Abstract
Muscular hypertrophy is caused mainly due to myopathic disorder. But, it is also rarely produced by neurogenic disorder. A 74-year-old woman complained of right calf pain with hypertrophy for several years. Recent lumbar spine magnetic resonance imaging (MRI) showed central and lateral canal narrowing at the L4-L5 intervertebral space. Lower extremity MRI revealed fatty change of right medial head of the gastrocnemius and soleus, causing right calf hypertrophy. Electrodiagnostic examinations including electromyography and nerve conduction velocity testing demonstrated 5th lumbar and 1st sacral polyradiculopathy. Integrating all the results, the diagnosis was neurogenic muscle hypertrophy. Neurogenic muscle hypertrophy is very rare, but we recommend that clinicians consider this problem when a patient complains of lower limb hypertrophy and pain.
Go to : 
Muscular hypertrophy is caused mainly due to myopathic disorder. But, it is also rarely produced by neurogenic disorder [1]. Radiculopathy is one of the neurogenic disorders which has symptoms such as pain, paresthesia, numbness, and hypotonia that involves its dermatome that is innervated by the corresponding nerve root. We experienced a case of unilateral calf muscle hypertrophy involving the right lumbar 5th (L5) and 1st sacral (S1) radiculopathy. We present details of this case with a review of the pertinent literature.
A 74 year old woman visited our clinic, who had been suffering from pain in the low back and right lower limbs and right calf hypertrophy. Six years ago, the patient had experienced low back pain and right 5th lumbar (L5) radiating pain. At that time, the patient had been diagnosed as spinal stenosis between the 4th lumbar (L4) and 5th lumbar (L5) intervertebral space by lumbar spine magnetic resonance imaging (MRI) and a hemi-laminectomy with interspinal device insertion had been done at another hospital. The patient had no specific past history except the surgery. 5 years before the present visit, low back pain and right L5 and S1 radiating pain were developed. And calf hypertrophy had been developed in 3 years ago.
She described her pain as a continuous dull pain in the low back area and along the right L5 and S1 dermatomes. This pain worsened while walking and was alleviated with rest. At the time of presentation, the patient's pain level was 70/100 mm on visual analogue scale (VAS) from 0/100 mm (no pain) to 100/100 mm (worst pain imaginable). The patient was unable to walk more than 150 m due to pain.
A physical examination showed 50% sensory loss along the right L5 and S1 dermatomes, using pin pricking and light touching. The 6-scale muscle strength test that goes from grade 0 (no evidence of muscle contractility) to grade 5 (normal: complete range of motion against gravity with full resistance) revealed decreasing power of ankle plantar flexion at Grade 4 (good: complete range of motion against gravity with some resistance) out of 5 on the right side. In deep tendon reflex (DTR), the knee jerk was normal (2+/2+), however, ankle jerk on the right site was decreased (1+/2+). The straight leg raising test showed a positive result at 45° in the right lower limb. The pulsation of the dorsalis pedis artery was normal. When we measured calf girth, the left side was 37 cm, while the right side was 42 cm.
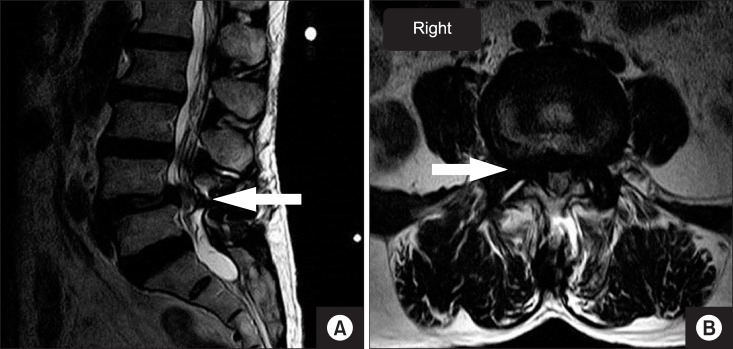
Lumbar MRI, lower extremity MRI, electromyography (EMG) and a nerve conduction velocity (NCV) test and laboratory test was done for diagnosis. In a recent lumbar MRI, central and lateral canal narrowing was revealed central and lateral canal narrowing at the L4-L5 intervertebral space (Fig. 1). A lower extremity MRI that was done to confirm the reason for the right lower limb hypertrophy revealed a complete fatty change accompanying the right medial head of the gastrocnemius, and hypertrophy of the soleus (Fig. 2). Also, following electrodiagnostic examinations including electromyography (EMG) and nerve conduction velocity (NCV) testing, the chronic state of right L5 and S1 polyradiculopathy was evident. The levels of Creatinine kinase (CK), CK-MB and alkaline phosphatase (ALP) were normal respectively. Doppler ultrasound examination did not reveal deep vein thrombosis. Therefore, the right unilateral calf hypertrophy was diagnosed as neurogenic muscle hypertrophy.
We performed right an L5, S1 selective transforaminal epidural block using, in each instance, 5 mg of triamcinolone and 2.5 ml of 0.5% mepivacaine for the low back pain and the right L5, S1 radiating pain. Pregabalin, a non-steroidal anti-inflammatory drug, and muscle relaxant were prescribed for 2 weeks. The low back pain and right lower limb radiating pain were alleviated, as judged by a VAS score of 20/100 mm after treatment. 4 months later, she fell down on the road. The low back pain and right leg pain were increased, as judged by a VAS score of 50/100 mm. So, the patient was prescribed pregabalin and tramadol for 2 weeks. Two weeks later, her pain was decreased to a VAS score of 30/100 mm. Therefore, other invasive procedures weren't needed. We are still constantly observing the diameter of the right calf, which has not changed in the past 6 months.
Go to : 
Neurogenic muscle hypertrophy is also termed "denervation hypertrophy". It was first described in the 19th century and has been occasionally reported thereafter [2,3]. It is mostly caused by nerve root compression. Among the body regions deformed by hypertrophy, the calf is predominantly involved, and comprises 78% of all known reports. Calf hypertrophy can be caused by L5, S1 nerve root compression [4,5], as in the present case.
The pathophysiology of neurogenic muscle hypertrophy is still not clear. However, two theories have been suggested. One posits that the hypertrophy is produced as a secondary result of chronic muscle stimulation. In a case that features chronic muscle stimulation, EMG will reveal constant and abnormal complex repetitive discharges, such as Myokymia, which is caused by the involuntary trembling of muscle fibers, and neuromyotonia, which involves peripheral nerve muscle fiber activity as a result of abnormal nerve stimulation [6,7]. The second theory posits that hypertrophy of muscle fiber results from excessive exercise loading in the innervated muscle fiber [6].
In the present case, the muscle weakness or decreased DTR could have had a neurogenic cause based on a physical examination. The patient had mild muscle weakness consistent with a rank of grade 4 in ankle plantar flexion. The gastrocnemius and soleus are the muscles related with ankle plantar flexion, in which part of the innervation is from the tibial nerve from the S1-2 nerve root. We also discovered a sensory decrease from the dermatome, which is managed by L5 and S1. According to the deep tendon reflex, there was decreased right ankle jerk with a 1+ lesion. To identify the result clearly, we performed lumbar spine MRI which showed lateral canal narrowing central and lateral canal narrowing at the L4-L5 intervertebral space. The congruity of the imaging findings and the physical examination results indicate a high reliability of the final result.
There are many differences between myopathic muscle hypertrophy and neurogenic muscle hypertrophy [6,8,9,10,11]. Myopathic muscle hypertrophy is evident with a diffuse lesion, which is centralized on the muscle, not a nerve innervated lesion. Conversely, neurogenic muscle hypertrophy is mostly an isolated muscle innervated by an abnormal nerve. To confirm the lesion on the right calf, we checked both lower extremities using MRI. Muscle hypertrophy characterized by fatty change and pseudohypertrophy was focused on the gastrocnemius and soleus. Myopathic muscle hypertrophy increases muscle enzymes (CK, CK-MB, ALP), but in neurogenic hypertrophy the increase is mild, or the levels remains normal. In this case, there was a normal level from muscle enzyme test. According to the history of the patient, there was no particular muscular and metabolic disease, or excessive exercise history. According to the EMG and nerve conduction velocity results, we could not confirm any decreased duration of motor unit potential, which is the most sensitive and specific parameter in myopathic muscle hypertrophy. In this case, right L5 and S1 polyradiculopathy was noted. The collective observations supported the diagnosis as neurogenic muscle hypertrophy. Among the various causes of neurogenic muscle hypertrophy, such as anterior horn cell disease, plexopathy, sciatic nerve injury, and polyneuropathy, we can confidently conclude that L5, S1 nerve roots compression caused the sustained and exacerbated symptoms in this patient.
Neurogenic muscle hypertrophy shows increased size and number of muscle fibers [3], internal nucleation, fiber splitting and disruption of intermyofibrillar architecture in muscle biopsies on the affected muscles [12].
The treatment of neurogenic muscle hypertrophy has not been clearly reported. Treatment can involve surgery or can be nonsurgical. In nonsurgical treatment, an injection of botulinum toxin [13] and steroid medication [14] are effective. In surgical treatment, Gibson and Waddell [15] reported that microdiscectomy is the effective way to reduce radiculopathy and muscle hypertrophy. In the present case, we performed a right L5, S1 selective transforaminal epidural block to relieve right L5, S1 radiating pain. After that, radiating pain was relieved and patient was informed about the disease and further management. But, the patient didn't want to take the treatment. We found that the selective transforaminal epidural block decreased pain, but was not enough to improve the calf muscle hypertrophy.
In conclusion, muscular hypertrophy has a myopathic cause and a neurogenic cause. To discriminate between these, a proper neurologic examination and laboratory tests such as muscle enzyme test, EMG, MRI, and muscle biopsy are needed. Neurogenic muscle hypertrophy is very rare, but we recommend clinicians consider this problem when patients complain of lower limb hypertrophy and pain.
Go to : 
References
1. Gutmann L. AAEM minimonograph #46: neurogenic muscle hypertrophy. Muscle Nerve. 1996; 19:811–818. PMID: 8965832.

2. Pareyson D, Morandi L, Scaioli V, Marazzi R, Boiardi A, Sghirlanzoni A. Neurogenic muscle hypertrophy. Report of two cases. J Neurol. 1989; 236:292–295. PMID: 2760647.
3. Deffond D, Clavelou P, Colamarino R, Roche C, Dordain G, Tournilhac M. Neurogenic muscle hypertrophy: 3 cases. Rev Neurol (Paris). 1996; 152:272–278. PMID: 8763656.
4. Krendel DA, Hedaya EV, Gottleib AJ. Calf enlargement, S1 radiculopathy, and focal myositis. Muscle Nerve. 1992; 15:517–518. PMID: 1565123.
5. Heuss D, Schober S, Eberhardt K, Probst-Cousin S, Kayser C, Hecht M, et al. Muscle hypertrophy due to scarring of the S1 nerve root. Neurol Res. 2000; 22:469–472. PMID: 10935218.
6. Walcott BP, Nahed BV, Redjal N, Stein TD, Kahle KT, Coumans JV. Pathological mechanism of lumbar disc herniation resulting in neurogenic muscle hypertrophy. J Clin Neurosci. 2011; 18:1682–1684. PMID: 21985744.

7. Beydoun SR, Shapiro C, Engel WK. Calf muscle hypertrophy, complex repetitive discharges and spinal stenosis. Muscle Nerve. 1993; 16:322–323. PMID: 8446132.
8. Mattle HP, Hess CW, Ludin HP, Mumenthaler M. Isolated muscle hypertrophy as a sign of radicular or peripheral nerve injury. J Neurol Neurosurg Psychiatry. 1991; 54:325–329. PMID: 2056318.

9. Liguori R, Fuglsang-Frederiksen A, Nix W, Fawcett PR, Andersen K. Electromyography in myopathy. Neurophysiol Clin. 1997; 27:200–203. PMID: 9260160.

10. Garmirian LP, Chin AB, Rutkove SB. Discriminating neurogenic from myopathic disease via measurement of muscle anisotropy. Muscle Nerve. 2009; 39:16–24. PMID: 19058193.

11. Swartz KR, Fee DB, Trost GR, Waclawik AJ. Unilateral calf hypertrophy seen in lumbosacral stenosis: case report and review of the literature. Spine (Phila Pa 1976). 2002; 27:E406–E409. PMID: 12634577.
12. Lattanzi S, Cagnetti C, Di Bella P, Scarpelli M, Provinciali L, Silvestrini M. Neurogenic muscle hypertrophy. Neurology. 2014; 83:2191. PMID: 25452457.

13. Costa J, Graça P, Evangelista T, de Carvalho M. Pain and calf hypertrophy associated with spontaneous repetitive discharges treated with botulinum toxin. Clin Neurophysiol. 2005; 116:2847–2852. PMID: 16256429.

Go to : 




 Citation
Citation Print
Print



 XML Download
XML Download