INTRODUCTION
Regional anesthesia and analgesia have obtained much attention. Interscalene brachial plexus block (IBPB) has been widely implemented in shoulder, clavicle, and humerus surgery for perioperative or chronic pain management. In Korea, ever since the National Health Service of continuous IBPB for shoulder and humerus fracture surgery was permitted, the number of such intervention has been increased.
Techniques for IBPB have been developed, ranging from landmark techniques to nerve stimulator (NS) techniques and ultrasound (US) guidance. Recently, US have been commonly used. Many anesthesiologists and orthopedic surgeons can perform US-guided IBPB relatively more safe and accurate compared to previous intervention method. However, the risk of nerve injuries still remains. When performing US-guided IBPB, in-plane approach is the mostly used one on short-axis view. Posterior approach is more commonly used because there have been reports that anterior approach has the risk of causing phrenic nerve injury [
12]. However, the physicians need to be cautious about some nerves, namely dorsal scapular nerve (DSN) and long thoracic nerve (LTN), in posterior approach [
2]. US-guided IBPB by posterior approach has the risk of causing nerve injury because there are risks of encountering DSN and LTN. Even though there is a possibility of complications mentioned above, an anatomical relative position of DSN and LTN remains unknown. Therefore, the objective of this study was to determine the probability of encountering DSN and LTN in US-guided IBPB with nerve stimulator using the posterior approach.
Go to :

MATERIALS AND METHODS
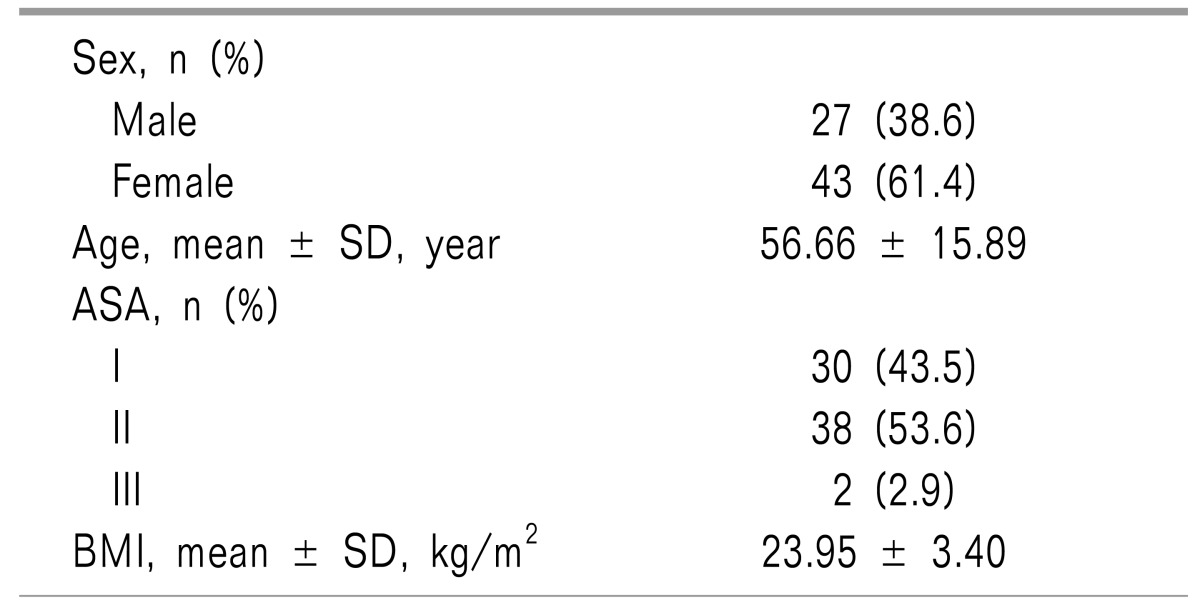
Institutional Review Board of the Hospital approved this study. Written informed consent was obtained from patients about the study during pre-anesthetic visitation. Seventy patients who were scheduled for shoulder surgery at class I-III American Society of Anesthesiologists (ASA) status were enrolled in this study. Patients who were 20 years of age or younger, pregnant, with localized infection, severe coagulopathy, neuromuscular disorders, or having history of allergy with local anesthetics were excluded. In addition, cases that the needle entry site was changed due to muscle twitches occurred as soon as the needle touched the patient's skin were also excluded.
After deciding the insertion site with ultrasound, dual- guided (US and NS-guided) IBPB was performed with patients in supine position with the patient's head facing away from the side to be blocked. The skin was disinfected. Ultrasound probe and cable were protected with a sterile ultrasound probe cover (Sono Lab
TM 18 × 120 cm, Lucky Medical, Korea). Transportable ultrasound equipment with a 38 mm linear 6-13 MHz probe (SonoSite M-Turbo
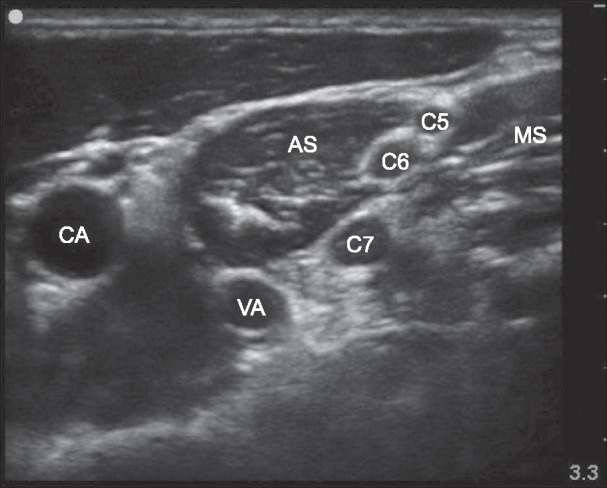
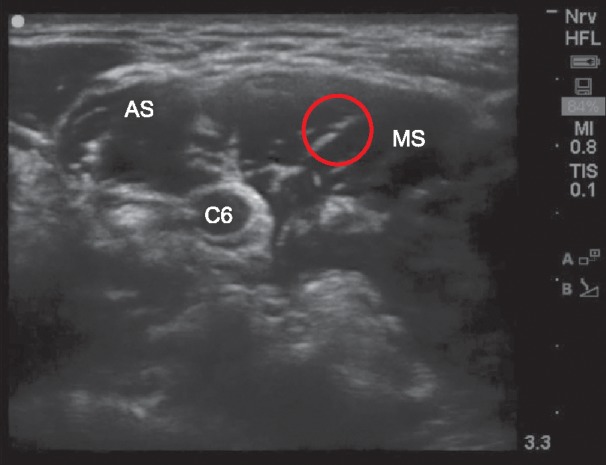
TM, SonoSite Inc., Bothell, WA, USA) was used. The probe was positioned in the transverse plane to identify the carotid artery. Once the artery was identified, the probe was moved slightly laterally across the neck. The probe was then moved cranially and caudally. Dorsal scapular or long thoracic nerves was identified within or superficial to the middle scalene muscle. The goal was to identify the scalene muscles and the brachial plexus that was sandwiched between that anterior and middle scalene muscles just below the level of transverse process of 7th cervical vertebra (
Fig. 1). A 22G stimulating needle (Stimuplex® D, B.Braun, Germany) was then inserted in-plane toward the brachial plexus in a posterior-to-anterior direction. Current was slowly decreased from 2.0 mA to 0.1 mA by 0.1 mA interval until a muscle twitch was disappeared. Stimulator pulse width was 0.1 ms with a frequency of 2 Hz. During the stimulation, direct palpation of the serratus anterior, rhomboids, and levator scapulae were used to confirm the muscle twitch.
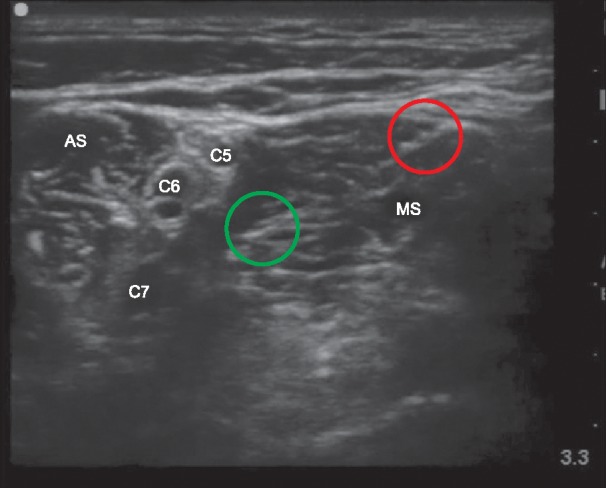
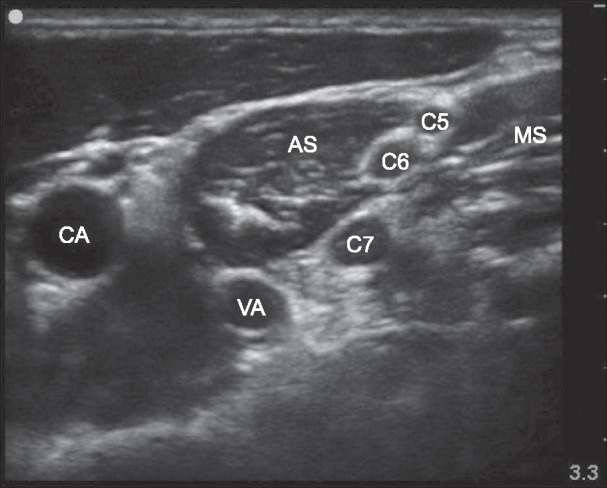 | Fig. 1Ultrasound image of the site of interscalene brachial plexus block. CA: carotid artery, VA: vertebral artery, AS: anterior scalene muscle, MS: middle scalene muscle, C5: 5th cervical root, C6: 6th cervical root, C7: 7th cervical root.
|
We investigated the incidence of muscle twitches stimulated DSN (levator scapulae muscle and rhomboids) and LTN (serratus anterior muscle) as well as the current intensity immediately before the disappearance of muscle twitches. We then withdrew the needle, changed the direction of needle, and performed IBPB. The needle passed through the middle scalene and then headed toward the brachial plexus. Although DSN and LTN were observed on the screen, we did not intentionally direct the needle toward those nerves or change its direction when the needle was not headed toward the correct direction for BPB. The study was ended when the needle reached at the brachial plexus and IBPB was achieved.
Go to :

DISCUSSION
Regional anesthesia has been widely used for intraoperative and postoperative pain management in shoulder, clavicle, and humerus surgery. IBPB is often used as one regional anesthesia method. However, complications can occur in the interscalene region where important anatomical structures are gathered.
In USA, according to ASA claims database, the most common complications associated with PNB claims since 1999 is nerve injury [
3]. Brachial plexus (38%) is the most frequently injured nerve, followed by median (21%), ulnar (16%), spinal cord (8%), and phrenic nerve (8%). The most common block related to nerve injury is interscalene block [
3]. Also in Korea, nerve injury related to PNB was 23% of total cases with the medical dispute cases [
4]. These results highlight the importance of physician's cautions on nerve injury.
Due to this risk of nerve injury, IBPB is performed under US observation of structures and needle location in recent years. US-guided IBPB by posterior approach is generally used to prevent phrenic nerve injury [
5]. However, the operator also needs to be cautious about some nerves, namely DSN and LTN, during this approach.
DSN is mainly derived from the 5th cervical nerve root. It leads to motor innervation of levator scapulae muscle and rhomboid muscle (
Fig. 3). DSN runs down and passes through the middle scalene muscle located an average of nearly 3 cm (1.8−4.5 cm) from the cervical spine, the origin of DSN [
67]. When injured by the needle approach, DSN syndrome as one chronic pain syndrome can occur. It is characterized with pain along the medial border of scapula that radiates to the lateral surface of upper extremities and causes weakness of the rhomboid and/or levator scapulae muscles [
8]. Patients with DSN syndrome usually complain of a not-well-defined shoulder pain and dysfunction with different degrees of functional impairment. In this study, the needle encountered DSN in the middle scalene muscle.
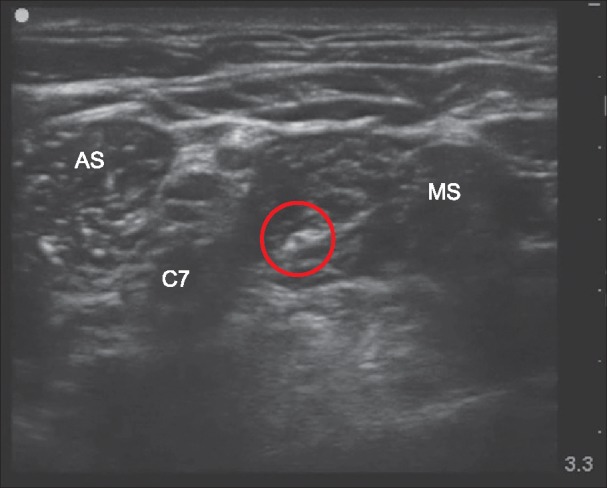
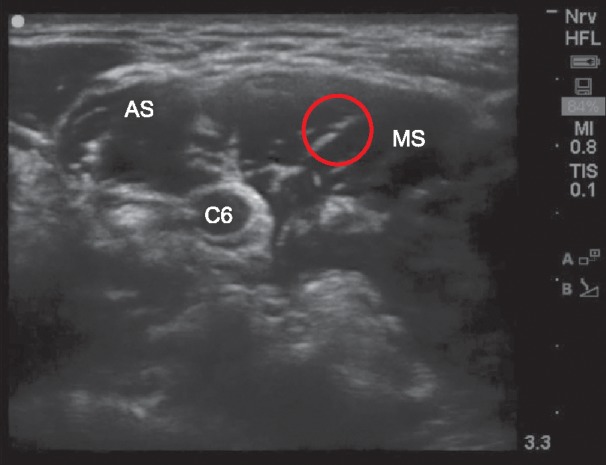 | Fig. 3Ultrasound image of dorsal scapular nerve. It derives from C5 nerve root. AS: anterior scalene muscle, MS: middle scalene muscle, Red circle: dorsal scapular nerve, C6: 6th cervical root.
|
The LTN arises from the anterior branches of the 5th, 6th, and 7th cervical nerve roots. It rarely (8%) arises from the 8th cervical nerve root (
Fig. 4) [
9]. This nerve innervates the serratus anterior muscle. However, it does not contribute to cutaneous innervation. It has been report that the 5th and 6th cervical roots can pierce the middle scalene muscle, combine with each other, and finally merge with the 7th cervical nerve root [
9]. It runs within or next to the middle scalene muscle often in close proximity of the DSN. LTN also can be encountered during IBPB by the posterior approach which can cause nerve injury. Injury to LTN actually has been reported [
10]. In addition, LTN syndrome may be caused by LTN injury. LTN syndrome is a chronic pain syndrome of the shoulder associated with different degree of serratus anterior muscle palsy, the impairment of shoulder elevation, and a characteristic scapula winging with medial translation and rotation of the inferior angle towards the midline. In this study, the needle encountered LTN in the middle scalene muscle.
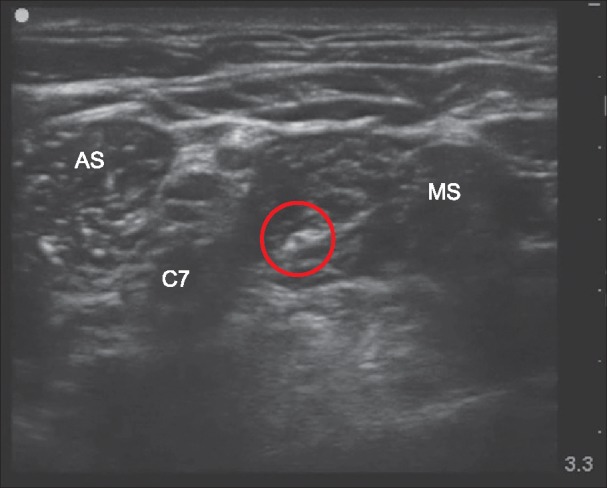 | Fig. 4Ultrasound image of long thoracic nerve. It arises from the anterior branches of the 6th cervical nerve root. AS: anterior scalene muscle, MS: middle scalene muscle, Red circle: long thoracic nerve, C7: 7th cervical root.
|
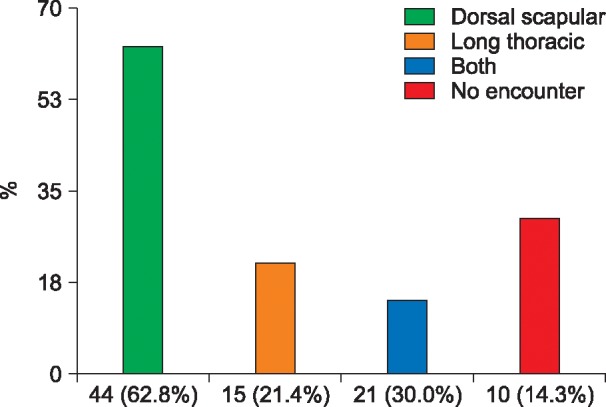
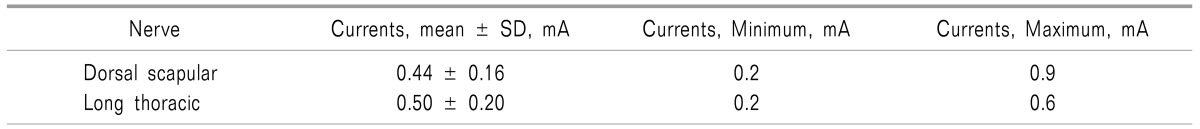
As a result of this study, DSN, LTN, both nervers, and neither nerves were encountered in 44 (62.8%), 15 (21.4%), 10 (14.3%), and 21 (30.4%) cases, respectively (
Fig. 2). Hanson and Auyong [
11] have studied about this previously. They identified DSN and LTN in 77% and 23% of 50 cases, respectively. This study is different from their study in the following respects. First, they found the nerves using US and then confirmed the motor response by stimulation. On the other hand, we confirmed the motor response during US-guided IBPB as usual. Second, they confirmed motor response by approaching the needle to identified nerves. However, we did not intentionally change the needle direction, although we identified the nerves before. In the cases that neither DSN nor LTN was encountered, the nerves already passed by the needle path and went to the cephalad or caudal direction (
Fig. 5). Lastly, they reported that the average of stimulation currents was 1.28 mA. On the other hand, this study verified that the stimulation currents of DSN and LTN were 0.44 mA and 0.50 mA, respectively. Currently it is unknown why the stimulation currents in the two studies had such big difference. However, the risk of encountering nerves can be avoidable if the stimulation currents is started with 1.5 mA.
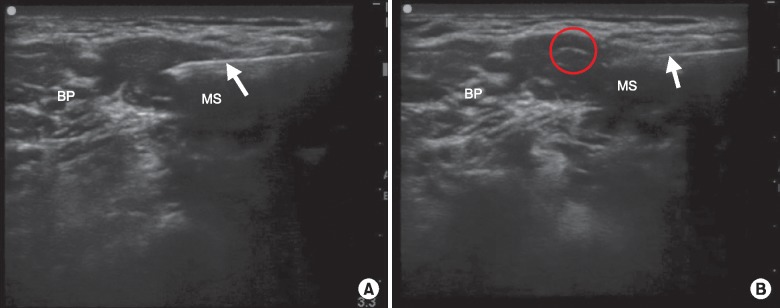
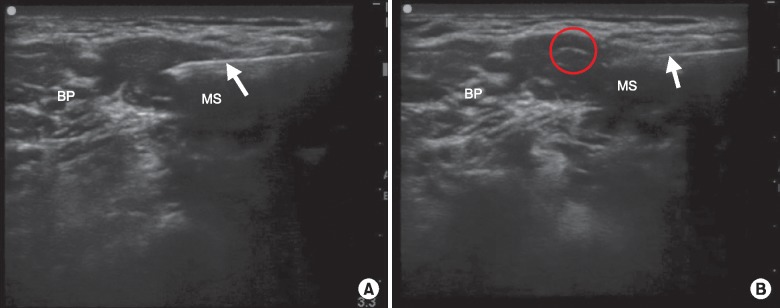 | Fig. 5Ultrasound image of dual-guided interscalene brachial plexus block (A) and just cephalad image of A (B). Dorsal scapular nerve and long thoracic nerve are not seen (A). Dorsal scapular nerve is seen. It already passed and went to the cephalad direction of needle path (B). BP: brachial plexus, MS: middle scalene muscle, Red circle: dorsal scapular nerve, Arrow: needle.
|
In conclusion, we believe that it will be safer to carefully check anatomical structures, including DSN and LTN (
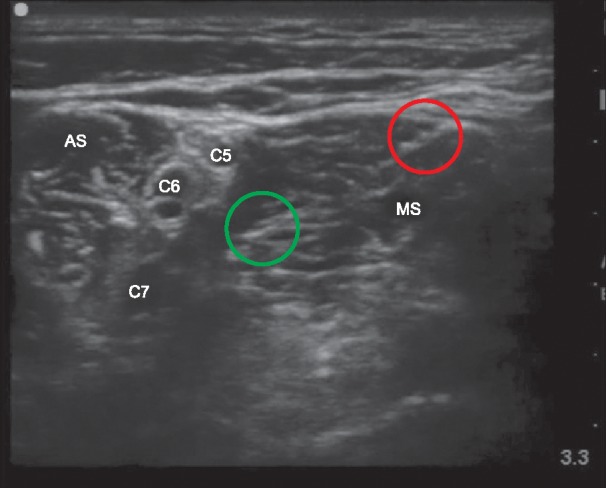
Fig. 6). If possible, NS should be used during US-guided IBPB with the posterior approach. If a motor response is present, it is considered to be safe to deflect the needle from its path and find another one. If this is performed under general anesthesia with hypoechoic ovale or hyperechoic linea images in the needle plane, it is recommended to avoid it instead of piercing it. If the US technology is more developed and its images are clearer, these risks can be identified and managed more readily.
 | Fig. 6Ultrasound image of dorsal scapular nerve and long thoracic nerve at the site of interscalene brachial plexus block. Dorsal scapular nerve and long thoracic nerve are seen in the middle scalene muscle. AS: anterior scalene muscle, MS: middle scalene muscle, Red circle: dorsal scapular nerve, Green circle: long thoracic nerve, C5: 5th cervical root, C6: 6th cervical root, C7: 7th cervical root.
|
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download