This article has been
cited by other articles in ScienceCentral.
Abstract
The musculoskeletal system is mainly composed of the bones, muscles, tendons, and ligaments, in addition to nerves and blood vessels. The greatest difficulty in an ultrasonographic freeze-frame created by the examiner is recognition of the targeted structures without indicators, since an elephant's trunk may not be easily distinguished from its leg. It is not difficult to find descriptive ultrasonographic terms used for educational purposes, which help in distinguishing features of these structures either in a normal or abnormal anatomic condition. However, the terms sometimes create confusion when describing common objects, for example, in Western countries, pears have a triangular shape, but in Asia they are round. Skilled experts in musculoskeletal ultrasound have tried to express certain distinguishing features of anatomic landmarks using terms taken from everyday objects which may be reminiscent of that particular feature. This pictorial review introduces known signature patterns of distinguishing features in musculoskeletal ultrasound in a normal or abnormal condition, and may stir the beginners' interest to play a treasure-hunt game among unfamiliar images within a boundless ocean.
Go to :

Keywords: Anatomic landmarks, Anisotropy, Education, Interventional ultrasonography, Musculoskeletal system, Peripheral nerves, Tendons, Terminology, Ultrasonic imaging
INTRODUCTION
Basically, ultrasonic imaging provides a boring two-dimensional black and white screen in an age of colorful virtual reality video games. What is worse, in a freeze-frame it is difficult for anyone other than the examiner to decipher targeted structures without the expression of direction and adjacent structures. Fortunately, skilled experts in musculoskeletal ultrasound have tried to express certain distinguishing features, in a normal or abnormal condition, using terms taken from everyday objects which may be reminiscent of that particular feature. These distinguishing features of the structures in ultrasound are utilized as targets for educational purposes in both diagnosis and treatment.
It is essential to weigh the pros and cons when an interventional treatment is performed under the fluoroscope and/or ultrasound. The fluoroscope provides clearly visible joint spaces and bony structures, and confirmation of the needle inside these structures using contrast medium. However, if there are major vessels or internal organs in the path of needle approach, ultrasound definitely reduces the risk of piercing or damaging these structures.
The musculoskeletal system includes the spine and the 4 extremities. The spine is divided into the cervical, thoracic, lumbar vertebrae, sacrum, and coccyx. The upper extremities include the shoulder, elbow, and wrist joints; the lower extremities consist of the hip, knee, and ankle joints.
This pictorial review introduces known distinguishing features from common tissues, such as the nerves, muscles, tendons, and ligaments, to each specific organ, such the spine and the 4 extremities.
Go to :

MAIN BODY
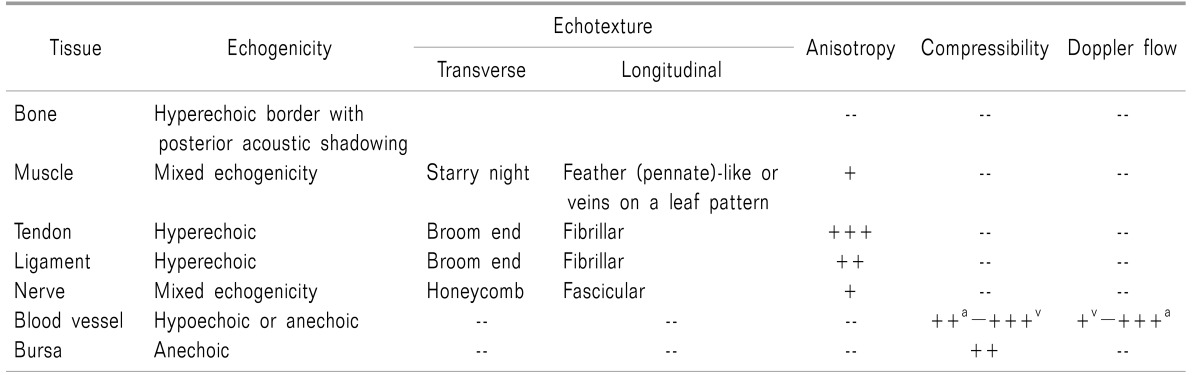
The musculoskeletal system is basically composed of the bones, joints, muscles, tendons, and ligament, as well as nerves with blood vessels. Where bone meets bone, a joint is formed. Where the muscle attaches to the bone for contraction and relaxation, it modifies into the tendon. The ligament maintains the connections between or among the bones. In addition, bursas provide a lubricated cushion at points of friction between the bone and the surrounding soft tissues, such as the skin, muscles, ligaments, or tendons. The nerves take part in the sensory, and motor innervation with the reflexes of these structures, while the blood vessels supply nutrition and extract waste.
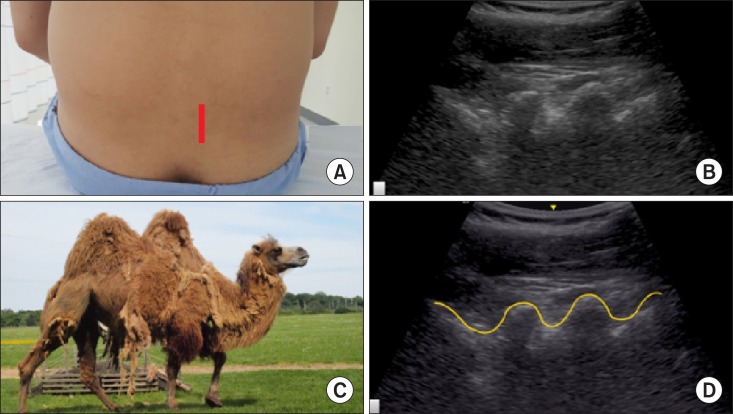
These tissues in musculoskeletal ultrasonography are described by their echogenicity, echotexture, degree of anisotropy, compressibility, or the presence of blood flow on Doppler examination (
Table 1) [
1].
Table 1
Ultrasonographic Features of Normal Tissues in the Musculoskeletal System

1. Bone and periosteum
The bony cortex demonstrates a smooth, continuous hyperechoic line with
posterior acoustic shadowing deep to the interface, because the entire sound beam is reflected and cannot penetrate beyond the bone [
1]. In addition, identification of marginal erosion and synovial inclusions in rheumatoid disorders is superior to conventional radiography.
Ultrasonic guidance can reduce time and effort in identifying the supraorbital, infraorbital, and mental foramen in the facial bone and suprascapular notch or foramen, in comparison to fluoroscopic guidance.
The periosteum is not visualized by ultrasound in normal situations. However, a thin hyperechoic line running parallel with the cortical bone is demonstrated in cases of damage to the cortex, periosseous soft tissues, and periosteum, which is called a
periosteal reaction [
2].
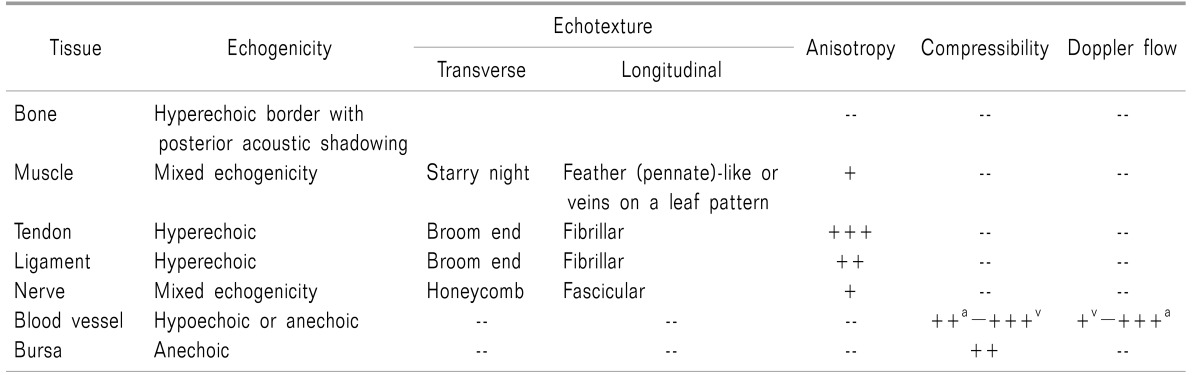
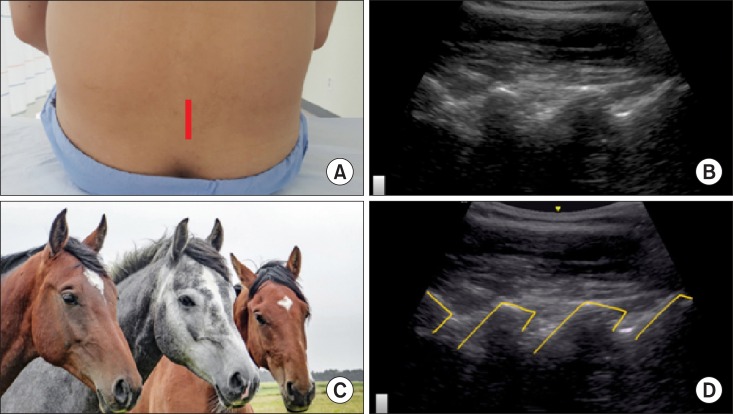
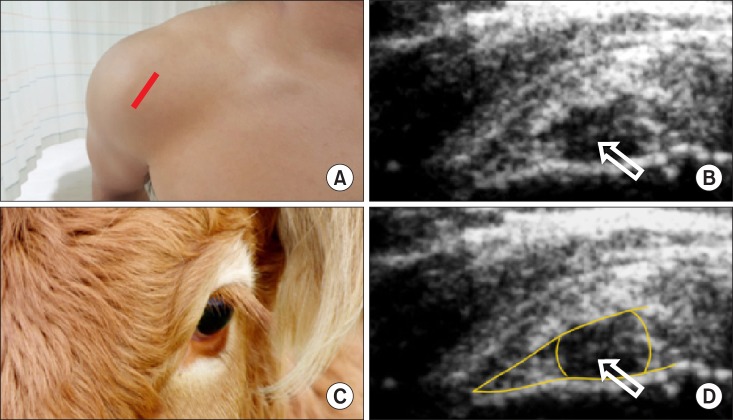
A paramedian sagittal sonogram of the lumbar spine demonstrates a "
horse head sign" under the lamina (
Fig. 1) [
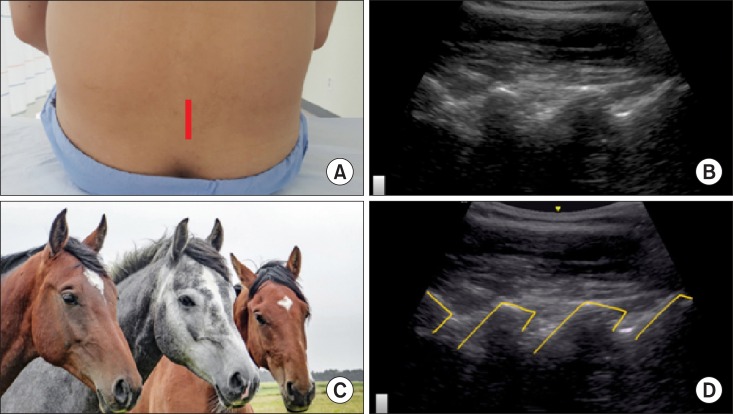
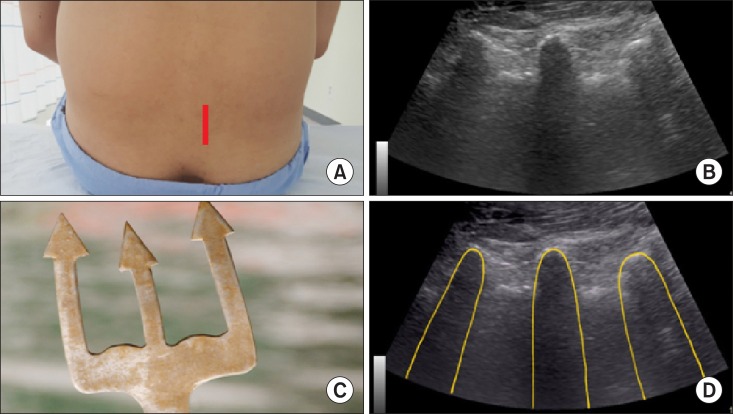
3]. If the probe is placed over the transverse processes in a paramedian sagittal process view, the transverse processes between the psoas muscle appear as hyperechoic curvilinear structures with finger-like acoustic shadowing beneath, a "
trident sign" (
Fig. 2) [
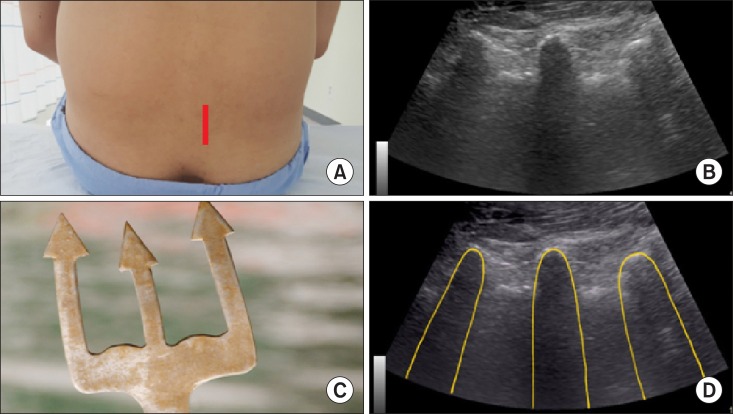
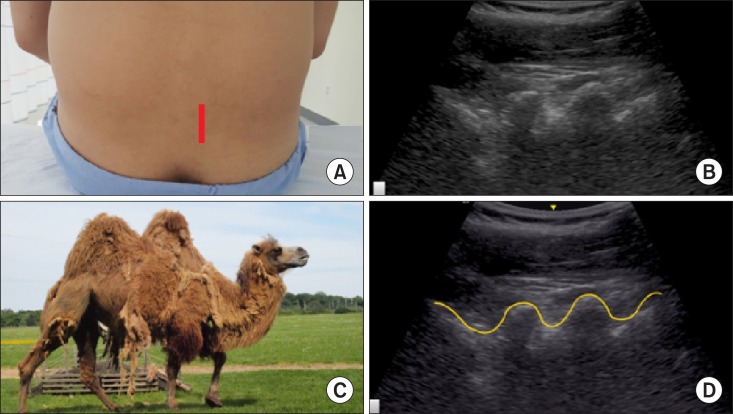
4]. In the lumbar paramedian sagittal view, the articular process may demonstrate a "
camel-hump-like appearance" (
Fig. 3) [
3].
 | Fig. 1A horse head sign of the lamina of the lumbar spine in a paramedian sagittal view. The lamina of the spine and its posterior acoustic shadow appear as a horse head in a paramedian sagittal view. (A) Probe location, (B) a paramedian sagittal ultrasonographic view, (C) a horse head, (D) a graphic overlay for (B).
|
 | Fig. 2A trident sign of the 3 consecutive transverse processes of the lumbar spine in a paramedian sagittal ultrasonographic view. The 3 consecutive transverse processes resemble as a trident, composed of hyperechoic curvilinear structures with finger-like acoustic shadowing beneath in a paramedian sagittal ultrasonographic view. (A) Probe location, (B) a paramedian sagittal ultrasonographic view, (C) a trident head, (D) a graphic overlay for (B).
|
 | Fig. 3A camel-hump sign of the lumbar articular process in a lumbar paramedian sagittal view. The superior and inferior articular processes resemble as a camel hump. (A) Probe location, (B) a paramedian sagittal ultrasonographic view, (C) a camel-hump, (D) a graphic overlay for (B).
|
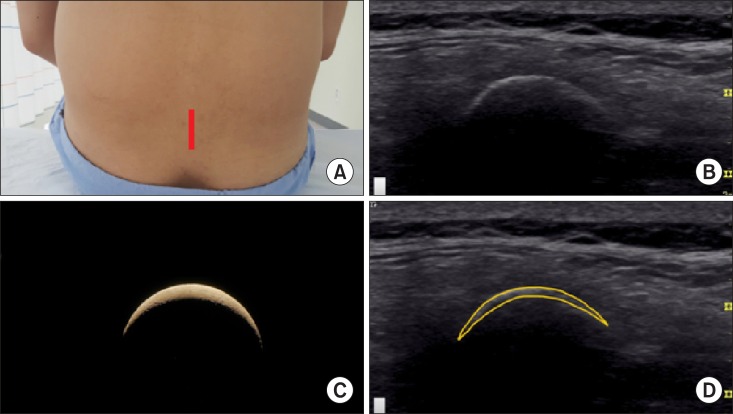
A sagittal ultrasound image of a lumbar midline dorsal spinous process appears as a typical "
crescent" shape with posterior acoustic shadowing (
Fig. 4) [
5].
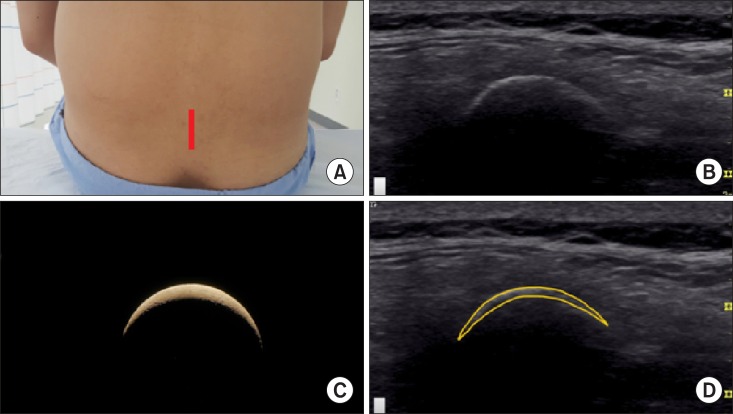 | Fig. 4A crescent sign of the lumbar midline dorsal spinous process in a median sagittal view. A lumbar midline dorsal spinous process with posterior acoustic shadowing appears as a crescent in a midline sagittal ultrasonographic view. (A) Probe location, (B) a midline sagittal ultrasonographic view, (C) a crescent, (D) a graphic overlay for (B).
|
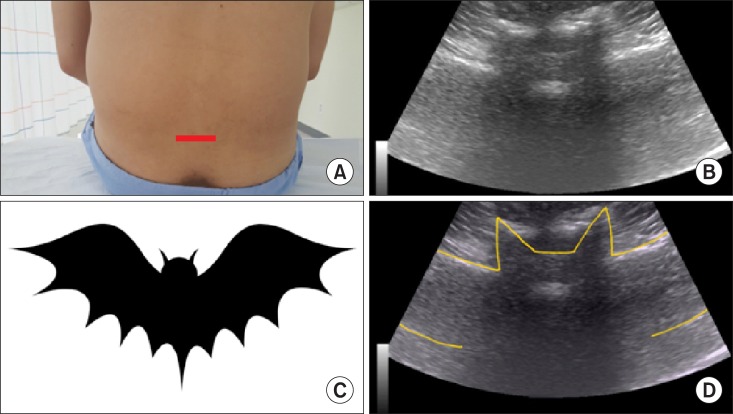
A midline transverse interlaminar view appears as a "
flying bat", which is composed of both the transverse processes and the articular processes of the facet joints with the posterior (the ligament flavum and dura mater) and anterior (the dura mater, posterior longitudinal ligament, and vertebral body) complexes of the vertebral body (
Fig. 5) [
6].
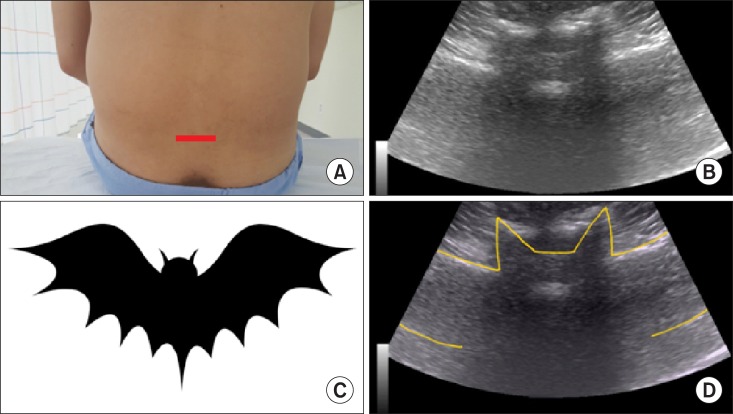 | Fig. 5A flying bat in a transverse midline interlaminar view. A flying bat in a midline transverse interlaminar view consists of both the transverse processes (wings) and the articular processes of the facet joints (ears) with the posterior (head; the ligament flavum and dura mater) and anterior (eyes; the dura mater, posterior longitudinal ligament, and vertebral body) complexes of the vertebral body. (A) Probe location, (B) a midline transverse ultrasonographic view, (C) a flying bat, (D) a graphic overlay for (B).
|
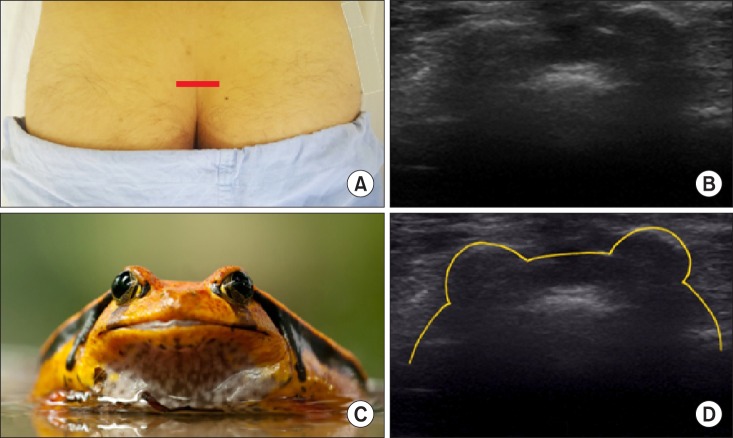
The two sacral cornua (2 hyperechoic reversed U-shaped structures with posterior acoustic shadowing) and the posterior surface of the sacrum in a transverse ultrasonographic view resemble a "
frog eyes sign" (
Fig. 6) [
6].
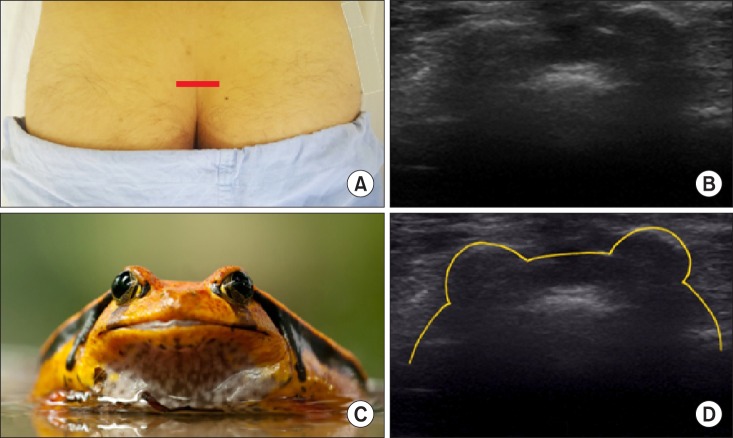 | Fig. 6Frog eyes sign of the 2 sacral cornua in a transverse view. The 2 sacral cornua above the sacral hiatus in a transverse ultrasonographic view appear as hyperechoic reversed U-shaped structures with acoustic shadowing, a frog eye sign, with the posterior surface of the sacrum. (A) Probe location, (B) a transverse ultrasonographic view, (C) a frog eye, (D) a graphic overlay for (B).
|
2. Joint and bursa
A typical synovial joint is basically composed of the articular cartilage, inner synovial fluid with synovial membrane, and outer fibrous membrane, continuing with the periosteum of the articulating bones. Therefore, a normal healthy joint on ultrasound demonstrates uniform bone profile, homogenous echogenicity of the periarticular soft tissues, and the potential minimal amounts of fluid in the joint recess or bursae. Hyaline cartilage appears as a well-defined anechoic or homogeneously hypoechoic band between the chondrosynovial and osteochondral margins in the shoulder, elbow, wrist, metacarpophalangeal, knee, and tibiotalar joints.
In an osteoarthritic joint, pathologic findings demonstrate a loss of the sharp contour of the cartilage, variations in the echogenicity of the cartilage matrix, and eventually an asymmetric narrowing of the cartilaginous layer. The bony changes in osteoarthritis range from a
hyperechoic signal in the attachment site of the joint capsule, to the bony cartilaginous margin, to evident osteophytes [
7].
Simple synovial effusions are
anechoic, however, debris within a joint effusion may represent pus, blood clots, fat lobules, or osteochondral fragments. A degenerated meniscus appears swollen with
decreased echogenicity [
8].
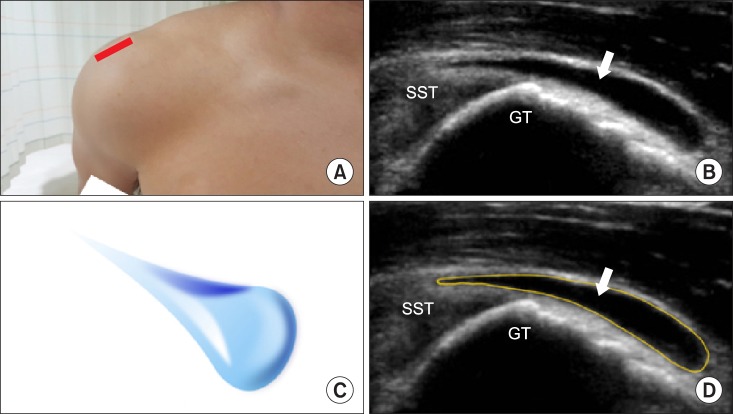
The normal bursa should not be more than 2 mm. An abnormal subacromial-subdeltoid bursa is recognized as a "
teardrop-shaped structure" with the most distended segment of the bursa most distal and most dependent (
Fig. 7) [
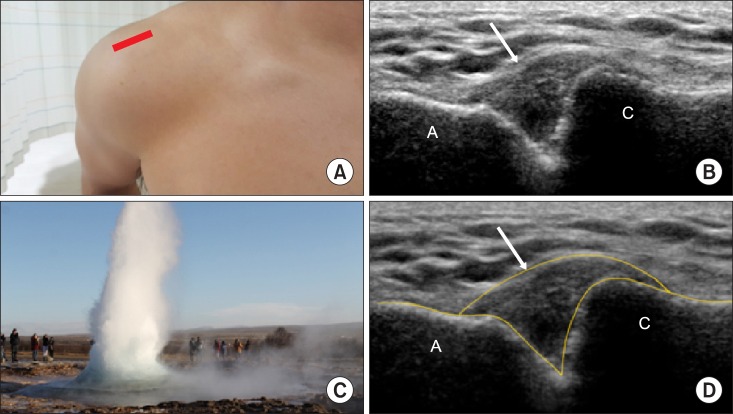
9]. A cyst or ganglion projecting superiorly from the acromioclavicular joint may present in rotator cuff tears when fluid from the subdeltoid bursa extends through the joint, the "
geyser" sign (
Fig. 8) [
10].
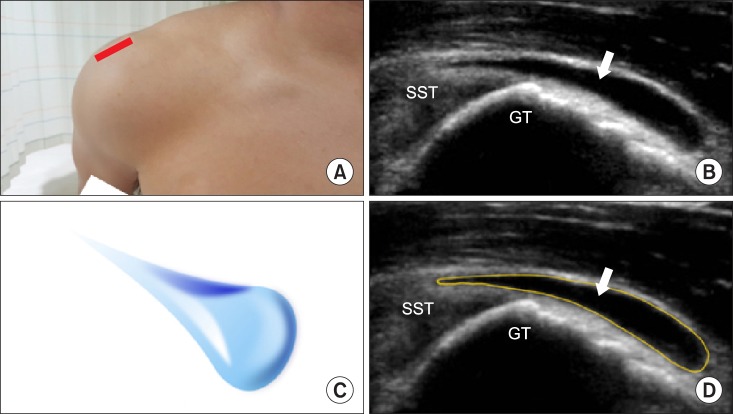 | Fig. 7A teardrop sign of the distended subacromial-subdeltoid bursa in a longitudinal view of the supraspinatus tendon. An abnormal subacromial-subdeltoid bursa with the most distended segment of the bursa most distal and most dependent may be shown as a teardrop in a transverse ultrasonographic view. (A) Probe location, (B) in a longitudinal view of the supraspinatus tendon, (C) a teardrop, (D) a graphic overlay for (B). Modified from Lew HL, Chen CP, Wang TG, Chew KT. Introduction to musculoskeletal diagnostic ultrasound: examination of the upper limb. Am J Phys Med Rehabil 2007; 86: 310-21.
|
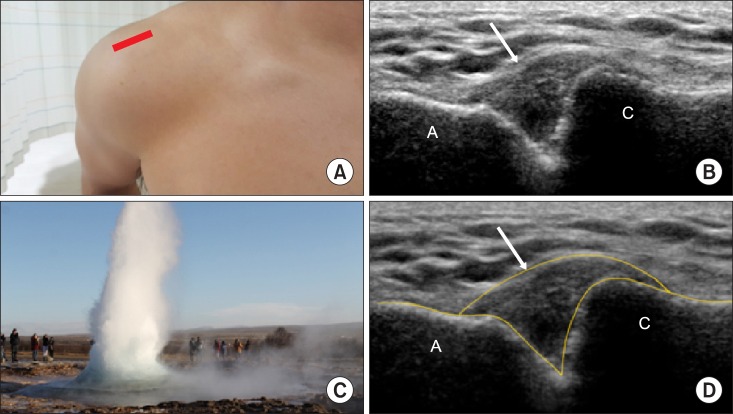 | Fig. 8A geyser sign of the cyst or ganglion projecting superiorly in a coronal across the acromioclavicular joint. It may present in rotator cuff tears. (A) Probe location, (B) a coronal across the acromioclavicular joint, (C) a teardrop, (D) a graphic overlay for (B). Modified from Beggs I. Shoulder ultrasound. Semin Ultrasound CT MR 2011; 32: 101-13.
|
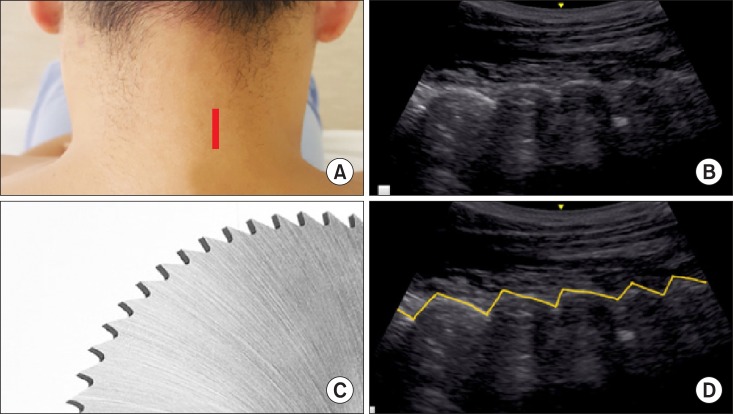
The hyperechoic articular processes of the cervical facet joints in a paramedian sagittal ultrasonographic view resemble "
saw teeth" in between the anechoic facet joint space (
Fig. 9) [
11].
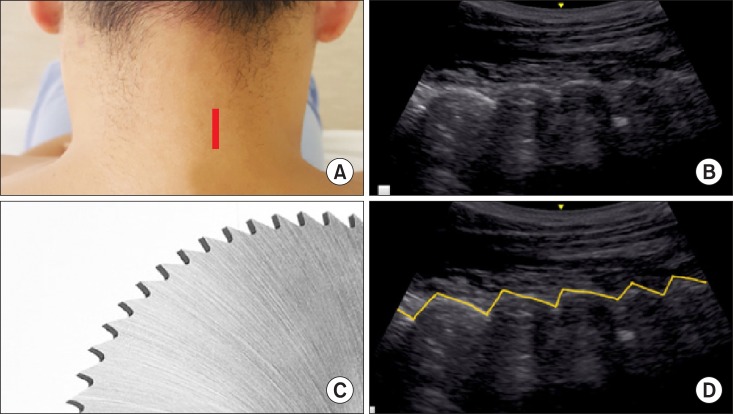 | Fig. 9A saw teeth sign of the cervical facet joints in a paramedian sagittal ultrasonographic view. The hyperechoic articular processes of the cervical facet joints in a sagittal ultrasonographic view resemble saw teeth in between the anechoic facet joint space. (A) Probe location, (B) a paramedian sagittal ultrasonographic view, (C) saw teeth, (D) a graphic overlay for (B).
|
3. Muscle
The skeletal muscle cells (fibers) are subsequently enveloped by the endomysium, fascicle, perimysium, epimysium, and fascia. The mixed echogenicity of muscle arises from the regular pattern of hypoechoic muscle fascicles within the hyperechoic perimysium and epimysium.
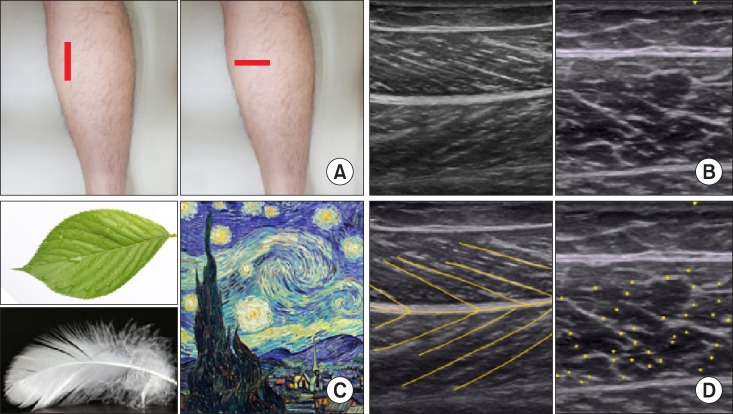
Longitudinally, muscle demonstrates a "
feather (uni-, bi-, or circum-pennate)" or "
veins on a leaf" pattern, whereas transversely they appear as a "
starry night" pattern, illustrated by post-impressionist painter Vincent van Gogh (
Fig. 10) [
112].
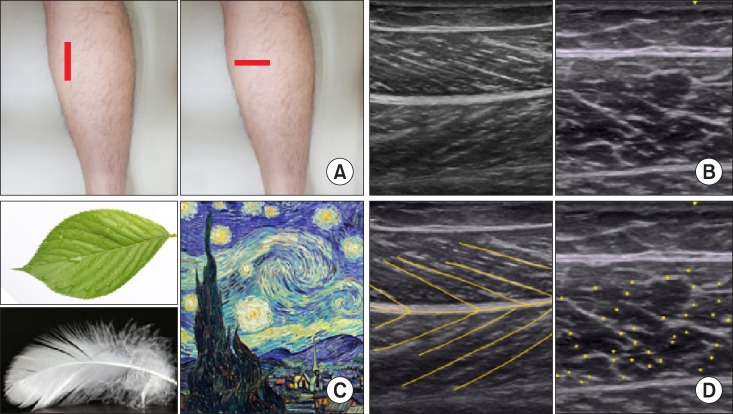 | Fig. 10A feather or veins on a leaf sign of the muscle in a longitudinal view and a starry night in a transverse ultrasonographic view in a medial gastrocnemius. The mixed echogenicity of muscle arises from the regular pattern of hypoechoic muscle fascicles within the hyperechoic perimysium and epimysium. (A) Probe location, (B) a longitudinal and transverse ultrasonographic view, (C) a feather or veins on a leaf and a starry night, (D) a graphic overlay for (B).
|
The muscle fascia is a band of collagenous connective tissue, which interpenetrates and surrounds the muscle, and inserts on the bone.
4. Tendon
A normal tendon in an ultrasonic examination demonstrates a hyperechoic linear band with fibrillar echotexture on longitudinal view. The collagen fibers are hyperechoic, separated by hypoechoic surrounding connective tissue. The characteristic anisotropy of the tendon means an unequal echogenicity along with the direction of the ultrasound beams of the ultrasonic probe.
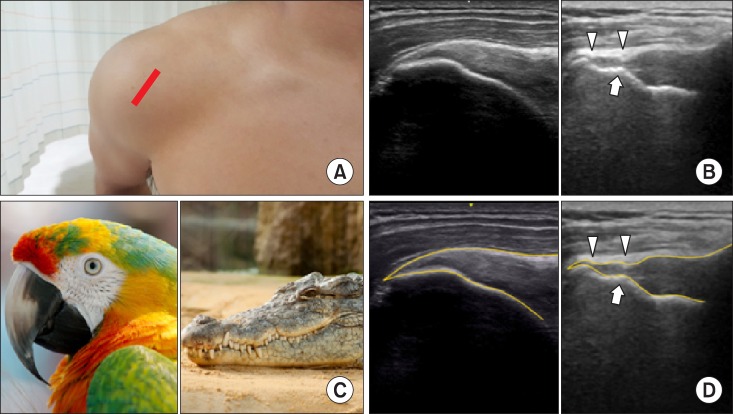
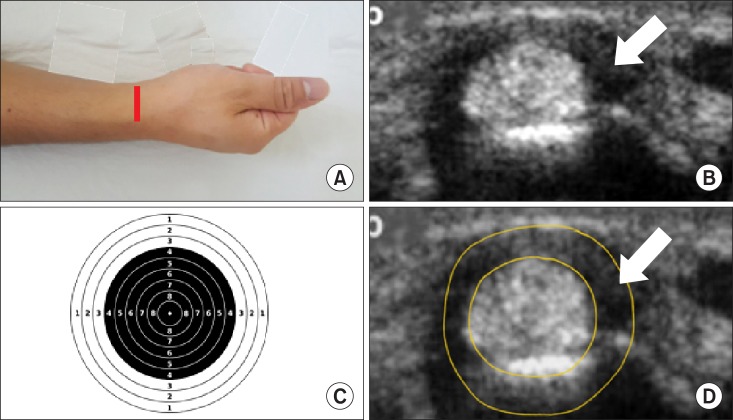
The supraspinatus muscle of the shoulder, a rotator cuff, originates from the supraspinous fossa of the scapula and inserts into the greater tubercle of the humerus below the acromion. A normal distal tendon of the supraspinatus attaching to the greater tubercle of the humerus demonstrates a "
bird's (parrot's) beak" while maintaining its thickness and convexity in a lateral coronal view. If the thickness and convexity of the distal tendon is lost due to rupture, it resembles a broken bird's beak. When a cortical irregularity on the greater tubercle coexists with a ruptured distal supraspinatus tendon, it resembles a "
crocodile's mouth" (
Fig. 11) [
1314]. In addition, Rim rent tears, involving a small, articular surface avulsion adjacent tuberosity, appear as a small, hypoechoic defect with a central hyperechoic line on the articular surface. The transverse view appears as a "
bull's eye" lesion, with a central punctate echo surrounded by a hypoechoic halo of fluid or an edematous lesion (
Fig. 12) [
14].
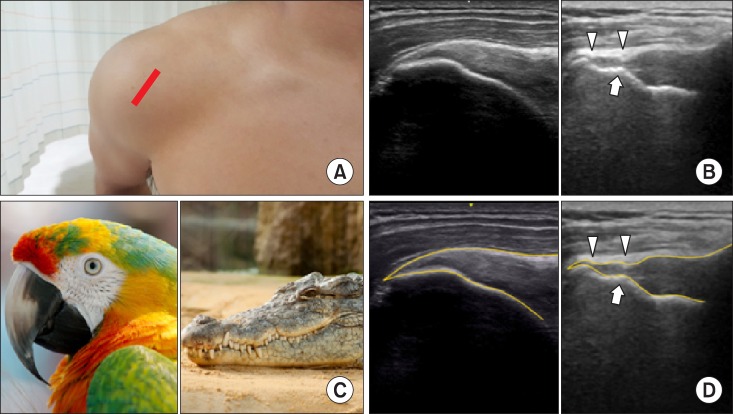 | Fig. 11A bird's (parrot's) beak in a normal supraspinous tendon attaching to the greater tubercle of the humerus and a crocodile's mouth in a ruptured supraspinous tendon coexisting with a cortical irregularity on the greater tubercle in a longitudinal view. (A) Probe location, (B) a longitudinal ultrasonographic view, (C) a bird's (parrot's) beak and a crocodile's mouth (D) graphic overlays for (B).
|
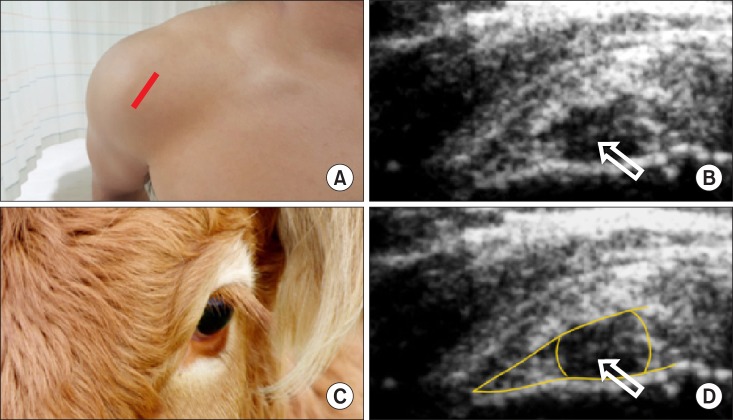 | Fig. 12A bull's sign of the rim rent tears of supraspinatus tendon in a transverse ultrasonographic view. Rim rent tears of the supraspinatus tendon, involving a small, articular surface avulsion adjacent tuberosity, appear as a small, hypoechoic defect with a central hyperechoic line on the articular surface. (A) Probe location, (B) a transverse ultrasonographic view, (C) a bull's sign, (D) a graphic overlay for (B). Modified from Lew HL, Chen CP, Wang TG, Chew KT. Introduction to musculoskeletal diagnostic ultrasound: examination of the upper limb. Am J Phys Med Rehabil 2007; 86: 310-21.
|
A transverse sonogram appears as a "
target" sign (peri-tendineal effusion) in de Quervain tenosynovitis, which demonstrates a hypoechoic ring around the abductor pollicis longus and extensor pollicis brevis tendons (
Fig. 13) [
14].
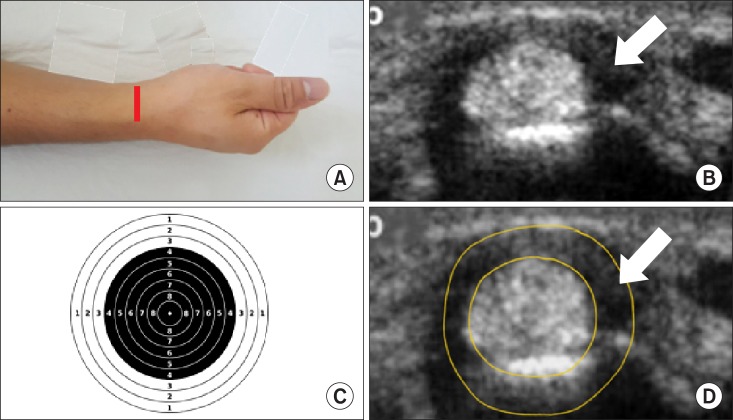 | Fig. 13A target sign of de Quervain tenosynovitis in a transverse ultrasonographic view. Peri-tendineal effusion in de Quervain tenosynovitis demonstrates a hypoechoic ring around the abductor pollicis longus and extensor pollicis brevis tendons. (A) Probe location, (B) a transverse ultrasonographic view, (C) a target sign, (D) a graphic overlay for (B). Modified from Lew HL, Chen CP, Wang TG, Chew KT. Introduction to musculoskeletal diagnostic ultrasound: examination of the upper limb. Am J Phys Med Rehabil 2007; 86: 310-21.
|
5. Ligament
A normal ligament demonstrates a hyperechoic linear structure, just like a tendon, however, it shows a more compact fibrillar echotexture, composed of dense connective tissue. The connective tissue consists of various amounts of collagen, elastin, and fibrocartilage, therefore, it demonstrates a more variable appearance than a tendon [
2].
6. Peripheral nerve
The myelinated or unmyelinated axons (nerve fibers) transmit information either from the periphery to the central nervous system or in the opposite direction. These axons are encapsulated with the endoneurium, perineurium, and epineurium, sequentially.
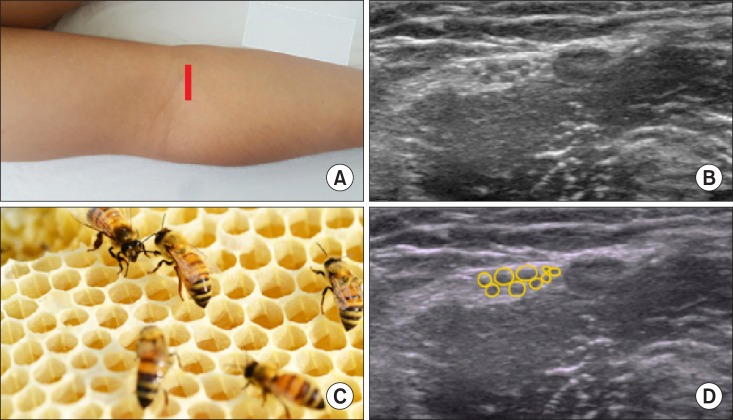
On longitudinal ultrasound views, the peripheral nerves appear as parallel hyperechoic lines with hypoechoic separations between them. They are similar to tendons, but less echogenic (hypoechoic). On transverse views, individual peripheral nerve fibers and their fibrous matrix present with multiple, punctate echogenicity within an ovoid, well-defined nerve sheath [
2]. A multifascicular pattern displays a black-and-white speckled ("
honeycomb") image (
Fig. 14), whereas an oligofascicular pattern is visualized as a more solid, oval, and black structure [
151617181920].
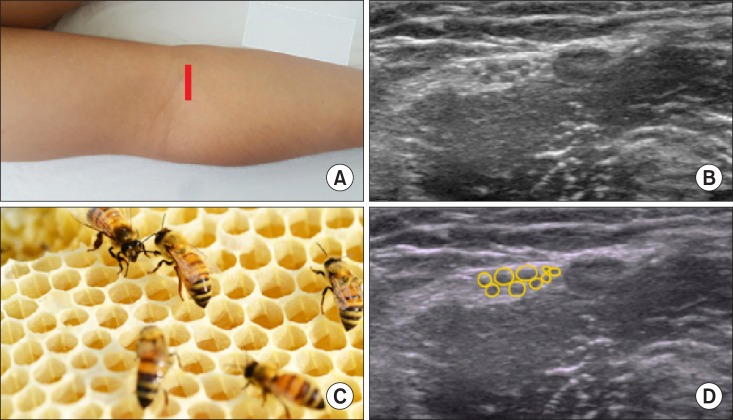 | Fig. 14A honeycomb sign of the peripheral nerve plexus in a transverse ultrasonographic view. (A) Probe location, (B) a transverse ultrasonographic view, (C) a honeycomb sign, (D) a graphic overlay for (B).
|
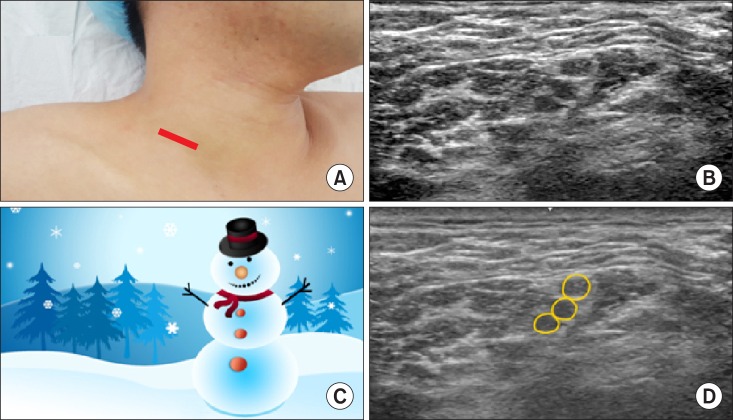
On a transverse view of the C5, C6, and C7 nerve roots with an interscalene approach for a brachial plexus block, the roots of C5, C6, and C7 appear to be sitting on top of each other in a "
snowman" appearance (
Fig. 15) [
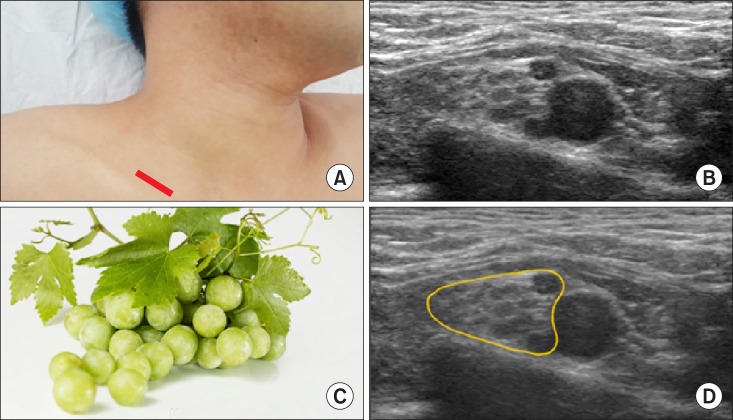
21]. On a transverse oblique plane, the subclavian and adjacent hyperechoic plexus appears like a "
cluster of grapes" (
Fig. 16) [
21].
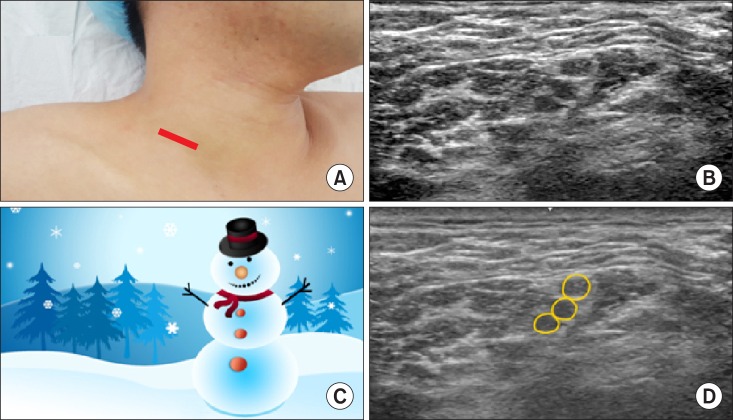 | Fig. 15A snowman sign of the consecutive nerve roots in a transverse ultrasonographic view. The C5, C6, and C7 nerve roots with an interscalene approach appear as a snowman. (A) Probe location, (B) a transverse ultrasonographic view, (C) a snowman sign, (D) a graphic overlay for (B).
|
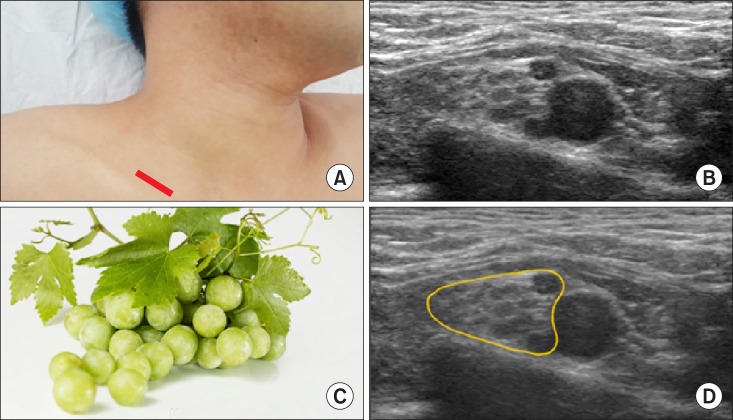 | Fig. 16A cluster of grapes sign of the subclavian and adjacent hyperechoic plexus in a transverse oblique view. (A) Probe location, (B) a transverse oblique view, (C) a cluster of grapes sign, (D) a graphic overlay for (B).
|
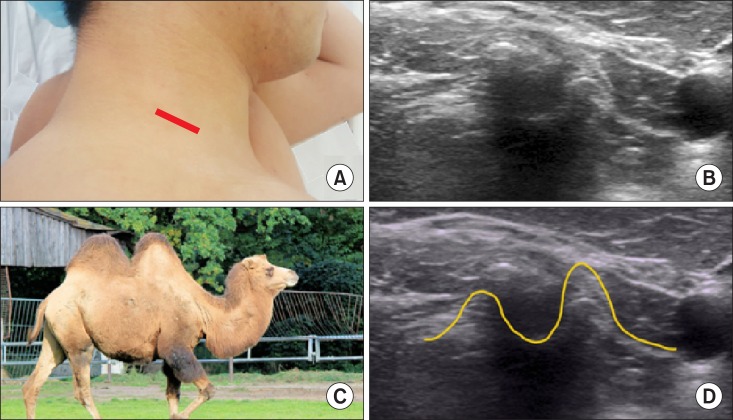
When performing a selective nerve root block for the C5 in a short transverse ultrasonographic image, the nerve root is located between the bigger anterior and smaller posterior tubercle of the C5 transverse process, which resembles as a "
2-humped camel" (
Fig. 17) [
6].
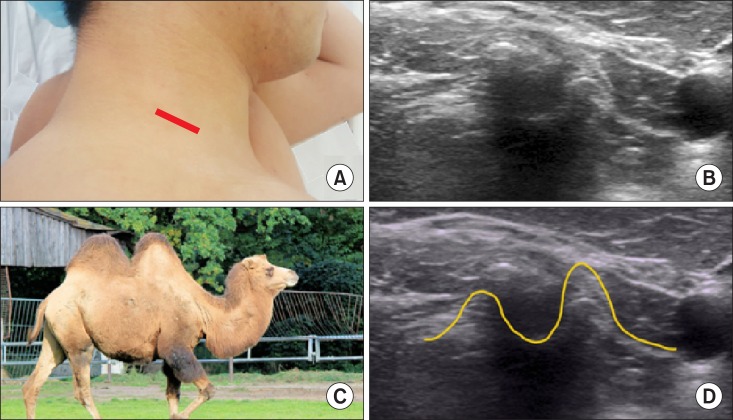 | Fig. 17A 2-humped camel sign of the bigger anterior and smaller posterior tubercle of the cervical transverse process in order to perform a selective nerve root block. (A) Probe location, (B) a transverse view, (C) a 2-humped camel sign, (D) a graphic overlay for (B).
|
Go to :

CONCLUSIONS
At first, beginners in an age of colorful virtual reality video games may tire of musculoskeletal ultrasound filled with a 2-dimensional, flat, black-and-white screen. However, finding signature patterns of distinguishing features in the normal anatomic or abnormal pathologic tissue of the musculoskeletal system may be an attractive proposal, similar to solving a picture puzzle. Therefore, this pictorial review of signature patterns which may be recognized in musculoskeletal ultrasonography may provide information and interest about the various known animals and objects which lurk within the musculoskeletal system, not unlike the movie "Night at the Museum".
Go to :

ACKNOWLEDGEMENTS
We really thank Dr. Nam, M.D., the husband of one of the authors, for being a good model for the musculoskeletal ultrasound.
Go to :

References
1. Smith J, Finnoff JT. Diagnostic and interventional musculoskeletal ultrasound: part 2. Clinical applications. PM R. 2009; 1:162–177. PMID:
19627890.

2. Moore RE. 2010 musculoskeletal ultrasound for the extremities: a practical guide to sonography of the extremities. Scotts Valley (CA): Createspace;2010. p. 9–11.
3. Karmakar MK, Li X, Kwok WH, Ho AM, Ngan Kee WD. Sonoanatomy relevant for ultrasound-guided central neuraxial blocks via the paramedian approach in the lumbar region. Br J Radiol. 2012; 85:e262–e269. PMID:
22010025.

4. Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiology. 2011; 114:1459–1485. PMID:
21422997.

5. Nomura JT, Leech SJ, Shenbagamurthi S, Sierzenski PR, O'Connor RE, Bollinger M, et al. A randomized controlled trial of ultrasound-assisted lumbar puncture. J Ultrasound Med. 2007; 26:1341–1348. PMID:
17901137.

6. Karmakar MK. Ultrasound-guided central neuraxial blocks. In : Narouze SN, editor. Atlas of ultrasound-guided procedures in interventional pain management. New York (NY): Springer;2011. p. 161–178.
7. Möller I, Bong D, Naredo E, Filippucci E, Carrasco I, Moragues C, et al. Ultrasound in the study and monitoring of osteoarthritis. Osteoarthritis Cartilage. 2008; 16(Suppl 3):S4–S7. PMID:
18760636.

8. Razek AA, Fouda NS, Elmetwaley N, Elbogdady E. Sonography of the knee joint. J Ultrasound. 2009; 12:53–60. PMID:
23397073.

9. van Holsbeeck M, Strouse PJ. Sonography of the shoulder: evaluation of the subacromial-subdeltoid bursa. AJR Am J Roentgenol. 1993; 160:561–564. PMID:
8430553.

10. Beggs I. Shoulder ultrasound. Semin Ultrasound CT MR. 2011; 32:101–113. PMID:
21414546.

11. Narouze S, Peng PW. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures. Part II: axial structures. Reg Anesth Pain Med. 2010; 35:386–396. PMID:
20607896.

12. Woodhouse JB, McNally EG. Ultrasound of skeletal muscle injury: an update. Semin Ultrasound CT MR. 2011; 32:91–100. PMID:
21414545.

13. Tekin L, Kara M, Ozçakar L. When the parrot's beak becomes the crocodile's mouth: a story on shoulder ultrasound. Rheumatol Int. 2013; 33:2447–2448. PMID:
22811012.

14. Lew HL, Chen CP, Wang TG, Chew KT. Introduction to musculoskeletal diagnostic ultrasound: examination of the upper limb. Am J Phys Med Rehabil. 2007; 86:310–321. PMID:
17413545.
15. van Geffen GJ, Moayeri N, Bruhn J, Scheffer GJ, Chan VW, Groen GJ. Correlation between ultrasound imaging, cross-sectional anatomy, and histology of the brachial plexus: a review. Reg Anesth Pain Med. 2009; 34:490–497. PMID:
19920425.

16. Kim YD, Yu JY, Shim J, Heo HJ, Kim H. Risk of encountering dorsal scapular and long thoracic nerves during ultrasound-guided interscalene brachial plexus block with nerve stimulator. Korean J Pain. 2016; 29:179–184. PMID:
27413483.

17. Lee MJ, Koo DJ, Choi YS, Lee KC, Kim HY. Dexamethasone or dexmedetomidine as local anesthetic adjuvants for ultrasound-guided axillary brachial plexus blocks with nerve stimulation. Korean J Pain. 2016; 29:29–33. PMID:
26839668.

18. Park SK, Sung MH, Suh HJ, Choi YS. Ultrasound guided low approach interscalene brachial plexus block for upper limb surgery. Korean J Pain. 2016; 29:18–22. PMID:
26839666.

19. Kim YH. Ultrasound phantoms to protect patients from novices. Korean J Pain. 2016; 29:73–77. PMID:
27103961.

20. Soneji N, Peng PW. Ultrasound-guided pain interventions -a review of techniques for peripheral nerves. Korean J Pain. 2013; 26:111–124. PMID:
23614071.

21. Tsui B, Suresh S. Ultrasound imaging for regional anesthesia in infants, children, and adolescents: a review of current literature and its application in the practice of extremity and trunk blocks. Anesthesiology. 2010; 112:473–492. PMID:
20068455.

Go to :





 Citation
Citation Print
Print


 XML Download
XML Download