopic gastrectomy, esophagectomy, liver lobectomy, and lung lobectomy. More than half of the patients received liver and lung lobectomies, and 65 patients were diagnosed with cancer (
Table 1).
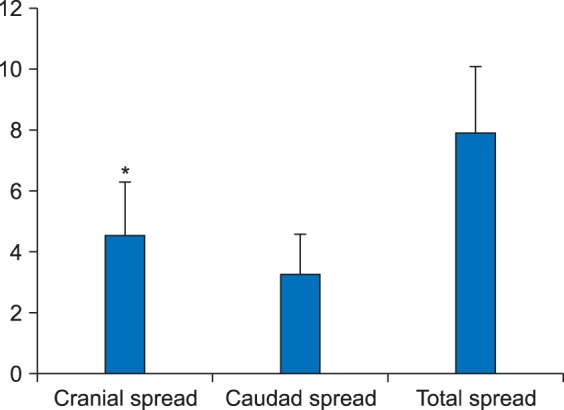
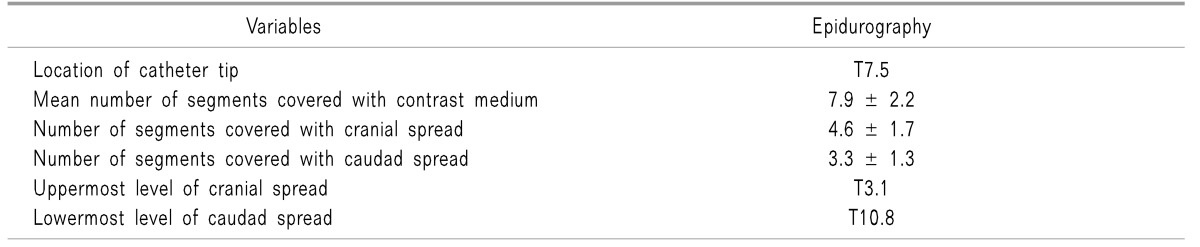
The mean number of vertebral segments covered by contrast medium spread was 7.9 ± 2.2 using 3 ml of contrast medium, and the segments were counted in both the cranial and caudal directions. The contrast medium spread in the cranial direction showed more extensive distribution than that in the caudal direction and the difference showed statistical significance (
P < 0.01). The uppermost level of cranial spread was T3.1, and the lowermost level of caudal spread was T10.8 (
Table 2,
Fig. 2). All patients showed even bilateral distribution of contrast medium (
Fig. 1A).
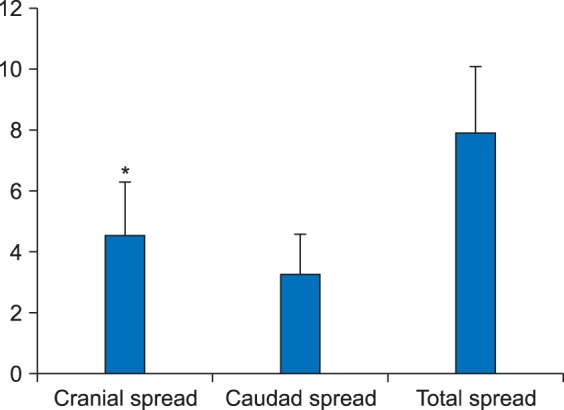 | Fig. 2The number of spinal segments of cranial, caudad and total (both direction) spread of contrast medium. Cranial spread showed extensive distribution compated to caudad spread, and it was statistically significant (P < 0.01).
|
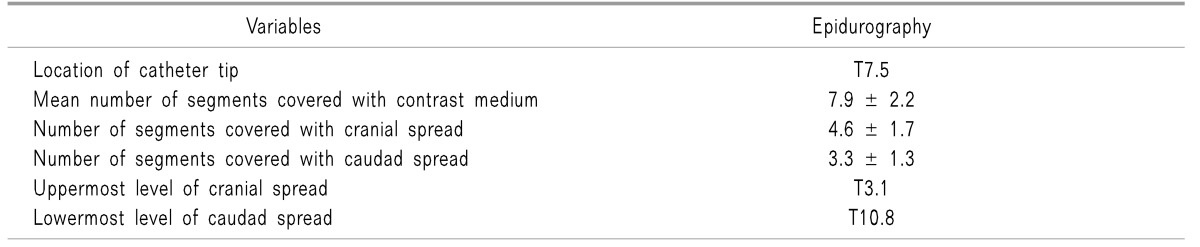
Table 2
The Mean Vertebral Segment of Thoracic Epidural Contrast Flow at the Catheter Tip

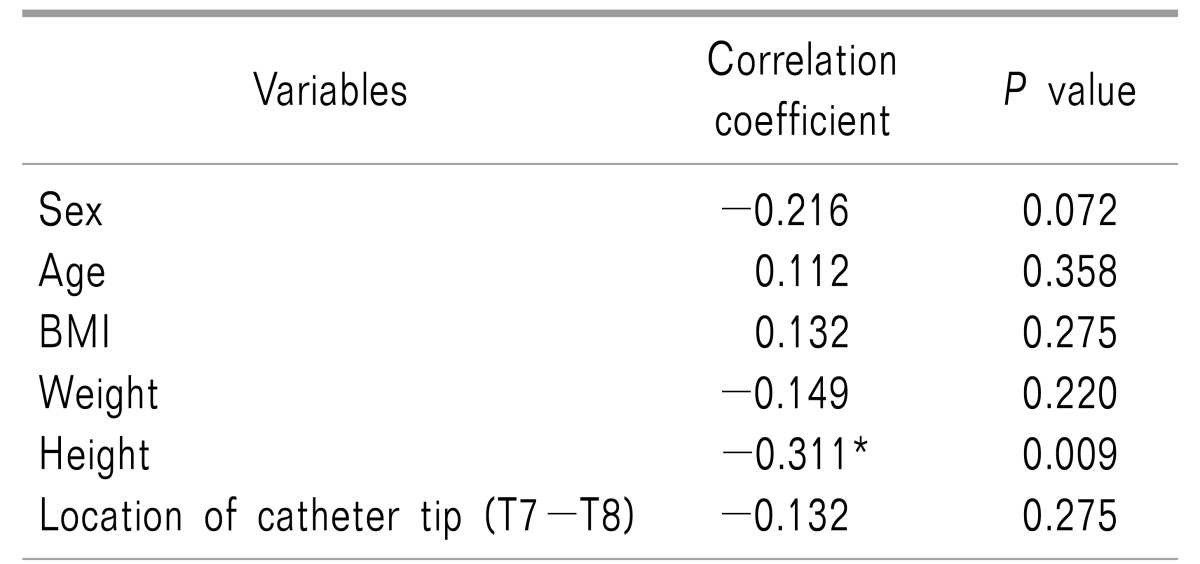
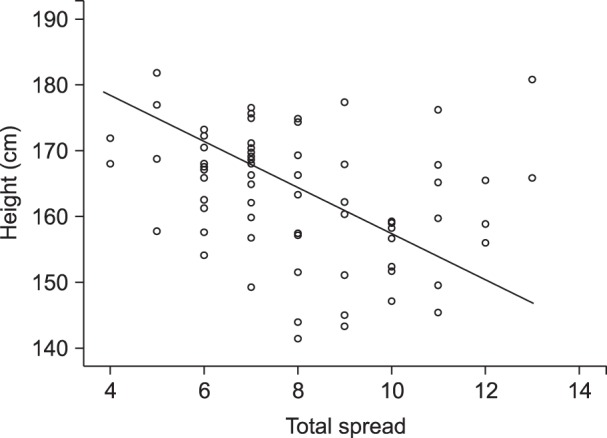
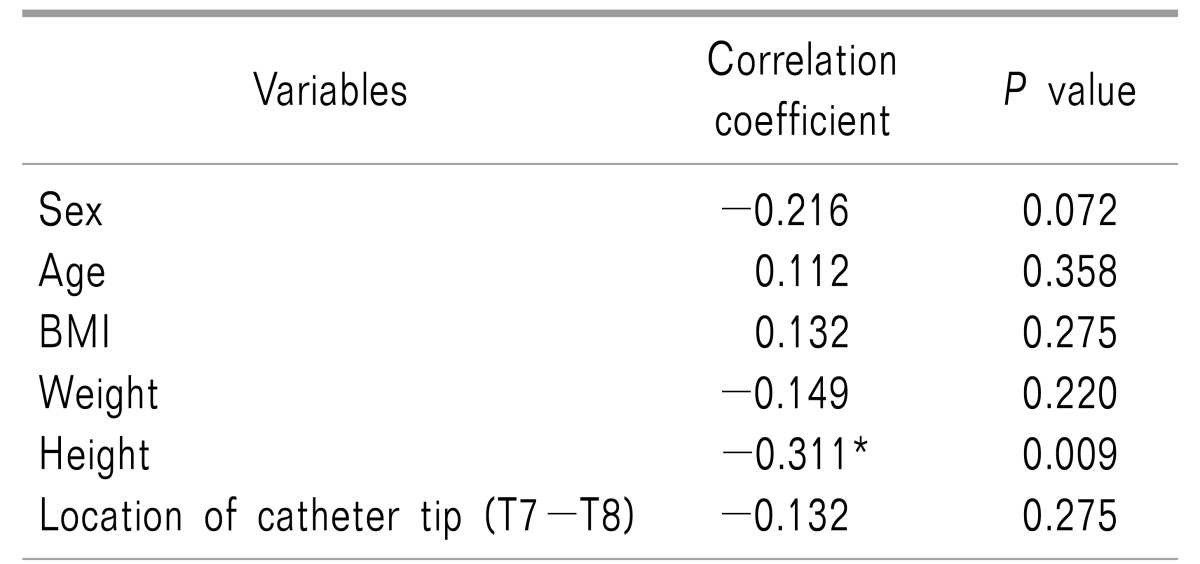
Correlation analysis was performed between various patient characteristics and the extent of contrast medium spread during TEA. The results of the analysis showed that patient height demonstrated a negative correlation with the extent of distribution of constrast medium (r = −0.311,
P < 0.05) (
Table 3,
Fig. 3).
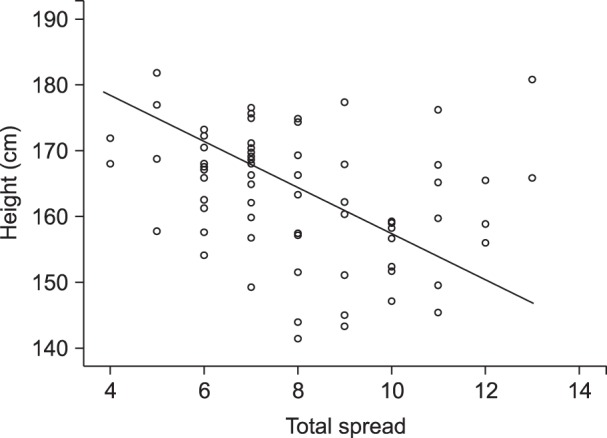 | Fig. 3Scatter plot showing the negative correlation of height (cm) and the extent of contrast medium spread during thoracic epidurography.
|
Table 3
Pearson's or Spearman's Correlation Coefficient of the Variables on the Extent of Contrast Medium Spread during Thoracic Epidurography

Go to :

DISCUSSION
This study was performed under the assumption that contrast medium distribution during epidurography could predict the dermatomal distribution of sensory blockade. Yokoyama et al. [
9] concluded that the spread of contrast medium has a clear correlation with the extent of LA blockade. In addition, according to the study by Kim et al. [
10], the viscosity of the contrast medium has little influence on its epidural spread.
Our study of thoracic epidurography demonstrated that a volume of 3 ml of contrast medium showed a distribution of total contrast spread to a mean of 7.9 ± 2.2 segments. The mean levels of the greatest cranial and caudal spread were T3.1 and T10.8, respectively. It is suggested that a TEA blockade of 10 dermatomes without general anesthesia is required for upper abdominal or thoracic surgery [
11]. Therefore, we believe that a sensory blockade of 8 segments encompassing T3 to T10 would be sufficient to maintain intraoperative analgesia for thoracoabdominal surgery in combination with general anesthesia.
The contrast medium spread in the cranial direction showed more extensive distribution than that in the caudal direction, with statistical significance. This finding was also observed in an epidurography study of the cervical spine. Regardless of the volume of injected contrast medium, all groups showed more extensive distribution in the cranial direction compared to the caudal direction [
12]. According to a study by Huang [
13], cervical epidural anesthesia with 2% lidocaine resulted in reduced lung volumes and capacities due to a paralytic effect on the intercostal muscles and diaphragm innervated by the thoracic intercostal and phrenic nerves, respectively. In addition, these pulmonary functions can show reductions of up to 20% or 30% from the baseline if sensory blockade reaches higher levels of the vertebral column [
14]. Considering these respiratory complications for high thoracic and cervical epidural anesthesia, excessive cranial and cervical level distribution of medication should be avoided. Furthermore, excessive neck flexion during high TEA was found to increase cranial spread of contrast medium [
15].
During lumbar epidural anesthesia, insufficient sensory blockade of one leg compared to the other may be observed, although this is infrequent. In such cases, unilateral distribution of the medication may by suspected, either to the right or left side. In the present study, every patient showed even and bilateral distribution of the contrast medium.
Our epidurography study showed that among various clinical variables, patient height showed a weak negative correlation with the extent of contrast medium spread during TEA. It seems logical to suppose that taller patients require more LA to achieve a certain level of blockade compared to shorter patients. In TEA, correlation coefficients ranging from −0.25 to −0.37 have been found between the spread of epidurally injected contrast medium and patient height [
916].
In contrast to the conflicting results regarding lumbar epidural anethesia, the effect of age on epidural spread during TEA showed a strong positive correlation (r = 0.70) [
816]. Several mechanisms have been suggested to explain this correlation, including decreased leakage of LA through the intervertebral foramina, compliance of the epidural space, and changes in fatty tissue with increasing age; however, it remains uncertain which of these acts as a true mechanism [
81617]. We were unable to find any correlation between age and the extent of contrast medium spread in the present study. All patients included in this study were scheduled to undergo upper abdominal or thoracic surgery, in most cases due to the development of cancer. Therefore, the distribution of age range was confined to older ages (52-83 years old). We believe that this biased age distribution accounted for the failure of our study to demonstrate a positive correlation between age and contrast medium distribution.
We were unable to find any correlation between weight or BMI and the exent of contrast medium spread. Few studies have observed a correlation between weight and level of sensory blockade [
8].
It seems apparent that the increased abdominal pressure and increased presence of body fat that follow the development of obesity are not sufficient to affect the spread of epidural blockade. Body weight and BMI demonstrated poor correlations with the amount of posterior epidural fat, while they showed a positive correlation with posterior subcutaneous body fat deposition [
818].
Our study has several limitations. This study was performed under the assumption that contrast medium distribution is equivalent to the distribution of LA. It should be noted that results based on the use of contrast medium may not always coincide with the epidural spread of LA. However, we performed an additional study to evaluate any discrepancies between the spread of contrast medium and that of LA, and the difference between the two was within 1 dermatome. We used a small test dose of contrast medium to confirm that the contrast was in the epidural space, not the intrathecal or vascular space, prior to injection of the main dose of contrast medium. The present study did not include the exact volume of the test dose. We attempted to identify any correlation factors that might affect the distribution of the contrast medium; however, some factors such as age had limited potential to show any correlation due to a biased age distribution.
Future studies enrolling greater numbers of patients with minimally biased distributions of clinical variables are needed.
In summary, thoracic epidurography using 3 ml of contrast medium demonstrated a spread of 8 segments encompassing T3 to T10. We believe that an injection volume of 3 ml would be sufficient for intermittent epidural administration for upper abdominal and thoracic surgery while avoiding excessive upper thoracic and cervical spread. Patient height showed a negative correlation with the extent of the contrast medium spread.
Go to :

ACKNOWLEDGEMENTS
We would like to give special thanks to Eun Suk Kim, Eun Bi Kim and Jin A Lee who did a contribution making high quality figures and analyzing statistics.
Go to :

References
1. Zhang D, Fujiwara R, Iseri T, Nagahama S, Kakishima K, Kamata M, et al. Distribution of contrast medium epidurally injected at thoracic and lumbar vertebral segments. J Vet Med Sci. 2013; 75:663–666. PMID:
23292108.

2. Gessler F, Mutlak H, Tizi K, Senft C, Setzer M, Seifert V, et al. Postoperative patient-controlled epidural analgesia in patients with spondylodiscitis and posterior spinal fusion surgery. J Neurosurg Spine. 2016; 24:965–970. PMID:
26849711.

3. Nishimori M, Low JH, Zheng H, Ballantyne JC. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database Syst Rev. 2012; CD005059. PMID:
22786494.

4. Pöpping DM, Elia N, Marret E, Remy C, Tramèr MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: a meta-analysis. Arch Surg. 2008; 143:990–999. PMID:
18936379.

5. Kim SH, Yoon KB, Yoon DM, Kim CM, Shin YS. Patient-controlled epidural analgesia with ropivacaine and fentanyl: experience with 2,276 surgical patients. Korean J Pain. 2013; 26:39–45. PMID:
23342206.

6. Park SK, Choi YS, Choi SW, Song SW. A comparison of three methods for postoperative pain control in patients undergoing arthroscopic shoulder surgery. Korean J Pain. 2015; 28:45–51. PMID:
25589946.

7. Windisch O, Heidegger CP, Giraud R, Morel P, Bühler L. Thoracic epidural analgesia: a new approach for the treatment of acute pancreatitis? Crit Care. 2016; 20:116. PMID:
27141977.

8. Visser WA, Lee RA, Gielen MJ. Factors affecting the distribution of neural blockade by local anesthetics in epidural anesthesia and a comparison of lumbar versus thoracic epidural anesthesia. Anesth Analg. 2008; 107:708–721. PMID:
18633056.

9. Yokoyama M, Hanazaki M, Fujii H, Mizobuchi S, Nakatsuka H, Takahashi T, et al. Correlation between the distribution of contrast medium and the extent of blockade during epidural anesthesia. Anesthesiology. 2004; 100:1504–1510. PMID:
15166571.

10. Kim YC, Lim YJ, Lee SC. Spreading pattern of epidurally administered contrast medium in rabbits. Acta Anaesthesiol Scand. 1998; 42:1092–1095. PMID:
9809094.

11. Iwata Y, Hamai Y, Koyama T. Anesthetic management of nonintubated video-assisted thoracoscopic surgery using epidural anesthesia and dexmedetomidine in three patients with severe respiratory dysfunction. J Anesth. 2016; 30:324–327. PMID:
26758074.

12. Kim KS, Shin SS, Kim TS, Jeong CY, Yoon MH, Choi JI. Fluoroscopically guided cervical interlaminar epidural injections using the midline approach: an analysis of epidurography contrast patterns. Anesth Analg. 2009; 108:1658–1661. PMID:
19372351.

13. Huang CH. Effect of cervical epidural blockade with 2% lidocaine plus epinephrine on respiratory function. Acta Anaesthesiol Taiwan. 2007; 45:217–222. PMID:
18251242.
14. Groeben H. Epidural anesthesia and pulmonary function. J Anesth. 2006; 20:290–299. PMID:
17072694.

15. Lee CJ, Jeon Y, Lim YJ, Bahk JH, Kim YC, Lee SC, et al. The influence of neck flexion and extension on the distribution of contrast medium in the high thoracic epidural space. Anesth Analg. 2007; 104:1583–1586. PMID:
17513662.

16. Saitoh K, Hirabayashi Y, Shimizu R, Mitsuhata H, Fukuda H. Extensive extradural spread in the elderly may not relate to decreased leakage through intervertebral foramina. Br J Anaesth. 1995; 75:688–691. PMID:
8672314.

17. Igarashi T, Hirabayashi Y, Shimizu R, Saitoh K, Fukuda H, Mitsuhata H. The lumbar extradural structure changes with increasing age. Br J Anaesth. 1997; 78:149–152. PMID:
9068330.

18. Wu HT, Schweitzer ME, Parker L. Is epidural fat associated with body habitus? J Comput Assist Tomogr. 2005; 29:99–102. PMID:
15665692.

Go to :





 Citation
Citation Print
Print


 XML Download
XML Download