This article has been
cited by other articles in ScienceCentral.
Abstract
Because of its anatomical location and function, the costotransverse (CTRV) joint can be a source of thoracic back pain. In this retrospective observational study, we evaluated the clinical effectiveness of the CTRV joint injection in thoracic back pain patients with suspected CTRV joint problems. We enrolled 20 thoracic back pain patients with localized tenderness that was provoked by the application of pressure on the affected CTRV joints. We injected it with 0.5 ml of a ropivacaine and triamcinolone mixture at each level. The mean pre-injection pain score decreased by 37.9% (7.2 ± 1.5 to 4.5 ± 1.7, P < 0.001) two weeks after CTRV joint injection. In addition, 70% of patients reported an excellent or good level of satisfaction. We demonstrated that an ultrasound-guided injection of the CTRV joint reduced patients' pain scores and led to a high level of satisfaction at short-term follow-ups in patients with suspected CTRV joint problems.
Go to :

Keywords: Costotransverse joint, Costovertebral joint, Intra-articular block, Sono-guided injection, Thoracic back pain, Thoracic spine
INTRODUCTION
Many potential pain generators exist in the thoracic spine, and variable clinical symptoms and the close proximity of related anatomical structures lead to poor localization of the exact pain source. Therefore, the diagnosis and treatment of thoracic back pain have been historically considered difficult for the pain physician [
1]. Thoracic facet joints and intervertebral disks are considered to be the most typical pain sources in the thoracic spine; therefore, clinical practice has focused on the assessment and treatment of these structures [
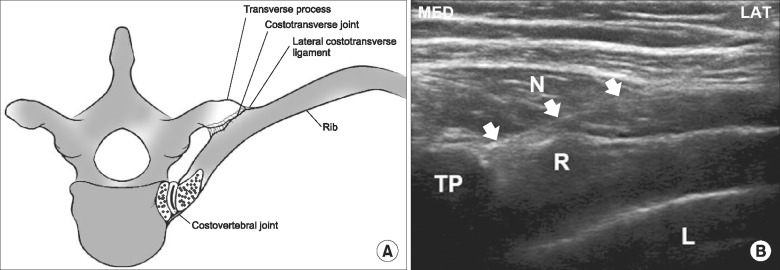
234]. The costovertebral and costotransverse (CTRV) joints are the articulations that connect the ribs with the bodies of the thoracic vertebrae and transverse processes (
Fig. 1) [
5]. The costovertebral and CTRV joints also significantly contribute to the stability and movement of the thoracic spine, which is not limited to motion of the ribs [
67]. Although the CTRV joints are relatively less studied compared to the thoracic facet joints and intervertebral disks, it has been well established that the CTRV joints may produce clinically significant thoracic back pain [
1891011]. Therefore, we hypothesized that the CTRV joints might be a source of pain and that this treatment could lead to clinical improvements. The aim of this study is to evaluate the clinical effectiveness of the CTRV joint injection in thoracic back pain patients with suspected CTRV joint problems.
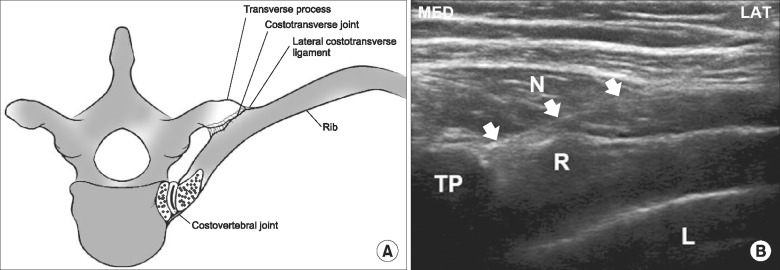 | Fig. 1(A) Rib head contact with the vertebral body via two joints. Costotransverse and costovertebral joints. (B) Ultrasound image of CTRV joint. With an in-plane approach, the needle was advanced medially toward the CTRV joint. As the needle passed under the transverse process of the target CTRV joint, it was advanced until the tip penetrated the capsule. TP: transverse process, R: rib, L: lung, N: needle.
|
Go to :

MATERIALS AND METHODS
This study is a retrospective observational audit of patients who received a CTRV joint injection for pain treatment. We reviewed clinical records and interviewed patients individually at a follow-up visit or via telephone. The study protocol was approved by the institutional review board, and written informed consent was obtained from all patients on an outpatient basis. The study population was defined as thoracic back pain patients with localized paraspinal tenderness 2-3 cm lateral to the midline where the transverse process meets the rib, at anticipated points that correspond to the CTRV joint on physical examination.
The patients were placed in the prone position during prescanning for identification of the 12th rib to investigate the thoracic level of the target CTRV joint using an ultrasound machine with a 7.5-MHz linear probe (SonoSite S-Nerve Ultrasound System, Sonosite, Bothell, WA, USA).
All ultrasound-guided CTRV joint injections were performed by one pain physician (K.B.Y.) as previously described by Deimel et al. [
10]. For image optimization, we identified the transverse process, CTRV joint, rib, and lung in the same plane (
Fig. 1). With an in-plane approach, the needle was advanced medially toward the CTRV joint. As the needle passed under the transverse process of the target CTRV joint, it was advanced until the tip penetrated the capsule (
Fig. 1). Thereafter, 0.5 ml of triamcinolone acetonide 2.5 mg and 0.75% ropivacaine mixture were injected at each CTRV joint.
Clinical and demographic data were collected for analysis, including age, gender, coexisting pain sites, duration of pain, previous pain intervention history, characteristics of thoracic back pain, and CTRV joint injection sites. Before and two weeks after CTRV joint injection, patients were asked to rate their pain score using a 10-point numeric rating scale (NRS; 0 = no pain, 10 = worst possible pain). We also assessed the degree of patient satisfaction as excellent, good, fair, or bad two weeks after injection.
Continuous data are reported as mean and standard deviation (SD) unless otherwise indicated. The normality of data distribution was assessed using the Shapiro–Wilk test. Categorical data are reported as both the number of patients and the percentage. A paired t-test was used to compare mean pain scores before and two weeks after CTRV joint injection. Statistical analyses were performed with SPSS statistical software, version 18.0 (SPSS Inc., Chicago, IL, USA). A P value < 0.05 was considered statistically significant.
Go to :

RESULTS
Twenty consecutive patients who were treated with CTRV joint injections were enrolled in this study.
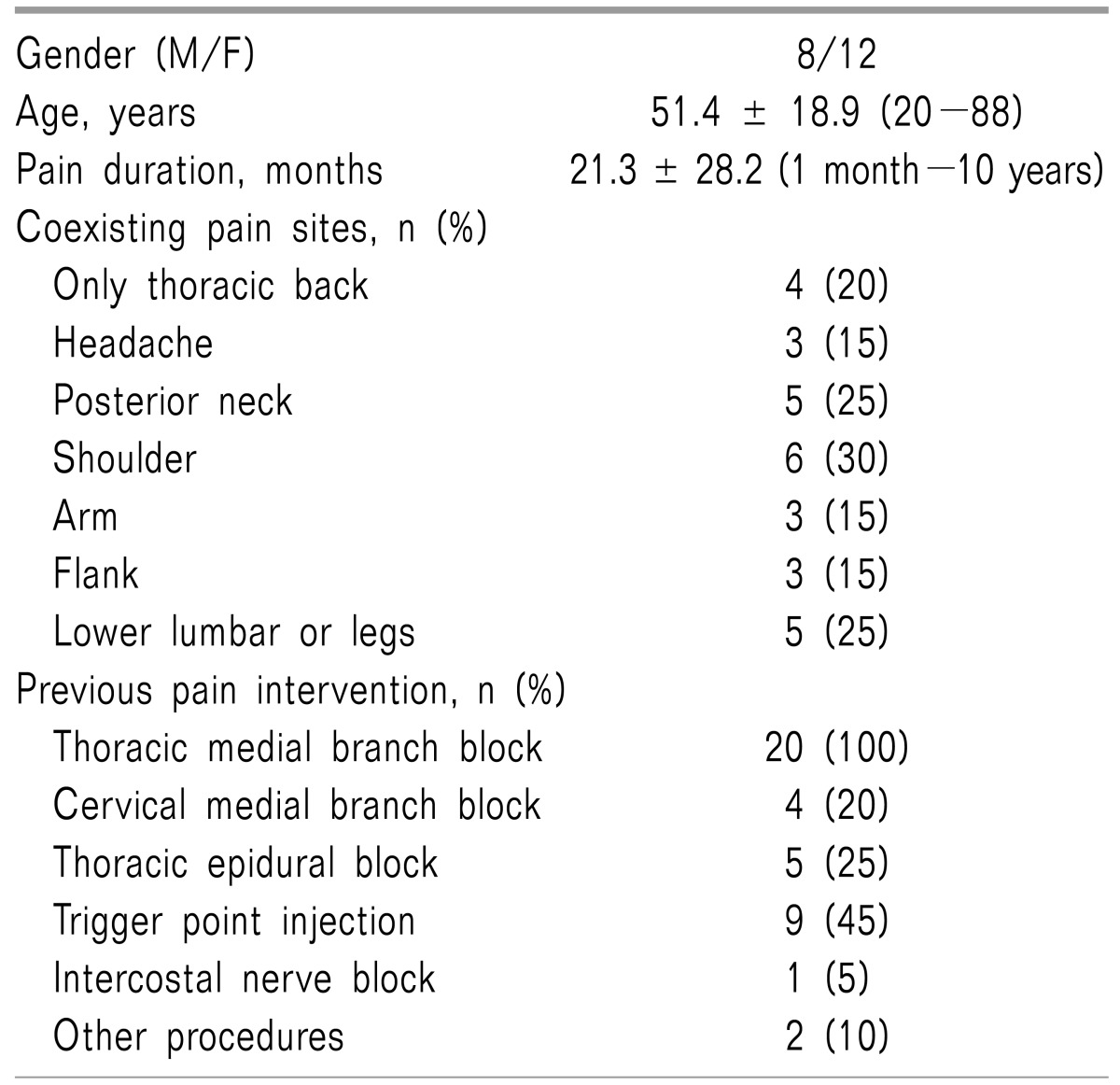
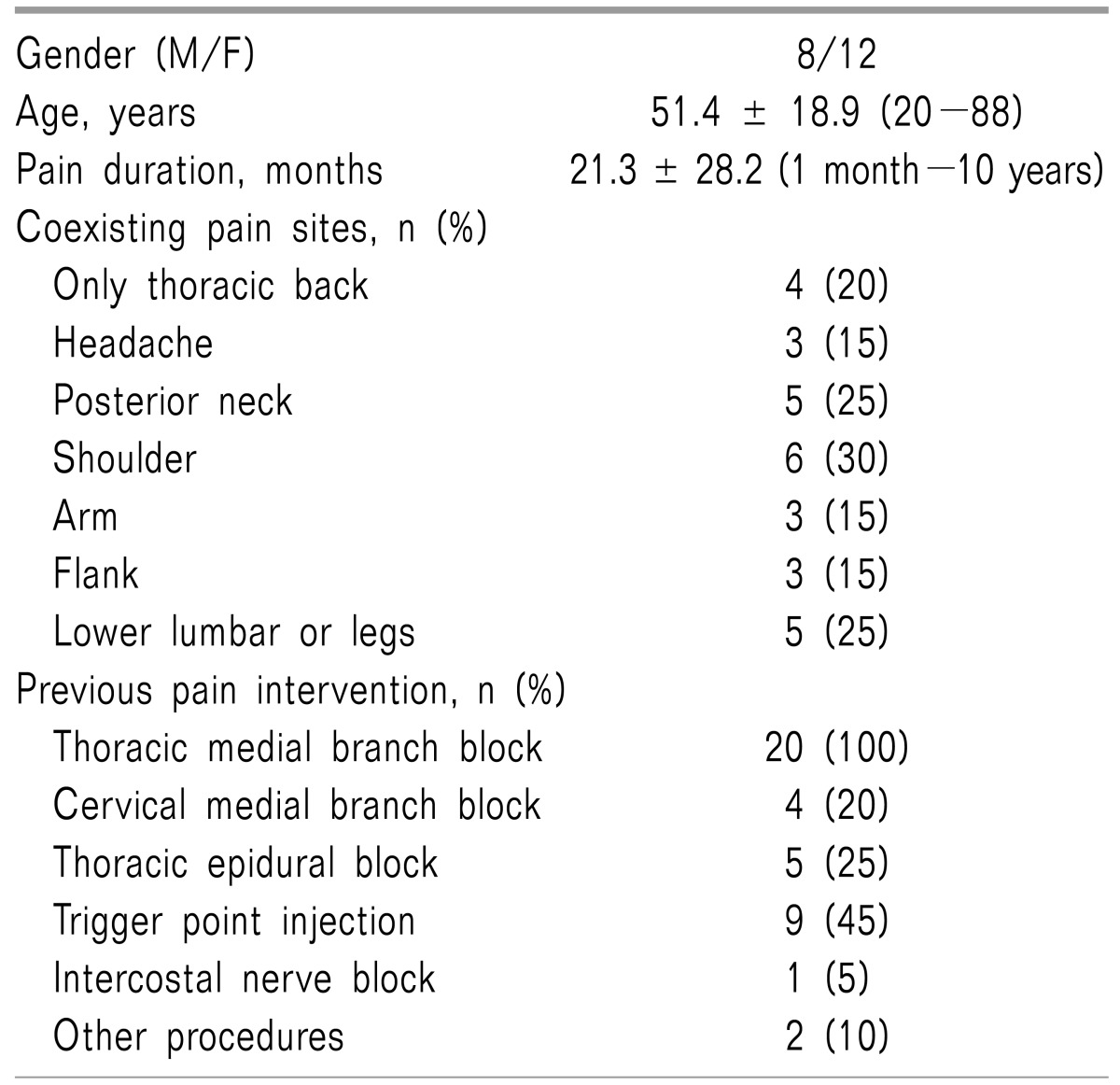
Patient characteristics and pain-related data are shown in
Table 1. Patients enrolled in this study previously experienced a variety of interventional procedures for thoracic back pain treatment. In particular, all patients had previously experienced thoracic medial branch blocks, but they reported no lasting improvement after any of these interventions.
Table 1
Patient Characteristics and Pain Profile

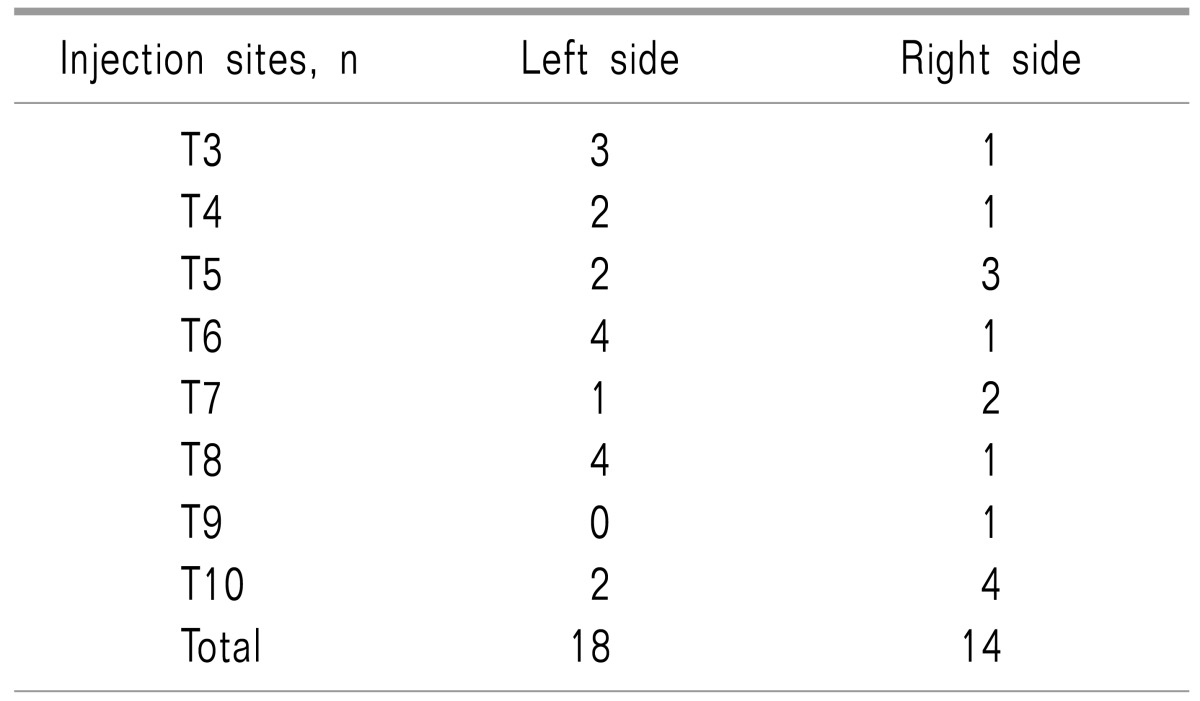
Injection sites for the CTRV joint injections are listed in
Table 2. Twenty symptomatic thoracic back pain patients received a combined total of 32 CTRV injections at the T3-T10 spine levels.
Table 2
Injection Sites for Costotransverse Joint Injections
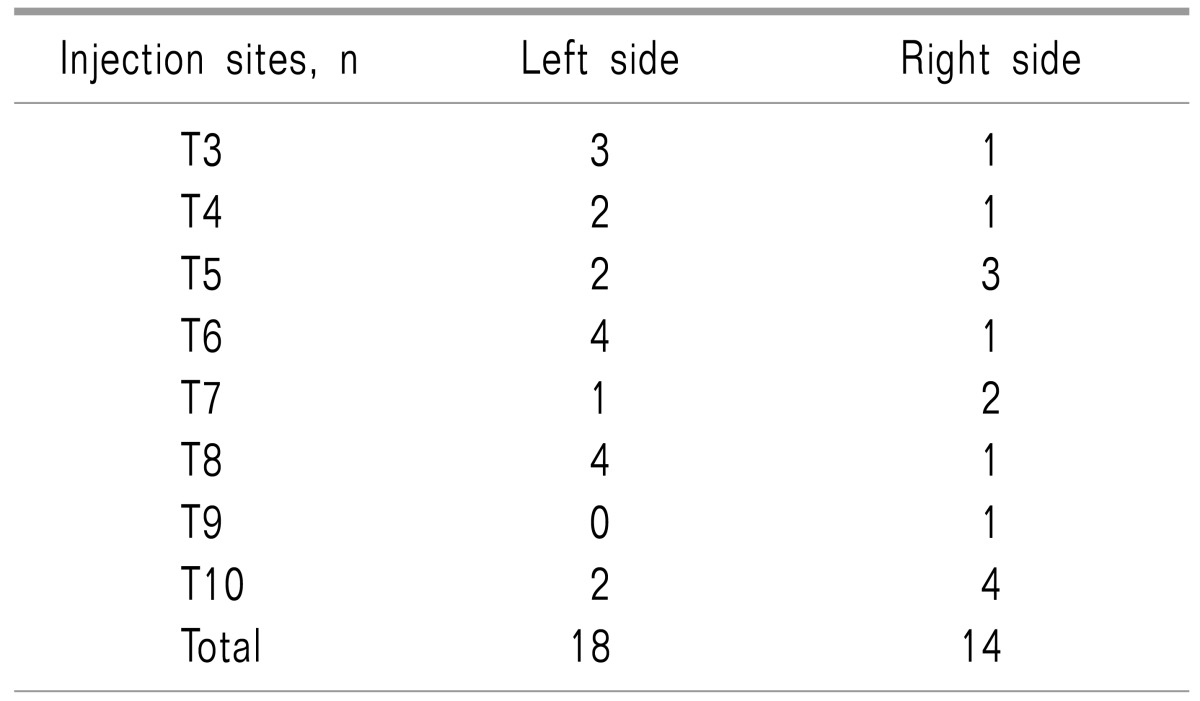

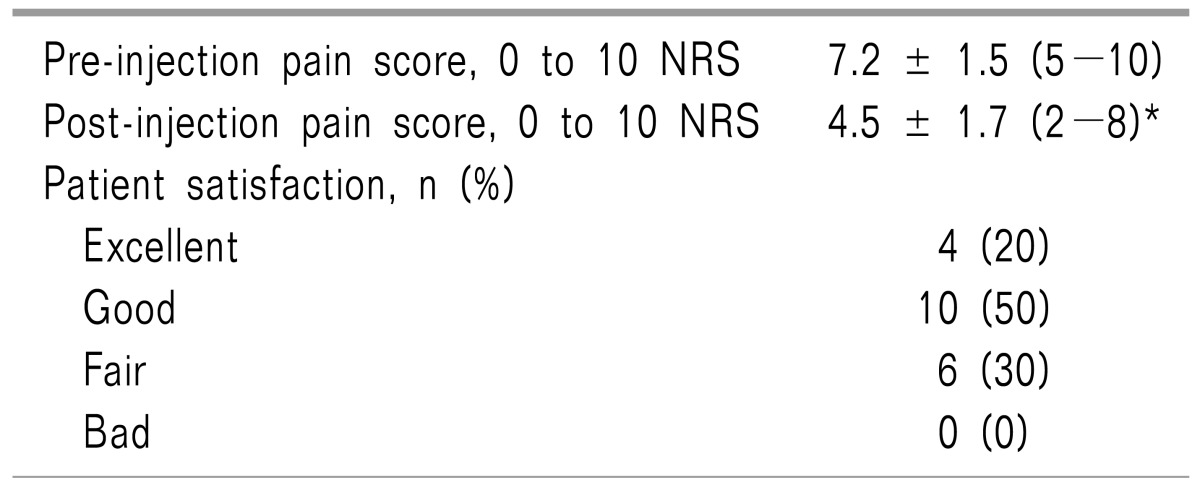
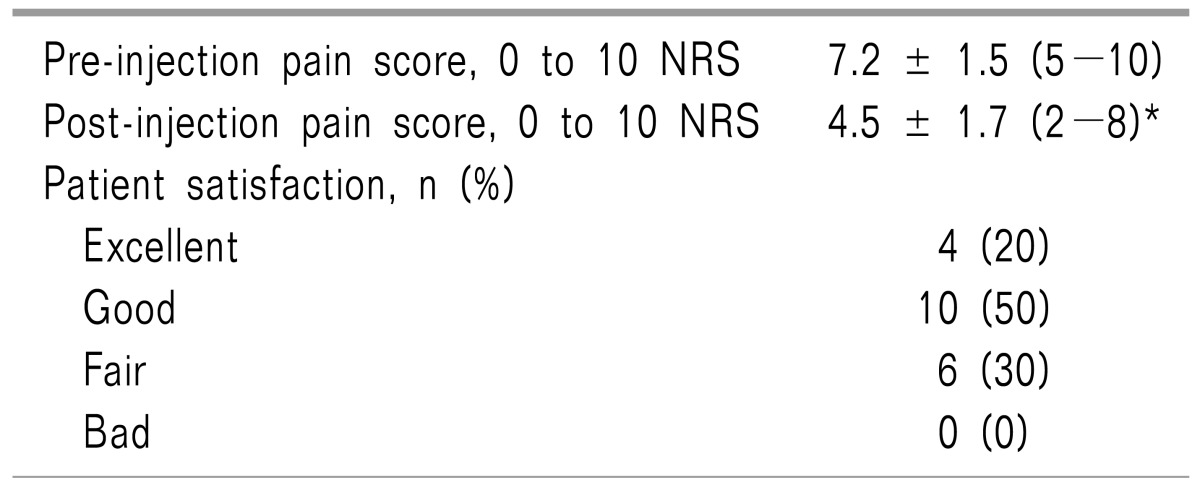
Table 3 shows the change in pain scores before and after the CTRV joint injection treatment, and the degree of patient satisfaction two weeks after the treatment. The mean pre-procedure pain score decreased by 37.9% (7.2 ± 1.5 to 4.5 ± 1.7,
P < 0.001) two weeks after CTRV joint injection. Although most patients reported reduced pain two weeks after injection, two patients reported the same pain score. In addition, 70% of patients (14/20) reported excellent or good satisfaction levels during the two weeks after the injection.
Table 3
Pain Scores before and Two Weeks after Costotransverse Joints Injection and the Degree of Patient Satisfaction Two Weeks after Injection

Go to :

DISCUSSION
This study reports the clinical outcomes of CTRV joint injection for treating CTRV joint–generated pain. We demonstrated that an ultrasound–guided CTRV joint injection with local anesthetic and steroid led to reduced pain scores and a high level of satisfaction at short-term follow-ups of thoracic back pain patients with suspected CTRV joint problems.
The provoked pain patterns of thoracic facet joints overlap considerably in the thoracic area, and no referral zone can be attributed solely to one joint [
1213]. In contrast to the thoracic facet joint, the CTRV joint pain pattern is very localized and presents with mainly unilateral symptoms which are limited to the affected CTRV joint [
19]. This pain pattern is also distinguished from referred pain caused by an active trigger point on the rhomboid or trapezius muscles [
1]. Interestingly, all patients had previously received thoracic medial branch blocks. In humans, the medial branches of the thoracic dorsal rami innervate the thoracic facet joints, whereas innervation of the CTRV joints comes from the lateral branch of the thoracic dorsal rami [
11]. Therefore, conventional thoracic medial branch interventions may not fully relieve pain originating from the CTRV joints.
Costovertebral joints, which receive sympathetic innervation, have also been known to cause thoracic back pain [
1]. However, this joint pain pattern sometimes radiates to the anterior chest area, similar to visceral-origin chest pain, which is called atypical chest pain and pseudo- angina [
114]. Some studies have demonstrated that intercostal nerve blocks effectively reduced this costovertebral joint-generated pain [
14]. Although no patients reported radiating pain to the anterior chest wall in this study, we cannot fully exclude costovertebral joint problems in some patients because the costovertebral and CTRV joints have a very close biomechanical relationship that is associated with rib movements [
67]. It is therefore difficult to differentiate which of the costovertebral or costotransverse joints is problematic with any kind of specificity on manual testing [
1]. Moreover, ultrasound guided-costovertebral joint injection is technically very difficult due to its location.
The CTRV joint is the joint formed between the facet of the tubercle of the rib and the adjacent transverse process of a thoracic vertebra [
5]. The CTRV joint is a plane-type synovial joint which allows both gliding and rotation of the connected rib [
567]. The pathophysiology of CTRV joint problems has not been completely elucidated, but in a recent histological study, immunoreactivity was confirmed for specific neuropeptides within the CTRV joint tissue samples, which suggests that the CTRV joint is generating pain [
11]. On the other hand, a partial resection model of the CTRV joint in canines demonstrated that the CTRV joint participates as a stabilizer of the thoracic spine along with the thoracic intervertebral disk and costovertebral joint [
6]. This finding suggests that CTRV joint dysfunction may affect or be affected by thoracic spine destabilization.
This study has several limitations. The small number of patients and lack of a control group impaired this study, and we did not conduct long-term follow-up. We cannot suggest specific diagnostic methods that identify CTRV joint problems among various overlapping anatomical structures, other than typical tenderness and related clinical manifestations. Therefore, a more controlled study is needed to determine the exact source of pain, such as a staged diagnostic block in the surrounding structures of the thoracic spine.
In conclusion, we demonstrated clinical improvements in thoracic back pain patients after a CTRV joint injection. Ultrasound-guided CTRV joint injections reduced patients' pain scores and led to a high level of satisfaction at short-term follow-up in patients with suspected CTRV joint-generated pain. The results of this study suggest that CTRV injection should be considered as a therapeutic option to solve complex problems of thoracic back pain in selected patients.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download