Abstract
Ilioinguinal and iliohypogastric (II/IH) nerve injury is one of the most common nerve injuries following pelvic surgery, especially with the Pfannenstiel incision. We present a case of intractable groin pain, successfully treated with a continuous II/IH nerve block. A 33-year-old woman, following emergency cesarean section due to cephalopelvic disproportion, presented numbness in left inguinal area and severe pain on the labia on the second postoperative day. The pain was burning, lancinating, and exacerbated by standing or movement. However, she didn't want to take additional medicine because of breast-feeding. A diagnostic II/IH nerve block produced a substantial decrease in pain. She underwent a continuous II/IH nerve block with a complete resolution of pain within 3 days. A continuous II/IH nerve block might be a goodoption for II/IH neuropathy with intractable groin pain in breast-feeding mothers without adverse drug reactions in their infants.
Go to : 
The ilioinguinal and iliohypogastric (II/IH) nerves are the cutaneous nerves of the lower abdomen and groin [1]. Injury to these nerves may often occur after a Pfannenstiel incision for pelvic surgery. II/IH neuropathy after major gynecologic surgery is the second most common neuropathy, reporting an incidence of 3.7% after Pfannenstiel incisions [23]. The most common surgery associated with inguinal neuralgia is herniorrhaphy, but it may also be seen after appendectomy, iliac crest graft harvesting, urological surgery, and gynecological surgery [4]. Medical treatment with antidepressants or anticonvulsive drugs is common [56]. However, the choice of medical treatment should be taken after a careful consideration of factors influencing the excretion of drugs into the breast milk and possible side-effects on the infant caused by the indirect exposure to drugs via breast milk. In addition, most breastfeeding mothers worry about taking such drugs during the postpartum period. We report a case of intractable groin pain after cesarean delivery, successfully treated with a continuous II/IH nerve block in a breastfeeding patient.
A 33-year-old female was transferred to the emergency department with severe groin pain after having emergency cesarean resection due to cephalopelvic disproportion 5 days earlier. She had burning, lancinating, and intermittent pain in the left groin region, especially the area of the superomedial thigh, the mons pubis, and labia majora. She sometimes felt numbness in the inguinal region. The pain was developed on the second postoperative day (POD) when she walked for exercise. It was getting worse over time. Symptoms were aggravated by standing, raising her leg, bending over, or walking. The pain did not occur when she lay on her back. She continued to stay in the bed due to intractable pain, even during urination or defecation. There was no sensory loss or muscle paralysis on the left lower extremity. There were also no sympathetic mediated symptoms, such as edema or sweating changes. The pain intensity was over 7 on the visual analogue scale (VAS). A diagnostic workup was performed to rule out occult inguinal hernia in the emergency department. There were no abnormal signs such as a bulging groin or silk glove sign on physical examination. Computed tomography (CT) of the pelvis showed no abnormal finding except an enlarged uterus. The patient was referred to the pain clinic when occult inguinal hernia was ruled out.
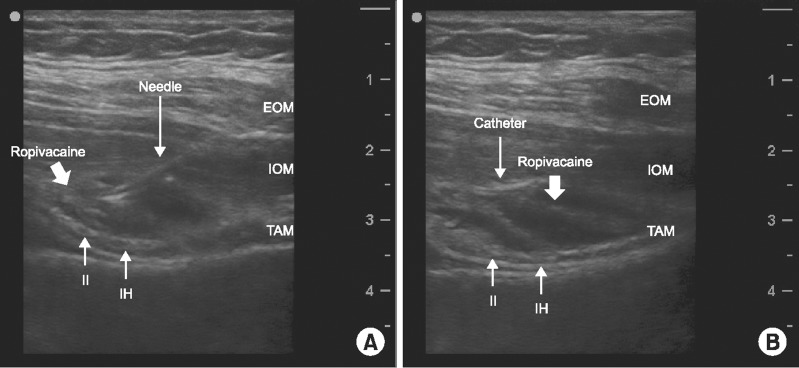
She worried about what would be happen to her baby when she took any treatments, especially medications, while breastfeeding. With a presumed diagnosis of ilioinguinal or genitofemoral neuralgia, a diagnostic block of the II/IH nerve using ultrasound was primarily performed immediately after breast-feeding for a differential diagnosis with the genitofemoral nerve and the correct treatment. Using an aseptic technique, an II/IH nerve block was performed under ultrasound guidance (6–13 MHz, S-nerve, SonositeInc, Bothell, WA, USA). The probe was placed on the left lower abdomen in transverse plane just above the anterior superior iliac spine (ASIS), and then slowly rotated from a transverse to an oblique plane to be perpendicular to the anatomical course of both nerves. The 3-muscle fascial layers of the external oblique (EO), internal oblique (IO), and transversus abdominis (TA) were identified, and a 20 G Tuohy epidural needle was inserted toward the round-shape hyperechoic structure between IO and TA. Complete circumferential spread of local anesthetic (LA) was achieved while 7 ml of mixed solution (0.2% ropivacaine 20 ml with dexamethasone 5 mg) was incrementally injected around the nerves. The VAS was immediately decreased from 7 to 2 after infiltration. The patient could stand or move freely, though the pain sometimes occurred. Additionally, she didn't complain of any problem in lactation. On POD 8, an ultrasound-guided continuous II/IH nerve block was performed using an epidural catheter set (Perifix® Filter set, B. Braun, Melsungen, Germany) in the same way (Fig. 1). A patient controlled analgesia (PCA) pump was used to deliver LA through a catheter for 3 days (basal infusion rate 5 ml/h, demand dose 5 ml, and lockout time 30 min). She had complete resolution of symptoms with the continuous nerve block. There were no adverse reactions such as sedation or behavior change in the breastfed infant during the perineural local anesthetic infusion. She was discharged without pain on POD 12. In outpatient follow-up, she didn't report recurrence of the pain.
Go to : 
The Pfannenstiel incision is a common cause of chronic pain after pelvic surgery such as cesarean deliveries and hysterectomies. One third of patients with the Pfannenstiel incision experience chronic pain at the incision site [34]. About 7% of patients complained of moderate to severe pain, and more than half of these patients had neuropathic pain around the incision site [4]. II/IH neuropathy may be caused by a direct transaction of the nerve from incision, nerve entrapment from sutures or ligation for bleeding control, tissue reapproximation, and neuroma. Although, there is a strong possibility of II/IH neuropathy considering the history of cesarean sections with the Pfannenstiel incision, due to the characteristics and area of pain in our case, occult hernia and genitofemoral neuropathy are important considerations in the differential diagnosis. Computed tomography (CT) can be a useful adjunct for the evaluation of patients presenting with undiagnosed groin pain. Garvey [7] found that a CT diagnosis for hernia had a positive predictive value of 92% and a negative predictive value of 96%. In this case, occult hernia could be ruled out, because there were no abnormal findings such as bulging along the pubic or groin area on physical examination and CT. Genitofemoral neuropathy presents with pain in a similar area as that supplied by the II/IH nerves. Differential diagnosis with genitofemoral neuropathy is challenging, but it is mandatory for correct treatment. In this case, the ultrasound guided nerve block with LA and a steroid was performed for confirmation of diagnosis and as a therapeutic method.
The optimal treatment for II/IH neuropathy is not clear. Treatments include medication with antidepressants and anticonvulsants, nerve blocks with or without a steroid, and surgical intervention [568]. Hahn [5] reported that surgical intervention is superior to medical treatment of II/IH nerve entrapment. But, conservative therapy should always be the first line of treatment. Palumbo et al. [9] recommended that noninvasive methods are to be preferred, whereas, neurectomy should be reserved for intractable cases. Ultrasound-guided nerve blocks combining a steroid with LA can be useful for accurate diagnosis and effective treatment in patients with inguinal neuralgia [8]. Gucev et al. [10] reported bilateral continuous II/IH block with 0.2% ropivacaine (infusion rate 4 ml/h) resulted in satisfactory analgesia after cesarean section. In our case, the II/IH nerve could be identified above ASIS between TA and IO and a perineural catheter was placed close to both nerves. Therefore, 7 ml of LA was sufficient to perform the nerve block compared with the transversus abdominis plane block with 20 ml of LA. And it might be enough to achieve good analgesia with a 5 ml/h of infusion rate.
Breast-feeding mothers are reluctant to consider medical treatment with antidepressants and anticonvulsants that are commonly used to treat neuropathic pain. Although adverse drug reactions (ADRs) via breast-feeding are rarely reported, CNS drugs such as antiepileptic drugs, opioids, and benzodiazepine were implicated in more than a third of all cases of ADRs in breastfed infants [11]. Gabapentin passes into breast milk (milk-to-plasma ratio 0.7–1.3) and pregabalin has an excellent oral bioavailability (90%) [12]. Considering pharmacokinetic parameters associated with lactation risk, breastfed infants should be carefully monitored with ADRs related to the neurological and gastrointestinal systems. Most of antidepressants also pass readily into breast milk. However, available data about infant serum levels showed low or undetectable plasma levels with tricyclics or SSRIs and there are no reports of ADRs [13]. It could be compatible with breast-feeding, but routine clinical monitoring of breastfed infants should be instituted. Ropivacaine has advantageous pharmacokinetic characteristics for lactation risk. It has the lowest milk-plasma ratio (0.23 ± 0.07 at 24 hr) and higher maternal plasma protein binding (95%) compared to lidocaine and bupivacaine [14]. In this case, we performed a diagnostic II/IH nerve block with ropivacaine and dexamethasone. Effective treatment could be achieved using a continuous nerve block without any medication for neuropathic pain. Dexamethasone is thought to pass through breast milk like other corticosteroids. But, no specific studies or reports have been done on the effects in breastfed infants. However, the use of glucocorticoid can cause a temporary decrease of milk production in nursing mothers. Babwah et al. [15] reported a case of temporary suppression of lactation with a nursing mother who was given local corticosteroid for treatment of tenosynovitis. In this case, we first performed a diagnostic II/IH nerve block with ropivacaine and dexamethasone. Effective treatment could be achieved using a continuous nerve block without any medication for treatment of neuropathic pain. There was no adverse drug reaction associated with ropivacaine in the infant and no reduction of lactation related to the steroid in the nursing mother.
In conclusion, ultrasound-guided continuous II/IH nerve blocks might be a good option for II/IH neuropathy with intractable groin pain in breast-feeding mothers who worry about adverse drug reactions in breastfed infants, during the postpartum period.
Go to : 
ACKNOWLEDGEMENTS
This work was supported by clinical research grant from Pusan National University Hospital 2014.
Go to : 
References
1. Rahn DD, Phelan JN, Roshanravan SM, White AB, Corton MM. Anterior abdominal wall nerve and vessel anatomy: clinical implications for gynecologic surgery. Am J Obstet Gynecol. 2010; 202:234.e1–234.e5. PMID: 20022582.

2. Cardosi RJ, Cox CS, Hoffman MS. Postoperative neuropathies after major pelvic surgery. Obstet Gynecol. 2002; 100:240–244. PMID: 12151144.

3. Luijendijk RW, Jeekel J, Storm RK, Schutte PJ, Hop WC, Drogendijk AC, et al. The low transverse Pfannenstiel incision and the prevalence of incisional hernia and nerve entrapment. Ann Surg. 1997; 225:365–369. PMID: 9114794.

4. Loos MJ, Scheltinga MR, Mulders LG, Roumen RM. The Pfannenstiel incision as a source of chronic pain. Obstet Gynecol. 2008; 111:839–846. PMID: 18378742.

5. Hahn L. Treatment of ilioinguinal nerve entrapment - a randomized controlled trial. Acta Obstet Gynecol Scand. 2011; 90:955–960. PMID: 21615360.

6. Benito-Léon J, Picardo A, Garrido A, Cuberes R. Gabapentin therapy for genitofemoral and ilioinguinal neuralgia. J Neurol. 2001; 248:907–908. PMID: 11697532.

7. Garvey JF. Computed tomography scan diagnosis of occult groin hernia. Hernia. 2012; 16:307–314. PMID: 22167621.

8. Leem JG. Ultrasound-guided nerve blocks for post-hernia repair pain. Korean J Pain. 2010; 23:227–229. PMID: 21217884.

9. Palumbo P, Minicucci A, Nasti AG, Simonelli I, Vietri F, Angelici AM. Treatment for persistent chronic neuralgia after inguinal hernioplasty. Hernia. 2007; 11:527–531. PMID: 17668147.

10. Gucev G, Yasui GM, Chang TY, Lee J. Bilateral ultrasound-guided continuous ilioinguinal-iliohypogastric block for pain relief after cesarean delivery. Anesth Analg. 2008; 106:1220–1222. PMID: 18349197.

11. Soussan C, Gouraud A, Portolan G, Jean-Pastor MJ, Pecriaux C, Montastruc JL, et al. Drug-induced adverse reactions via breastfeeding: a descriptive study in the French Pharmacovigilance Database. Eur J Clin Pharmacol. 2014; 70:1361–1366. PMID: 25183382.

12. Davanzo R, Dal Bo S, Bua J, Copertino M, Zanelli E, Matarazzo L. Antiepileptic drugs and breastfeeding. Ital J Pediatr. 2013; 39:50. PMID: 23985170.

13. Lanza di Scalea T, Wisner KL. Antidepressant medication use during breastfeeding. Clin Obstet Gynecol. 2009; 52:483–497. PMID: 19661763.

14. Matsota PK, Markantonis SL, Fousteri MZ, Pandazi AK, Manikis DE, Christodoulopoulou TC, et al. Excretion of ropivacaine in breast milk during patient-controlled epidural analgesia after cesarean delivery. Reg Anesth Pain Med. 2009; 34:126–129. PMID: 19282712.

15. Babwah TJ, Nunes P, Maharaj RG. An unexpected temporary suppression of lactation after a local corticosteroid injection for tenosynovitis. Eur J Gen Pract. 2013; 19:248–250. PMID: 24261425.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download